Arteriosclerosis / Atherosclerosis Symptoms: Arteriosclerosis and atherosclerosis are often used interchangeably, but they are not the same condition.
Arteriosclerosis is a general term for the thickening and hardening of arteries, whereas atherosclerosis is a specific type of arteriosclerosis related to plaque buildup in the walls of arteries.
Understanding the symptoms, causes, and differences between these conditions is crucial for early detection and management.
Understanding Arteriosclerosis and Atherosclerosis
Arteriosclerosis and atherosclerosis are two terms often used interchangeably, but they have distinct meanings and implications for heart health. This article aims to clarify these conditions, highlight their differences and similarities, and underscore their significance in contemporary health discussions.
Defining Arteriosclerosis and Atherosclerosis
Arteriosclerosis refers to the general hardening and thickening of the arteries. This broad term encompasses a range of conditions that cause arterial walls to become stiffer, often due to aging or disease. Arteriosclerosis affects blood flow and can increase the risk of heart complications.
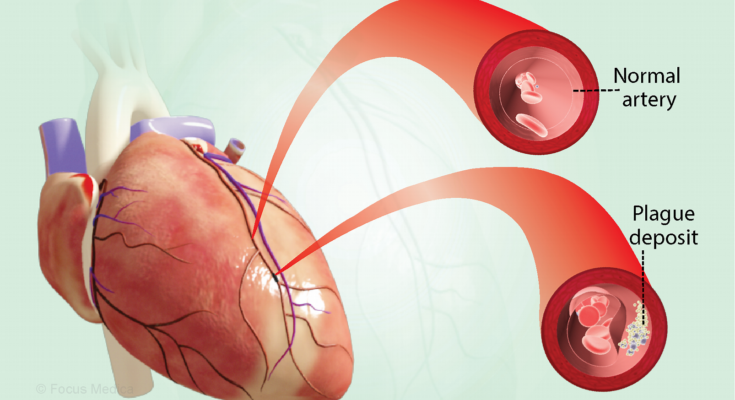
Atherosclerosis, a subtype of arteriosclerosis, specifically involves the buildup of plaques – a mixture of fats, cholesterol, and other substances – inside the artery walls. These plaques can restrict blood flow or rupture, leading to serious heart-related issues, including heart attacks and strokes.
Differences and Similarities Between the Conditions
While both conditions impact the arteries, their differences lie in their specific processes and consequences:
- Arteriosclerosis is a broad term for artery hardening, irrespective of the underlying cause.
- Atherosclerosis specifically involves the buildup of plaques within the arterial walls.
The similarities between these conditions include:
- Both affect arterial health and can lead to reduced blood flow.
- They share risk factors such as high blood pressure, high cholesterol, and smoking.
- Both conditions can lead to severe cardiovascular diseases if not managed properly.
Statistics and Relevance in Modern Health
These diseases hold significant relevance in today’s health landscape. According to recent statistics:
- Atherosclerosis is a leading cause of heart disease and strokes, which are among the top causes of death globally.
- Lifestyle factors, such as diet, exercise, and tobacco use, significantly influence the prevalence and severity of these conditions.
Understanding arteriosclerosis and atherosclerosis is crucial for preventing and managing heart disease. Awareness of these conditions, their differences, and impacts, is vital for individuals and healthcare professionals alike in our ongoing battle against heart-related illnesses.
Causes of Arteriosclerosis and Atherosclerosis
Arteriosclerosis and atherosclerosis, often used interchangeably, are conditions affecting the arteries, leading to serious health complications. Understanding their causes is crucial for prevention and management. This section delves into the primary causes of these conditions, providing a detailed exploration of each.
Lifestyle Factors
A key contributor to arteriosclerosis and atherosclerosis is lifestyle. The choices we make daily significantly impact our artery health.
- Diet: A diet high in saturated fats, trans fats, and cholesterol can lead to the buildup of plaque in the arteries. Conversely, a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help prevent these conditions.
- Exercise: Regular physical activity helps maintain a healthy weight and reduces artery-damaging inflammation.
- Smoking: Tobacco smoke is a major risk factor. It damages the lining of the arteries and contributes to the buildup of plaque.
- Alcohol Consumption: Excessive alcohol intake can lead to high blood pressure, a risk factor for arteriosclerosis.
Genetic Predispositions
Genetics also plays a role. Some individuals are genetically predisposed to higher levels of cholesterol, which can contribute to plaque buildup. Family history of early heart disease is another indicator of higher risk.
Other Contributing Health Conditions
Several health conditions can exacerbate the risk of developing arteriosclerosis and atherosclerosis:
- High Blood Pressure (Hypertension): This condition can damage arteries over time, making them more susceptible to atherosclerosis.
- High Cholesterol: Elevated levels of low-density lipoprotein (LDL) cholesterol, often termed “bad cholesterol,” can lead to plaque buildup.
- Diabetes: Poorly controlled diabetes accelerates the hardening and narrowing of arteries.
Understanding these causes is vital for anyone looking to maintain healthy arteries. Lifestyle adjustments, awareness of genetic factors, and managing other health conditions are essential steps in preventing arteriosclerosis and atherosclerosis.
Common Symptoms of Arteriosclerosis and Atherosclerosis
This guide outlines the common symptoms associated with each stage of these conditions, helping you stay informed about your cardiovascular health.
Early-Stage Symptoms
- Mild Chest Pain or Angina: In the early stages of these conditions, you might experience occasional chest pain or discomfort, often triggered by physical activity or stress.
- Shortness of Breath: Difficulty in breathing during routine activities could be an early warning sign.
- Fatigue: Unexplained tiredness or fatigue, especially after physical exertion, is a common early symptom.
- Leg Pain During Exercise: Known as claudication, this symptom involves muscle pain or cramping in the legs or arms induced by activity.
Advanced-Stage Symptoms
- Severe Chest Pain: As the condition progresses, chest pain may become more frequent and severe.
- Numbness or Weakness: Advanced stages may lead to numbness or weakness in your arms or legs, indicating reduced blood flow.
- Difficulty Speaking or Slurred Speech: This could signal a cerebrovascular event like a stroke, caused by reduced blood flow to the brain.
- Sudden, Severe Headache: A severe, unexplained headache can be a warning sign of a stroke due to either arteriosclerosis or atherosclerosis.
Differences in Symptoms Between Arteriosclerosis and Atherosclerosis
- Arteriosclerosis: This refers to the general hardening and thickening of the arteries. The symptoms are more generalized, such as high blood pressure and reduced blood flow to different parts of the body.
- Atherosclerosis: A type of arteriosclerosis, it specifically involves the build-up of plaques in the artery walls. Symptoms are often more specific, like chest pain (angina), heart attacks, or strokes, depending on which arteries are affected.
However, recognizing these symptoms can be a lifesaver. Early detection and intervention can significantly reduce the risk of severe cardiovascular events associated with arteriosclerosis and atherosclerosis. If you experience any of these symptoms, consulting a healthcare professional is essential for proper diagnosis and treatment.
Diagnosing Arteriosclerosis and Atherosclerosis
Methods Used in Diagnosis
Recognizing these conditions early is pivotal for effective management and treatment. Here, we delve into the commonly employed methods for diagnosing both arteriosclerosis and atherosclerosis.
- Physical Examination: Initially, healthcare professionals conduct a thorough physical examination. This includes checking for weakened pulse, decreased blood pressure in the affected limbs, and listening for abnormal sounds in the arteries.
- Blood Tests: These tests help in assessing cholesterol levels, triglycerides, and other substances in the blood that may contribute to arteriosclerosis.
- Doppler Ultrasound: This non-invasive method uses sound waves to visualize blood flow and can detect abnormal flow within the arteries, suggesting the presence of blockages.
- Angiography: By injecting a contrast dye into the arteries, angiography provides detailed images of the inside of the arteries, revealing areas of blockage or narrowing.
- CT Scans and MRI: These imaging techniques offer cross-sectional images of the arteries, helping in identifying hardened and narrowed areas.
- Ankle-Brachial Index: This simple test compares the blood pressure in the ankle with the blood pressure in the arm to gauge blood flow and detect narrowing of arteries.
Importance of Early Diagnosis
Early diagnosis of arteriosclerosis and atherosclerosis is critical. These conditions, if left unchecked, can lead to serious complications like heart attacks, stroke, and peripheral artery disease. Early detection:
- Prevents Progression: Identifying the disease early can help in implementing lifestyle changes and treatments that can slow or even stop the progression.
- Reduces Risk of Complications: Timely diagnosis reduces the risk of severe complications by allowing for early intervention.
- Improves Quality of Life: Early management of these conditions can significantly improve the quality of life, reducing symptoms like pain, fatigue, and mobility issues.
- Enhances Treatment Efficacy: Treatments are often more effective when initiated early, as the disease is less advanced and more responsive to both medical and lifestyle interventions.
However, employing a combination of physical examinations, blood tests, imaging techniques, and specialized tests is essential for accurately diagnosing arteriosclerosis and atherosclerosis. Understanding the importance of early diagnosis is crucial for preventing complications and maintaining a healthy, active lifestyle. Regular check-ups and being aware of the risk factors can greatly assist in early detection and effective management of these cardiovascular conditions.
Risk Factors and Prevention of Arteriosclerosis and Atherosclerosis
It’s essential to understand the risk factors associated with them to implement effective prevention strategies.
- Age and Gender: Age is a primary risk factor; these conditions are more common as people get older. Also, men are generally at a higher risk than women, although the risk for women increases after menopause.
- Unhealthy Diet: A diet high in saturated fats, trans fats, cholesterol, and sodium can contribute to the development of plaque in the arteries, leading to these conditions.
- High Blood Pressure: Consistently high blood pressure can cause arteries to harden and narrow, increasing the risk.
- High Cholesterol Levels: High levels of bad cholesterol (LDL) and low levels of good cholesterol (HDL) contribute to the formation of plaque.
- Lifestyle Factors: Smoking, physical inactivity, and obesity are significant contributors. Smoking, in particular, damages blood vessels and can accelerate arterial diseases.
- Diabetes: Diabetes significantly increases the risk as it alters the way the body uses blood fats.
- Family History: A family history of heart disease can increase your risk, indicating a possible genetic predisposition.
Preventative Measures and Lifestyle Changes
Prevention plays a crucial role in combating arteriosclerosis and atherosclerosis. Here are some effective strategies:
- Healthy Diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean proteins. Reduce intake of saturated fats, trans fats, and cholesterol.
- Regular Exercise: Engage in at least 150 minutes of moderate aerobic exercise or 75 minutes of vigorous exercise each week.
- Maintain Healthy Weight: Achieving and maintaining a healthy weight can significantly reduce the risk.
- Quit Smoking: Stopping smoking can improve arterial health and reduce risk factors.
- Manage Blood Pressure and Cholesterol: Regular health check-ups to monitor blood pressure and cholesterol levels are crucial. Follow prescribed treatments if necessary.
- Diabetes Management: Effective management of diabetes can lower the risk of arterial diseases.
- Stress Management: Reducing stress through techniques like meditation, yoga, or other relaxation methods can benefit heart health.
Incorporating these lifestyle changes and being aware of the risk factors can significantly reduce the risk of arteriosclerosis and atherosclerosis. Remember, it’s never too late to start making healthier choices.
Treatment Options for Arteriosclerosis and Atherosclerosis
Treatment options can be broadly categorized into medical treatments, such as medications and surgical procedures, and lifestyle modifications.
Medical Treatments (Medication, Surgery, etc.)
- Medications: Key to managing arteriosclerosis and atherosclerosis, medications include cholesterol-lowering drugs (like statins), antihypertensive drugs to control blood pressure, and antiplatelet agents to prevent blood clots.
- Surgical Procedures: In severe cases, surgical interventions become necessary. Angioplasty, where a balloon is used to open narrowed arteries, and bypass surgery, where blood flow is rerouted around a blocked artery, are common procedures. Stent placement is also a frequent treatment to keep arteries open.
Lifestyle Modifications as Treatment
- Dietary Changes: A heart-healthy diet, low in saturated fats, cholesterol, and sodium, and rich in fruits, vegetables, and whole grains is vital.
- Regular Physical Activity: Regular exercise helps improve heart health and manage weight, which is crucial in controlling arteriosclerosis.
- Smoking Cessation: Smoking is a major risk factor for arteriosclerosis and stopping it is a critical component of treatment.
- Stress Management: Chronic stress can contribute to artery damage and managing stress through techniques like meditation, yoga, or counseling is beneficial.
- Weight Management: Being overweight contributes to the development of arteriosclerosis, thus, maintaining a healthy weight is essential.
However, treating arteriosclerosis and atherosclerosis requires a combination of medical interventions and significant lifestyle changes. It’s important for patients to work closely with their healthcare providers to determine the most effective treatment plan for their individual needs.
Complications of Untreated Arteriosclerosis and Atherosclerosis
Potential Health Complications
Arteriosclerosis and atherosclerosis, if left untreated, can lead to severe and life-threatening complications. Here’s an overview of the risks associated with these conditions:
- Heart Attacks: Atherosclerosis can cause the arteries that supply blood to the heart to become narrow and hardened. This can lead to a blockage, causing a heart attack. Symptoms include chest pain, shortness of breath, and in severe cases, collapse.
- Stroke: Arteriosclerosis in the arteries supplying the brain can result in a stroke. A stroke occurs when the blood supply to part of the brain is interrupted, leading to potentially permanent damage to brain tissue.
- Peripheral Artery Disease (PAD): This condition, stemming from atherosclerosis, affects the blood vessels outside the heart and brain. It predominantly impacts the legs, causing pain and cramping during walking.
- Kidney Disease: The renal arteries, which supply blood to the kidneys, can be affected by atherosclerosis, potentially leading to chronic kidney disease.
- Aneurysms: Atherosclerosis can weaken the walls of arteries, leading to the formation of aneurysms. These are bulges in the artery walls that can burst, causing life-threatening internal bleeding.
Importance of Management and Treatment
Proactively managing and treating arteriosclerosis and atherosclerosis is crucial for several reasons:
- Preventing Complications: Effective treatment can significantly reduce the risk of heart attacks, strokes, and other severe complications.
- Improving Quality of Life: By managing these conditions, symptoms like pain and fatigue can be alleviated, enhancing daily life.
- Longevity: Timely treatment and management can extend life expectancy by preventing potentially fatal complications.
- Overall Health: Treating these conditions often involves lifestyle changes that can improve overall health, such as diet, exercise, and smoking cessation.
However, understanding the potential complications of untreated arteriosclerosis and atherosclerosis underscores the importance of early detection, continuous management, and treatment. Regular check-ups and following a treatment plan prescribed by a healthcare professional can significantly mitigate these risks.
Living with Arteriosclerosis and Atherosclerosis
Living with arteriosclerosis and atherosclerosis can be challenging, but with the right approach, you can manage symptoms effectively and maintain a good quality of life. Here are some tips to help you navigate daily life with these conditions:
Healthy Diet: A heart-healthy diet is crucial. Focus on eating plenty of fruits, vegetables, whole grains, and lean proteins. Limit intake of saturated fats, trans fats, cholesterol, salt (sodium), and added sugars. Consider a Mediterranean-style diet, which has been shown to be beneficial for heart health.
Regular Exercise: Engage in regular physical activity, such as walking, swimming, or cycling. Aim for at least 30 minutes of moderate exercise most days of the week. Always consult with your doctor before starting any new exercise regimen.
Maintain a Healthy Weight: If you’re overweight, losing even a small amount of weight can significantly reduce the strain on your heart. Work with a dietitian or a healthcare provider to create a weight loss plan that’s right for you.
Quit Smoking: Smoking is a major risk factor for both arteriosclerosis and atherosclerosis. Quitting smoking can dramatically reduce your risk of heart disease and improve your overall health.
Manage Stress: Chronic stress can negatively impact your heart health. Practice stress-reducing techniques such as deep breathing, meditation, yoga, or tai chi.
Regular Health Check-Ups: Stay on top of your health by scheduling regular check-ups with your doctor. Keep track of your blood pressure, cholesterol levels, and other relevant health indicators.
Medication Adherence: If you’re prescribed medication to manage your condition, take it as directed. Do not skip doses or stop taking medication without consulting your doctor.
Educate Yourself: Learn as much as you can about arteriosclerosis and atherosclerosis. Understanding your condition can empower you to make informed decisions about your health.
Stay Hydrated: Drinking plenty of water is good for your overall health and can help your blood circulate more easily.
Social Support: Don’t underestimate the power of emotional support. Stay connected with family and friends, and consider joining a support group for people with heart conditions.
Remember, living with arteriosclerosis and atherosclerosis requires a proactive approach to health. These tips can help you manage your symptoms and maintain a high quality of life. Always consult with your healthcare provider for personalized advice and treatment plans.
FAQs: Understanding Arteriosclerosis and Atherosclerosis
1. What is the difference between arteriosclerosis and atherosclerosis?
Arteriosclerosis is a broad term referring to the hardening and loss of elasticity of arteries. It can be caused by various conditions, including age-related changes.
Atherosclerosis, a subtype of arteriosclerosis, specifically involves the buildup of fats, cholesterol, and other substances in and on the artery walls, leading to narrowed and obstructed arteries.
2. What are the symptoms of arteriosclerosis and atherosclerosis?
Both conditions can initially be asymptomatic. However, as they progress, symptoms such as chest pain, shortness of breath, numbness or weakness in limbs, and high blood pressure may appear, depending on the affected arteries.
3. Who is at risk of developing these conditions?
Risk factors include aging, high cholesterol, high blood pressure, smoking, diabetes, obesity, a sedentary lifestyle, and a family history of heart disease.
4. How are arteriosclerosis and atherosclerosis diagnosed?
Diagnosis may involve physical exams, blood tests, EKGs, stress tests, angiograms, or other imaging tests like CT scans or MRIs to check for signs of narrowed, enlarged, or hardened arteries.
5. Can lifestyle changes prevent arteriosclerosis and atherosclerosis?
Yes, lifestyle changes can significantly impact prevention and management. These include eating a heart-healthy diet, engaging in regular physical activity, maintaining a healthy weight, quitting smoking, and managing stress.
6. What are the treatment options for these conditions?
Treatments range from lifestyle changes and medications (like cholesterol-lowering drugs, blood pressure medications, etc.) to surgical procedures (like angioplasty or bypass surgery) in more severe cases.
7. Can arteriosclerosis and atherosclerosis lead to other health issues?
Yes, if left untreated, these conditions can lead to serious complications like heart attacks, strokes, and peripheral artery disease.
8. Are there any new treatments or research in the field?
Ongoing research focuses on understanding the genetic and molecular basis of these diseases to develop more effective treatments. Advances in medical technology also continually improve diagnostic and treatment options.
Conclusion
If you’re experiencing symptoms that could suggest arteriosclerosis or atherosclerosis, such as chest pain, shortness of breath, or leg pain during physical activities, it’s crucial to consult a healthcare professional. Early detection and treatment can make a significant difference in managing these conditions and reducing the risk of serious complications like heart attacks and strokes.
Remember, while the information provided here is detailed, it is not a substitute for professional medical advice. Always seek the guidance of qualified health providers with any questions you may have regarding a medical condition. Your health and well-being are paramount, and timely medical intervention can be a lifesaver.