Aortic Valve Disease Treatment: Aortic valve disease is a critical condition affecting the heart’s aortic valve, pivotal in regulating blood flow from the heart to the rest of the body.
This disease encompasses various disorders, including aortic stenosis and aortic regurgitation, each presenting unique challenges to cardiac health.
Understanding Aortic Valve Disease
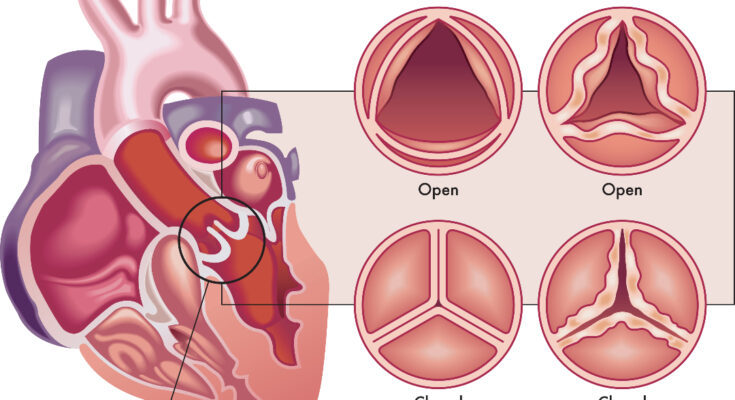
Aortic valve disease refers to conditions affecting the aortic valve, one of the heart’s four valves. This valve regulates blood flow from the heart into the aorta, the main artery. When afflicted, the valve may not open fully (stenosis) or may not close properly (regurgitation), impeding the heart’s efficiency and impacting overall cardiovascular health.
Causes and Risk Factors
- Age-Related Changes: Natural wear and tear over time can lead to aortic valve disease, especially in older adults.
- Congenital Heart Defects: Some people are born with an aortic valve that has only two cusps (bicuspid valve) instead of three, increasing the risk.
- Rheumatic Fever: This complication of strep throat can damage the aortic valve.
- Endocarditis: An infection of the valve.
- High Blood Pressure and Cholesterol: These conditions can accelerate valve damage.
- Lifestyle Factors: Smoking and obesity are known risk enhancers.
Prevalence and Demographics Affected
Aortic valve disease is a common cardiac condition, especially among the elderly. The prevalence increases with age, particularly in those over 65. While it can occur in any gender, certain types, like aortic stenosis, are more common in males. Moreover, individuals with a family history of heart diseases or congenital heart defects are at a higher risk.
However, aortic valve disease is a critical condition affecting millions worldwide. Understanding its causes, risk factors, and the demographics most affected is crucial for early detection and effective management.
Symptoms and Early Detection of Aortic Valve Disease
Aortic valve disease can present a range of symptoms, vital for early diagnosis and effective treatment. Common signs include:
- Shortness of Breath: Often experienced during activities or when lying down.
- Chest Pain or Pressure: Typically occurring with exertion and relieved by rest.
- Fatigue: A frequent and early symptom, especially during increased physical activity.
- Heart Palpitations: Sensations of a rapid, fluttering heartbeat.
- Dizziness or Fainting: Caused by reduced blood flow from the heart.
- Swelling: In the ankles and feet due to fluid retention.
Identifying these symptoms promptly can be crucial in managing the progression of the disease.
The Importance of Early Detection
Early detection plays a pivotal role in the successful treatment of aortic valve disease. It allows for timely intervention, potentially preventing severe complications like heart failure or sudden cardiac death. Recognizing symptoms early and consulting with a healthcare professional can significantly improve treatment outcomes and quality of life.
Diagnostic Tests and Procedures
To diagnose aortic valve disease, doctors may recommend a series of tests and procedures:
- Echocardiogram: Uses sound waves to create detailed images of the heart, assessing the valve’s function and structure.
- Electrocardiogram (ECG): Records the electrical activity of the heart, identifying irregular rhythms.
- Chest X-ray: Checks for an enlarged heart or other abnormalities.
- Cardiac MRI: Provides detailed images of the heart’s structure and function.
- Stress Test: Evaluates heart function during physical exertion.
- Cardiac Catheterization: Involves inserting a thin tube into the heart to measure pressure and flow.
These tests help in determining the severity of the disease and guiding treatment decisions.
Treatment Options for Aortic Valve Disease
The treatment options are diverse, ranging from medications to advanced surgical procedures. The choice of treatment depends on the severity of the condition, the patient’s overall health, and the specific characteristics of the valve disease.
Medications and Their Role in Treatment
Medications are often the first line of defense in managing aortic valve disease. They can help to reduce symptoms and slow the progression of the disease. Commonly prescribed medications include:
- Beta-blockers: Reduce heart rate and blood pressure, easing the heart’s workload.
- Diuretics: Help eliminate excess fluid, reducing the burden on the heart.
- Blood thinners: Prevent blood clots, a risk in some valve diseases.
- Antiarrhythmics: Control irregular heartbeats that can accompany valve disorders.
Surgical Options: Valve Repair and Valve Replacement
When medications are not sufficient, surgery may be necessary. There are two primary surgical approaches:
- Valve Repair: Preserving the patient’s own valve. This is often preferred as it involves less risk and preserves the natural heart structure.
- Valve Replacement: Involves removing the damaged valve and replacing it with a prosthetic valve. This can be either a mechanical valve, which lasts longer but requires lifelong blood thinners, or a bioprosthetic valve, which has a shorter lifespan but does not usually require blood thinners.
Traditional Surgery vs. Minimally Invasive Procedures
Aortic valve surgery can be performed through traditional open-heart surgery or through minimally invasive techniques. Traditional surgery involves a larger incision and longer recovery time but is sometimes necessary for complex cases. Minimally invasive procedures, such as Transcatheter Aortic Valve Replacement (TAVR), involve smaller incisions and offer quicker recovery times, making them a preferred option for many patients, especially those at higher surgical risk.
Emerging Treatments and Technologies
The field of aortic valve treatment is continually evolving, with new technologies and techniques being developed. These include advancements in prosthetic valve materials, less invasive surgical techniques, and better diagnostic tools for early detection and treatment planning. Research into stem cell therapy and tissue engineering also holds promise for future treatments.
However, the treatment of aortic valve disease has numerous options, each tailored to the patient’s specific needs. With advancements in medicine and technology, the prospects for successful treatment and improved quality of life continue to grow. It’s important for patients to consult with their healthcare providers to understand the best treatment path for their individual condition.
Living with Aortic Valve Disease
Lifestyle Modifications and Management
Living with aortic valve disease requires a proactive approach to maintaining your health. Adopting certain lifestyle changes can significantly impact the progression of the disease and enhance your quality of life. Key modifications include:
- Healthy Diet: Emphasize a heart-healthy diet rich in fruits, vegetables, whole grains, lean proteins, and low in saturated fats.
- Regular Exercise: Engage in regular physical activity tailored to your condition, but always consult with your healthcare provider before starting any new exercise regimen.
- Smoking Cessation: If you smoke, quitting is one of the most beneficial steps you can take to protect your heart.
- Weight Management: Maintaining a healthy weight reduces strain on the heart and can alleviate symptoms associated with aortic valve disease.
- Stress Management: Techniques such as meditation, yoga, or deep breathing exercises can help manage stress, which is crucial for heart health.
Ongoing Care and Monitoring
Regular medical check-ups and monitoring are vital in managing aortic valve disease effectively. This includes:
- Routine Echocardiograms: These tests monitor the condition of your heart valve and how well your heart is functioning.
- Blood Pressure Monitoring: Keeping your blood pressure within a target range is essential to reduce the burden on your aortic valve.
- Medication Adherence: If prescribed, consistently taking your medications as directed is crucial for managing your condition.
- Symptom Tracking: Keeping a record of any new or worsening symptoms and reporting them to your healthcare provider promptly.
Support Systems and Patient Resources
Navigating aortic valve disease is not a journey you should undertake alone. Various support systems and patient resources can provide invaluable assistance:
- Patient Support Groups: Connecting with others who are facing similar challenges can provide emotional support and practical advice.
- Educational Resources: Seek out reliable information from reputable sources to stay informed about your condition and treatment options.
- Professional Counseling: Mental health professionals can help you cope with the emotional aspects of living with a chronic illness.
- Family and Friends: Don’t hesitate to lean on your personal network for support in managing your daily needs and emotional well-being.
Prevention and Awareness of Aortic Valve Disease
Proactive Strategies for Prevention
Aortic valve disease, a critical condition affecting heart function, can often be managed more effectively with early detection and prevention. Adopting a proactive approach is essential. Here are key strategies:
- Healthy Lifestyle Choices: Emphasize a balanced diet, regular exercise, and avoiding smoking. These choices reduce the risk of conditions that can lead to aortic valve disease, like high blood pressure and atherosclerosis.
- Regular Monitoring of Heart Health: Especially for those with a family history of heart disease, regular monitoring can detect issues early. Encourage routine heart health evaluations with your healthcare provider.
- Managing Existing Health Conditions: For those with conditions like hypertension, diabetes, or high cholesterol, effective management is crucial. These conditions, if uncontrolled, can exacerbate the risk of developing aortic valve complications.
The Importance of Awareness and Regular Check-Ups
Awareness is a powerful tool in combating aortic valve disease. Understanding the symptoms – like breathlessness, chest pain, fatigue, and palpitations – can prompt earlier intervention and treatment. Regular check-ups play a pivotal role in this:
- Early Detection: Regular check-ups can identify signs of aortic valve disease before symptoms become severe.
- Personalized Health Strategies: Healthcare providers can offer tailored advice and monitoring based on individual health profiles.
Future Outlook and Ongoing Research
The future is promising with continuous advancements in the understanding and treatment of aortic valve disease. Ongoing research focuses on:
- Innovative Treatment Methods: Exploring less invasive surgical options and advanced medication.
- Genetic Research: Understanding the genetic factors of the disease to develop targeted therapies.
- Enhancing Prosthetic Valve Technology: Improving the durability and functionality of artificial valves.
Staying informed about these advancements and participating in regular health screenings can dramatically alter the course of aortic valve disease.
Conclusion
It cannot be overstressed how important it is to consult healthcare professionals when it comes to matters of heart health, particularly aortic valve disease. These experts can provide personalized advice and treatment plans based on your specific health needs.
Remember, early detection and intervention can make a significant difference in the outcome of heart-related conditions. Do not hesitate to reach out to your doctor if you experience any symptoms or have concerns about your heart health.