Anthrax Symptoms: Anthrax, a serious infectious disease, is caused by the bacterium Bacillus anthracis. This disease can affect both humans and animals, primarily grazing livestock. It has been a concern for centuries, notably used as a biological weapon.
This article delves into the critical aspects of anthrax, including its symptoms, causes, and transmission.
What is Anthrax?
Anthrax stands as a significant medical and biological concern due to its history and potential use as a biohazard. This section delves into the detailed definition of anthrax, provides a historical overview of its outbreaks, and acknowledges its classification as a biological hazard.
Detailed Definition of Anthrax
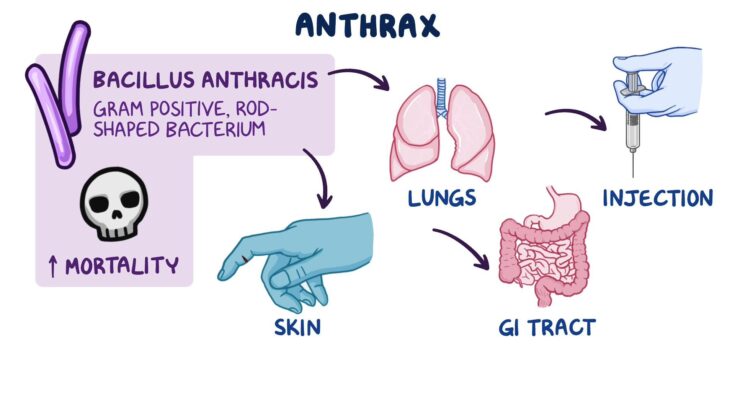
Anthrax is a severe infectious disease caused by the bacterium Bacillus anthracis. It predominantly affects livestock and wild game, but can also infect humans. The disease manifests in three forms: cutaneous (skin), inhalation, and gastrointestinal. Each form presents distinct symptoms and varies in severity, with inhalation anthrax being the most lethal. The bacteria produce spores that can survive in the environment for decades, posing a persistent risk.
Historical Context of Anthrax Outbreaks
Historically, anthrax has been both a naturally occurring illness and a tool of warfare and bioterrorism. Outbreaks have been recorded since ancient times, with significant occurrences impacting both human and animal populations globally. In the early 20th century, anthrax was notably used in biological warfare programs, and more recently, it garnered attention during the 2001 anthrax letter attacks in the United States.
Classification as a Biological Hazard
Anthrax is classified as a Category A biological hazard by the Centers for Disease Control and Prevention (CDC). This classification is reserved for pathogens that pose the highest risk to national security and public health due to their ease of dissemination, high mortality rates, potential for major public health impact, and the necessity for special preparedness.
Anthrax Symptoms
Here is an in-depth look at the common symptoms associated with anthrax, helping you understand and identify them quickly.
Common Symptoms of Anthrax
Anthrax symptoms vary based on the type of infection but generally include:
- Cutaneous Anthrax: This form, resulting from skin contact with the bacterium, typically presents with a blister or bump that develops into a painless ulcer with a black center.
- Inhalation Anthrax: Acquired by inhaling spores, inhalation anthrax starts with flu-like symptoms which rapidly progress to severe respiratory issues.
- Gastrointestinal Anthrax: Ingestion of contaminated food leads to gastrointestinal anthrax, marked by nausea, vomiting, abdominal pain, and severe diarrhea.
- Injection Anthrax: Although rare, injection anthrax (linked to injected drugs) causes deep, intense skin sores accompanied by fever and potentially severe systemic issues.
Detailed Symptom Breakdown for Each Anthrax Type
Cutaneous Anthrax Symptoms:
- Initial itching followed by a lesion resembling an insect bite
- Development of a painless sore with a black necrotic center
- Swelling in nearby lymph glands
Inhalation Anthrax Symptoms:
- Early signs include fever, fatigue, and a mild cough or chest discomfort
- Rapid progression to severe breathing difficulties and shock
Gastrointestinal Anthrax Symptoms:
- Acute inflammation of the intestinal tract
- Nausea and vomiting, often bloody
- Severe abdominal pain followed by diarrhea
Injection Anthrax Symptoms:
- Redness and swelling at the injection site
- Formation of abscesses
- Fever and chills, possibly leading to septicemia
Understanding the symptoms of the different types of anthrax is vital for early detection and treatment. If you suspect anthrax exposure, seek immediate medical attention. Awareness is the first step in combating this serious infection.
Causes of Anthrax
Anthrax is caused by the bacterium Bacillus anthracis, found in soil. The bacterium forms spores that can survive for decades in harsh conditions. Transmission occurs through:
Transmission Methods: How Anthrax Spreads
The transmission of anthrax occurs through various means, each linked to the spores of Bacillus anthracis. Common routes include:
- Direct Contact: Handling infected animals or contaminated animal products can lead to cutaneous anthrax, the most common form.
- Inhalation: Breathing in anthrax spores, typically from contaminated animal products or in bioterrorism scenarios, can cause inhalational anthrax, which is the most deadly form.
- Ingestion: Consuming undercooked meat from infected animals can lead to gastrointestinal anthrax.
Understanding these transmission methods is vital for implementing preventive measures and controlling the spread of the disease.
Risk Factors and Vulnerable Populations
Certain factors and populations are more susceptible to anthrax. Key risk factors include:
- Occupational Exposure: Veterinarians, farmers, and laboratory workers handling animal products are at a higher risk.
- Geographical Location: Areas with a history of anthrax in animals pose a greater risk for human infection.
- Unvaccinated Individuals: Those unvaccinated against anthrax are more susceptible, particularly in high-risk professions.
Identifying and protecting these vulnerable populations is a significant step in preventing and managing anthrax outbreaks. By understanding the causes and risk factors of anthrax, health professionals and individuals can better prepare and respond to potential threats posed by this serious bacterial disease.
Diagnosis of Anthrax
The process of diagnosing anthrax involves a combination of clinical assessment and specific laboratory tests.
Key Diagnostic Tests for Anthrax
- Blood Cultures: The most common test for anthrax involves taking blood samples to identify the presence of Bacillus anthracis.
- Skin Lesion Samples: In cases of cutaneous anthrax, samples from skin lesions are tested.
- Chest X-rays and CT Scans: These imaging tests are crucial for diagnosing inhalation anthrax, as they can reveal characteristic abnormalities in the lungs.
- Polymerase Chain Reaction (PCR) Tests: PCR tests are used to detect the genetic material of the anthrax bacteria, offering a rapid and sensitive diagnosis.
- Serologic Testing: This involves detecting antibodies against the bacterium, although it’s more useful for epidemiological studies rather than acute diagnosis.
The Crucial Role of Early Detection
Early detection of anthrax is vital for several reasons:
- Improves Treatment Efficacy: Early-stage anthrax is more responsive to antibiotics.
- Reduces Mortality Risk: Particularly in inhalation anthrax, early treatment significantly reduces the risk of fatal outcomes.
- Prevents Spread: Quick identification helps in containing potential outbreaks, especially in bioterrorism scenarios.
Symptoms and Their Diagnostic Importance
Recognizing the symptoms of anthrax plays a pivotal role in diagnosis. Symptoms vary depending on the type of anthrax but generally include:
- Cutaneous Anthrax: Appears as a raised, itchy bump that develops into a painless sore with a black center.
- Inhalation Anthrax: Initial symptoms resemble a common cold, progressing to severe respiratory distress.
- Gastrointestinal Anthrax: Characterized by nausea, loss of appetite, vomiting, and fever.
Healthcare professionals often initiate the diagnostic process based on the presence of these symptoms, especially in individuals with a history of exposure to infected animals or contaminated materials.
The diagnosis of anthrax hinges on a blend of clinical acumen and specific laboratory tests. Recognizing the symptoms early and understanding the importance of prompt testing can make a significant difference in treatment outcomes and in preventing the spread of this potentially lethal disease.
Treatment Options for Anthrax
The primary mode of treatment is through antibiotics, which play a crucial role in managing this infection. However, the choice of antibiotics and the duration of treatment depend on the anthrax’s form (cutaneous, inhalation, or gastrointestinal) and severity.
1. Antibiotics: The First Line of Defense
- Penicillin: Historically, penicillin was the first choice for treating anthrax. However, due to possible resistance, it’s now often replaced with other antibiotics.
- Ciprofloxacin and Doxycycline: These are the frontline treatments, especially in cases of suspected or confirmed bioterrorism, where antibiotic resistance is a concern. They are effective in all forms of anthrax.
- Duration and Administration: Treatment usually continues for 60 days, especially in inhalation anthrax, to completely eradicate the spores. Oral and intravenous options are available, depending on the infection’s severity.
2. Supportive Care: Managing Symptoms and Complications
- Hydration and Nutrition: Ensuring adequate hydration and nutrition is vital, especially in severe cases.
- Pain Management: Symptomatic treatment for pain and inflammation is essential, particularly in cutaneous anthrax.
- Breathing Assistance: For inhalation anthrax, mechanical ventilation may be necessary.
3. Vaccine and Post-Exposure Prophylaxis
- Vaccine Availability: While a vaccine is available, it’s primarily for at-risk populations (like military personnel) and not for general use.
- Post-Exposure Prophylaxis: In cases of exposure, antibiotics can be used as a preventative measure, often in combination with the vaccine.
Effectiveness and Duration: A Balancing Act
- Early Treatment: The effectiveness of treatment is significantly higher if started early, particularly within a few days of exposure.
- Challenges with Late Diagnosis: Delayed treatment, especially in inhalation anthrax, can drastically reduce the chances of survival, underscoring the importance of quick diagnosis and treatment initiation.
The treatment of anthrax, while straightforward in theory, requires careful consideration of the type of exposure, symptoms, and timing. The effectiveness of antibiotics is high with early intervention, but the potential for resistance and complications necessitates a thorough understanding of treatment options. It’s essential for healthcare professionals to stay updated on the latest guidelines and for individuals to seek immediate care if exposure is suspected.
Prevention and Control of Anthrax
Prevention is a critical step in safeguarding individuals and communities against this disease. Here are the key strategies:
- Vaccination: The anthrax vaccine is a primary tool in preventing infection, especially for those at higher risk, such as military personnel, laboratory workers, and individuals handling potentially infected animals. It’s crucial to follow the recommended vaccination schedule for optimal protection.
- Safety Practices in High-Risk Occupations: For those working in environments with a higher risk of exposure, such as livestock handling and veterinary fields, wearing appropriate protective gear is essential. This includes gloves, masks, and other personal protective equipment.
- Regulations in Animal Husbandry: Implementing strict regulatory measures in livestock management to prevent infection in animals is vital. This includes proper vaccination, disposal of potentially infected carcasses, and maintaining hygienic conditions in farms and slaughterhouses.
Measures for Controlling Outbreaks and Limiting Disease Spread
When an anthrax outbreak occurs, prompt and effective control measures are crucial to limit its spread and impact. The following are key measures:
- Rapid Identification and Isolation: Quick identification of infected individuals or animals and their subsequent isolation is crucial to prevent the spread of anthrax.
- Use of Antibiotics: In the event of exposure, early administration of antibiotics can be lifesaving. Antibiotics like ciprofloxacin, doxycycline, or amoxicillin are used under medical supervision.
- Public Health Education: Educating the public, especially in vulnerable areas, about the signs and symptoms of anthrax and the importance of seeking immediate medical care is essential.
- Environmental Decontamination: In the case of an outbreak, decontaminating the affected environment is vital. This includes the safe disposal of infected animal products and sterilization of contaminated areas.
- International Collaboration: Since anthrax is a global concern, international cooperation in sharing information, resources, and strategies is crucial for effective control.
By implementing these prevention and control measures, we can significantly reduce the risk and impact of anthrax outbreaks. Regular updates from health authorities and adherence to safety guidelines are vital in staying ahead of this serious disease.
Conclusion
If you or someone you know exhibits any symptoms of anthrax, it’s imperative to consult a healthcare professional immediately. Timely medical advice and treatment are essential for managing this disease effectively.
By staying informed and vigilant, we can better protect ourselves and our communities from the risks of anthrax. Remember, your health and safety are paramount – don’t hesitate to seek professional advice if you suspect exposure to this serious disease.