Aortic Dissection Symptoms: Aortic dissection is a serious condition that involves the aorta, the main artery leading from the heart.
Understanding the symptoms and causes of this potentially life-threatening condition is crucial for early diagnosis and treatment.
This comprehensive article aims to provide a detailed overview of the symptoms and causes of aortic dissection, thereby enhancing awareness and promoting prompt medical intervention.
What is Aortic Dissection?
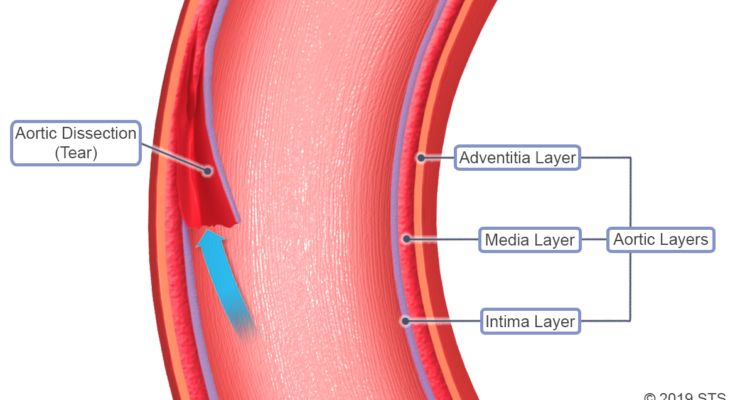
Aortic dissection is a serious medical condition that demands immediate attention. It occurs when there is a tear in the inner layer of the aorta, the large blood vessel branching off the heart. This tear allows blood to flow between the layers of the wall of the aorta, leading to a dissection. The condition can be life-threatening and requires prompt diagnosis and treatment.
Types of Aortic Dissection
There are two main types of aortic dissection, categorized based on the location of the tear:
- Type A: This type involves a tear in the ascending aorta, which may extend into the abdomen. Type A is more common and more dangerous, often requiring surgical intervention.
- Type B: In this type, the tear is located in the descending aorta and may also extend into the abdomen. Type B is typically treated with medications, although surgery may be necessary in some cases.
Prevalence and Demographic Statistics
Aortic dissection is relatively rare, affecting approximately 5-30 people per million each year. It is more common in men than women, with men in their 60s and 70s being the most frequently affected group. Risk factors include high blood pressure, a history of heart surgery or heart disease, and certain genetic conditions.
Understanding aortic dissection, its types, and its prevalence is crucial for early detection and treatment, which can significantly improve outcomes for those affected by this condition.
Symptoms of Aortic Dissection
Here is an in-depth look at the symptoms of aortic dissection, differentiating them from other cardiac issues, and includes personal stories or case studies for a comprehensive understanding.
Common Symptoms of Aortic Dissection
- Sudden Severe Chest or Upper Back Pain: Often described as a tearing or ripping sensation, this pain is distinct in its intensity and onset.
- Loss of Consciousness: Fainting or blackouts can occur due to reduced blood flow.
- Shortness of Breath: Patients may experience difficulty breathing, often a result of the dissection impacting lung function.
- Weak Pulse or Uneven Blood Pressure: There might be a noticeable difference in pulse strength or blood pressure between limbs.
- Stroke-like Symptoms: In some cases, symptoms like speech difficulties, paralysis, or weakness on one side of the body may occur.
Differentiating from Other Cardiac Issues
- Intensity and Nature of Pain: Unlike a heart attack, where the pain is often a heavy, pressing sensation, aortic dissection pain is sharp and tearing.
- Symptom Onset: The symptoms of aortic dissection are sudden and severe, which is a critical differentiator from other gradual-onset cardiac conditions.
- Physical Manifestations: Stroke-like symptoms and differences in pulse and blood pressure are more specific to aortic dissection than to other cardiac problems.
Recognizing the symptoms of aortic dissection is crucial for timely and effective treatment. Understanding how these symptoms differ from other cardiac issues can be lifesaving. Personal stories further highlight the importance of awareness and quick response to this medical emergency.
Causes and Risk Factors of Aortic Dissection
This article provides an in-depth examination of the causes that lead to aortic dissection, aiming to enhance understanding of this critical health issue.
Key Risk Factors Contributing to Aortic Dissection
Several risk factors contribute to the likelihood of developing aortic dissection. These include:
- Age and Gender Dynamics: Aortic dissection is more commonly observed in individuals aged between 60 and 80 years. Men are at a higher risk compared to women, with a ratio of about two to one.
- Genetic Factors: Certain genetic conditions, like Marfan syndrome and Ehlers-Danlos syndrome, can predispose individuals to aortic dissection. Family history of aortic diseases also plays a significant role.
- Lifestyle Influences: Factors such as smoking, high cholesterol, and obesity can increase the risk of aortic dissection. A sedentary lifestyle and poor diet are also contributing factors.
The Critical Role of High Blood Pressure
High blood pressure (hypertension) is a leading risk factor for aortic dissection. Persistent high blood pressure can cause stress on the arterial wall, leading to a higher likelihood of a tear developing. Controlling blood pressure through medication, diet, and lifestyle changes is crucial in reducing the risk of aortic dissection.
Understanding the causes and risk factors of aortic dissection is essential for prevention and early detection. Regular health check-ups, especially for those in high-risk groups, are vital for maintaining cardiovascular health and preventing conditions like aortic dissection. Remember, early detection and lifestyle changes can make a significant difference in outcomes.
Diagnosing Aortic Dissection
Understanding the diagnostic methods, the significance of early detection, and the challenges posed by symptom-based diagnosis is crucial for both medical professionals and patients.
Methods and Technologies Used in Diagnosis
1. Imaging Techniques: The cornerstone of diagnosing aortic dissection involves advanced imaging techniques. This includes:
- Computed Tomography (CT) Scan: A CT scan is often the first-line imaging test. It provides detailed images of the aorta, helping to identify the presence and extent of a dissection.
- Magnetic Resonance Imaging (MRI): MRI offers high-resolution images and is particularly useful in assessing the aorta’s condition without exposing patients to radiation.
- Transesophageal Echocardiogram (TEE): This technique uses sound waves to create images of the heart and aorta. It’s especially beneficial for patients who cannot undergo CT or MRI.
2. Blood Tests: While not diagnostic for aortic dissection, blood tests can rule out other conditions and assess the overall health of the patient.
The Role of Early Detection in Effective Treatment
- Reducing Complications: Early detection of aortic dissection is vital. It significantly reduces the risk of severe complications such as aortic rupture or organ damage.
- Guiding Treatment Decisions: Timely diagnosis allows for immediate treatment decisions, which can range from surgery to medication management, depending on the dissection’s severity and location.
Challenges in Diagnosing Based on Symptoms Alone
- Vague Presentation: The symptoms of aortic dissection, such as chest pain and shortness of breath, are often similar to those of less serious conditions like heartburn or muscle strain, leading to misdiagnosis.
- Rapid Progression: The condition can rapidly worsen, so a high index of suspicion is required, especially in patients with risk factors like high blood pressure or a history of heart disease.
However, the diagnosis of aortic dissection involves a combination of advanced imaging techniques and a high index of suspicion. Early detection plays a pivotal role in managing this life-threatening condition, highlighting the need for awareness among healthcare providers and at-risk populations. Understanding the challenges in symptom-based diagnosis is key to preventing misdiagnosis and ensuring timely and effective treatment.
Treatment and Management of Aortic Dissection
Understanding the treatment options and the importance of emergency care is crucial for health professionals and patients alike. Here’s an overview of the current treatment methods and long-term management strategies for aortic dissection.
Overview of Current Treatment Options
- Surgical Intervention: For certain types of aortic dissections, especially those involving the ascending aorta, immediate surgery is often necessary. This procedure aims to repair the torn area of the aorta.
- Medication: In cases where surgery is not immediately required, or for certain types of dissections, medications to lower blood pressure and reduce the heart rate are commonly used. This helps decrease the force exerted on the torn aorta.
- Monitoring: Regular imaging tests are vital to monitor the aorta’s condition post-diagnosis, whether the patient undergoes surgery or is managed with medication.
Importance of Emergency Care in Aortic Dissection
- Prompt Diagnosis: Early detection and diagnosis are critical. Symptoms like sudden severe chest or upper back pain, shortness of breath, and symptoms of stroke demand immediate medical attention.
- Risk Assessment: Quick risk assessment by medical professionals can determine the necessity of urgent surgical intervention.
- Stabilization: Before any long-term treatment plan, stabilizing the patient’s condition is essential, which often includes controlling blood pressure and heart rate.
Long-term Management Strategies for Patients
- Lifestyle Modifications: Adopting a heart-healthy lifestyle is crucial. This includes regular exercise, a balanced diet, quitting smoking, and managing stress.
- Regular Follow-ups: Ongoing care with frequent check-ups and imaging tests helps in monitoring the condition and adjusting treatments as necessary.
- Medication Adherence: Patients must adhere to prescribed medication regimens to manage blood pressure and reduce the risk of further complications.
- Patient Education: Understanding the condition, its risks, and the importance of ongoing care is vital for patients.
By comprehensively understanding and implementing these treatment and management strategies, the risks associated with aortic dissection can be significantly reduced, leading to better patient outcomes. Remember, aortic dissection is a medical emergency, and early intervention is key to successful treatment and management.
Prevention and Awareness of Aortic Dissection
Strategies for Prevention Focusing on Modifiable Risk Factors
Aortic dissection, a serious condition where the inner layer of the aorta tears, can often be prevented by addressing modifiable risk factors. Key strategies include:
- Maintaining Healthy Blood Pressure: High blood pressure is a significant risk factor for aortic dissection. It’s crucial to maintain blood pressure within a healthy range through lifestyle changes and, if necessary, medication.
- Heart-Healthy Diet: Adopting a diet low in saturated fats and cholesterol, rich in fruits, vegetables, and whole grains can help in reducing the risk.
- Regular Exercise: Engaging in regular physical activity helps in maintaining a healthy weight and reducing blood pressure, both of which are important for aortic health.
- Avoiding Smoking and Excessive Alcohol: Smoking and excessive alcohol consumption can weaken the arterial walls, increasing the risk of aortic dissection.
- Stress Management: Chronic stress can contribute to high blood pressure and heart disease, so managing stress through techniques like meditation, yoga, or counseling is beneficial.
Importance of Regular Medical Check-Ups and Awareness
Early detection and management of conditions that could lead to aortic dissection are critical. Regular medical check-ups are essential for:
- Monitoring Blood Pressure: Consistent monitoring can detect hypertension early, allowing for timely intervention.
- Screening for Heart Conditions: Regular heart health evaluations can identify issues that may predispose individuals to aortic dissection.
- Patient Education: Health professionals can provide valuable information about the warning signs of aortic dissection, enabling individuals to seek prompt medical attention.
Resources for Further Information and Support
For those seeking more information or support regarding aortic dissection, numerous resources are available:
- Healthcare Providers: Your primary care physician or a cardiologist can offer personalized advice and information.
- Online Platforms: Websites like the American Heart Association provide comprehensive information about heart health and aortic dissection.
- Support Groups: Local or online support groups can be a source of comfort and information, connecting individuals with others who have experienced similar health issues.
However, prevention and awareness of aortic dissection are pivotal in mitigating risks associated with this condition. By focusing on modifiable risk factors, maintaining regular health check-ups, and utilizing available resources, individuals can significantly reduce their risk and ensure prompt treatment if needed.
FAQs on Aortic Dissection Symptoms and Causes
What are the main symptoms of aortic dissection?
Aortic dissection typically presents with sudden, severe chest or upper back pain, often described as a tearing sensation. The pain may radiate to the neck, jaw, or arms. Some patients experience a sudden onset of shortness of breath, fainting, or stroke-like symptoms due to disrupted blood flow.
Can aortic dissection symptoms be mistaken for other conditions?
Yes, the symptoms of aortic dissection can be similar to other heart-related conditions like heart attacks. This similarity can lead to misdiagnosis. It’s crucial for medical professionals to consider aortic dissection in patients with severe chest pain and risk factors for this condition.
What causes an aortic dissection?
Aortic dissection is often caused by hypertension (high blood pressure) which stresses the arterial wall. Other causes include genetic conditions like Marfan syndrome or Ehlers-Danlos syndrome, a history of heart surgery, or traumatic injury to the chest.
Are there any risk factors that increase the likelihood of aortic dissection?
Risk factors for aortic dissection include chronic high blood pressure, a family history of the condition, pre-existing aortic valve disease, and lifestyle factors like smoking. Men in their 60s and 70s are at higher risk.
Is aortic dissection a medical emergency?
Absolutely. Aortic dissection is a life-threatening emergency requiring immediate medical attention. Delay in treatment can lead to fatal complications like aortic rupture or organ damage due to reduced blood flow.
How is aortic dissection diagnosed?
Diagnosis of aortic dissection usually involves imaging tests like CT scans, MRI, or echocardiography. These tests help visualize the aorta and identify the presence of a dissection.
Can lifestyle changes reduce the risk of aortic dissection?
Lifestyle modifications can reduce the risk of aortic dissection. This includes managing high blood pressure, quitting smoking, maintaining a healthy weight, and regular monitoring for those with genetic conditions affecting the aorta.
Conclusion
We strongly encourage anyone experiencing symptoms indicative of aortic dissection, such as severe chest pain, shortness of breath, or fainting, to seek medical advice immediately. Timely intervention can be the difference between life and death.
Consulting with healthcare professionals ensures that you receive an accurate diagnosis and appropriate treatment, significantly improving your chances of a positive outcome.