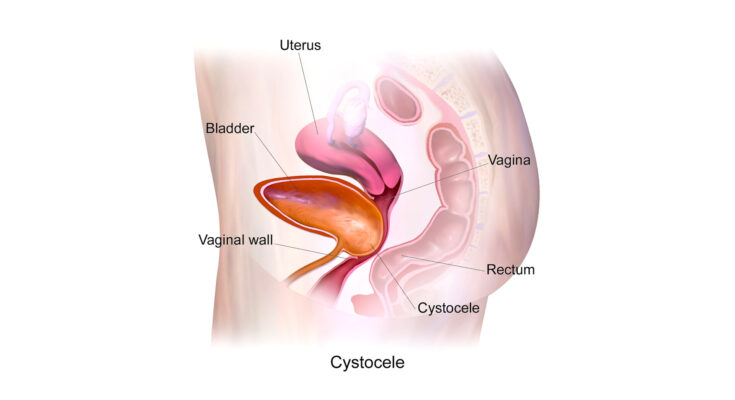
Anterior Vaginal Prolapse Symptoms: Anterior vaginal prolapse, commonly known as cystocele, is a medical condition characterized by the bulging or herniation of the bladder into the vagina.
This condition occurs when the muscles and supportive tissues between a woman’s bladder and vaginal wall weaken.
The primary cause of this weakening is often related to childbirth, but other factors like age, menopause, and chronic constipation can also contribute.
What is Anterior Vaginal Prolapse?
Anterior Vaginal Prolapse (AVP), often referred to as a cystocele, is a medical condition where the bladder bulges into the vaginal canal due to weakened pelvic floor muscles. This weakening can be a result of various factors such as childbirth, aging, or heavy lifting. AVP typically presents symptoms like discomfort or pressure in the pelvic area, urinary incontinence, or difficulties during sexual intercourse. Understanding AVP is crucial for timely diagnosis and effective treatment.
Understanding AVP: A Detailed Definition
AVP occurs when the front wall of the vagina, which supports the bladder, weakens or loosens. This leads to the bladder sagging or bulging into the vagina, causing discomfort and other symptoms. The severity of AVP varies; in mild cases, there may be few or no noticeable symptoms, whereas more severe cases can significantly impact quality of life.
How AVP Differs from Other Types of Vaginal Prolapse
While AVP specifically involves the bladder and the front wall of the vagina, other types of vaginal prolapse can affect different parts of the pelvic anatomy. For example, a rectocele is a prolapse of the back wall of the vagina, often involving the rectum, and uterine prolapse involves the descent of the uterus into the vaginal canal. Understanding these distinctions is vital for proper diagnosis and treatment. Each type of prolapse has unique symptoms and treatment approaches, emphasizing the importance of a correct diagnosis.
In summary, Anterior Vaginal Prolapse is a condition characterized by the weakening of the pelvic floor muscles leading to the bladder bulging into the vagina. It’s essential to differentiate AVP from other types of vaginal prolapse for accurate diagnosis and effective treatment. Regular pelvic exams and awareness of symptoms can aid in early detection and management of AVP.
Symptoms of Anterior Vaginal Prolapse
The symptoms of cystocele vary among individuals but typically include:
Common Symptoms of Anterior Vaginal Prolapse
- Sensation of Pelvic Pressure or Fullness: Women often describe a feeling of heaviness or dragging in the pelvic area. This sensation may worsen as the day progresses or during physical activities like lifting.
- Visible Bulge in the Vagina: In more advanced cases, a bulge may be seen or felt at the vaginal opening. It is a clear indicator that the bladder is protruding into the vaginal space.
- Discomfort or Pain During Intercourse: Sexual activity may become uncomfortable or painful due to the altered anatomy and pressure in the vaginal area.
- Urinary Problems: These can include frequent urination, a feeling of incomplete bladder emptying, or urinary incontinence, especially when coughing, sneezing, or exercising.
- Lower Back Pain: As the prolapse worsens, it can lead to a dull, aching pain in the lower back, often linked to the added pressure on pelvic organs.
- Difficulties with Bowel Movements: Some women experience constipation or difficulty in bowel evacuation, as the prolapsed bladder can exert pressure on the rectum.
Impact on Daily Life
These symptoms can profoundly affect daily activities and quality of life. The discomfort and pain can limit physical activities and exercise tolerance, leading to a sedentary lifestyle. Urinary problems can be particularly distressing, often leading to social embarrassment and avoidance of social activities. The impact on sexual health can strain intimate relationships and affect mental well-being.
Moreover, the constant discomfort can lead to chronic stress and fatigue, affecting overall health. Women may also experience a decrease in self-esteem and body image issues due to the visible changes and symptoms.
It’s essential for women experiencing these symptoms to consult a healthcare provider for proper diagnosis and management. Early intervention can help manage symptoms effectively and improve quality of life.
Remember, while these symptoms are common indicators of AVP, they can also be signs of other conditions. Therefore, a medical evaluation is crucial for an accurate diagnosis and appropriate treatment plan.
Potential Causes of Anterior Vaginal Prolapse
Understanding the causes of AVP is crucial for both prevention and effective treatment. This section delves into the various factors that can contribute to the development of AVP, highlighting the roles of lifestyle choices, genetic predispositions, and coexisting medical conditions.
Lifestyle Factors Influencing AVP
Lifestyle plays a significant role in the risk of developing anterior vaginal prolapse. Key lifestyle factors include:
- Childbirth: Vaginal deliveries, especially multiple or complicated births, can weaken pelvic muscles and tissues, increasing the risk of prolapse.
- Physical Strain: Activities that put excessive pressure on the pelvic floor, like heavy lifting, can lead to prolapse.
- Obesity: Excess weight increases the strain on pelvic muscles, contributing to the development of AVP.
- Smoking: Smoking can lead to a chronic cough, which repeatedly stresses the pelvic muscles, increasing prolapse risk.
Genetic Predisposition
Genetics also play a crucial role in the likelihood of developing AVP. Women with a family history of pelvic organ prolapse are at a higher risk, suggesting a hereditary component to the condition.
Coexisting Medical Conditions
Several medical conditions can increase the risk of AVP, including:
- Menopause: Reduced estrogen levels during menopause can weaken pelvic tissues, making prolapse more likely.
- Chronic Respiratory Issues: Conditions like asthma or chronic bronchitis, which involve frequent coughing, can strain pelvic muscles.
- Hysterectomy: Surgical removal of the uterus can alter the support of pelvic organs, potentially leading to prolapse.
- Neurological Conditions: Diseases affecting the nervous system, such as multiple sclerosis or spinal injuries, can disrupt the normal function of the pelvic floor.
Understanding the potential causes of anterior vaginal prolapse is essential for both prevention and treatment. Women should be aware of these risk factors and discuss them with their healthcare providers, especially if they have a family history of pelvic organ prolapse or have other risk factors. Early intervention and lifestyle adjustments can significantly reduce the risk of developing AVP.
Diagnosis of Anterior Vaginal Prolapse
Diagnosing this condition involves a comprehensive approach that focuses on patient history, physical examination, and, in some cases, additional tests.
The initial step usually involves a detailed discussion about the patient’s symptoms, medical history, and any pelvic surgeries or childbirth experiences. This conversation helps healthcare providers understand the severity of the symptoms and their impact on the patient’s quality of life.
Following this, a physical examination is conducted. This typically includes a pelvic exam, where the doctor checks for any bulging in the vaginal wall and assesses the strength of the pelvic muscles.
In certain scenarios, further diagnostic tests may be required. These can include:
- Urodynamic Tests: These tests assess how well the bladder, sphincters, and urethra are storing and releasing urine.
- Cystoscopy: A procedure where a small camera is inserted into the bladder via the urethra to check for abnormalities.
- Imaging Tests: Tests like ultrasounds or MRIs can provide a detailed view of the pelvic organs.
Medical Professionals Involved in Diagnosis
The diagnosis of anterior vaginal prolapse often involves a team of medical professionals. This team may include:
- Primary Care Physicians: They often conduct the initial evaluation.
- Gynecologists: Specialists who focus on female reproductive health.
- Urogynecologists: Experts in pelvic floor disorders affecting women.
- Urologists: Specialists in urinary tract disorders.
Importance of Early Detection
Early detection of anterior vaginal prolapse is crucial for several reasons:
- Preventing Progression: Early diagnosis can help prevent the prolapse from worsening.
- Managing Symptoms Effectively: Timely intervention can lead to more effective management of symptoms.
- Improving Quality of Life: Early treatment can significantly improve a patient’s quality of life, reducing discomfort and other related symptoms.
It’s essential for women experiencing symptoms like a feeling of fullness in the pelvic area, discomfort in the vagina, or urinary problems, to consult their healthcare provider. Early intervention can lead to more effective treatment and better overall outcomes.
Treatment Options for Anterior Vaginal Prolapse
Fortunately, there are various treatment options available, ranging from simple lifestyle changes to medical procedures. In this article, we will explore these treatment options and discuss the effectiveness of each.
Lifestyle Changes and Non-Surgical Options
- Pelvic Floor Exercises (Kegels): Strengthening the pelvic floor muscles can be very effective in managing symptoms of anterior vaginal prolapse. Regular Kegel exercises can help in tightening and toning these muscles.
- Weight Management: Maintaining a healthy weight can reduce the pressure on pelvic organs and alleviate symptoms.
- Avoiding Heavy Lifting: Reducing strain on the pelvic floor by avoiding heavy lifting can help in managing prolapse.
- Estrogen Therapy: For postmenopausal women, estrogen therapy can help strengthen vaginal tissues, although it’s not suitable for everyone.
- Pessary: A pessary is a removable device placed inside the vagina to support areas affected by prolapse. It’s a non-surgical option that can be effective for many women.
Surgical Treatments
- Anterior Colporrhaphy: This surgical procedure involves tightening the tissues that support the bladder.
- Sling Procedures: These involve using synthetic material or your own tissue to create a sling around the bladder neck to support the urethra and bladder.
- Hysterectomy: In some cases, removing the uterus (hysterectomy) might be recommended, especially if the prolapse is severe.
- Mesh Repair: Surgical mesh can be used to reinforce the vaginal wall. However, it’s important to discuss the potential risks and benefits with your doctor, as there have been concerns about mesh complications.
Effectiveness of Treatments
- Pelvic Exercises and Lifestyle Changes: These are highly effective for mild cases and as preventative measures.
- Pessary: Offers temporary relief and is effective for those who prefer non-surgical options.
- Surgical Treatments: Generally offer long-term solutions and are typically more effective for moderate to severe prolapse.
However, the treatment for anterior vaginal prolapse depends on the severity of the condition, the patient’s health status, and personal preferences. It’s crucial to consult with a healthcare provider to determine the most suitable treatment plan. With the right approach, many women find significant relief from symptoms and an improvement in their quality of life.
Prevention and Management of Auditory Verbal Processing Issues
Preventing or managing these challenges is crucial for improving quality of life and communication skills.
Strategies for Prevention and Management:
Early Intervention: Recognizing AVP issues early on is key. Engage with healthcare professionals who specialize in auditory processing to get a tailored management plan.
Exercise Your Brain: Activities like puzzles, memory games, and language exercises can enhance auditory processing abilities. They keep the brain active and improve its ability to decode and comprehend verbal information.
Lifestyle Choices for Better AVP Management:
- Exercise Regularly: Physical activity can improve overall brain health. Cardiovascular exercises, in particular, increase blood flow to the brain, which can enhance auditory processing capabilities.
- Healthy Diet: A balanced diet rich in omega-3 fatty acids, antioxidants, and vitamins can support brain health. Foods like fish, nuts, berries, and leafy greens are especially beneficial.
Mindfulness and Stress Reduction: High stress levels can exacerbate AVP issues. Practices like yoga, meditation, and mindfulness can reduce stress and improve concentration and auditory processing.
Consistent Sleep Patterns: Adequate sleep is crucial for brain function. Establishing a regular sleep schedule can help in managing AVP symptoms.
Technology Aids: Use of assistive listening devices and apps designed for auditory training can be beneficial. These tools can help in enhancing auditory discrimination and comprehension.
Professional Support: Regular consultations with audiologists and speech therapists can provide specific strategies and exercises tailored to individual needs.
While AVP issues can be challenging, adopting a proactive approach involving exercise, a healthy diet, stress management, and consistent sleep patterns can significantly help in managing symptoms. Combining these lifestyle choices with professional guidance and technology aids can lead to better coping strategies and an enhanced quality of life.
Conclusion
If you are experiencing any symptoms of anterior vaginal prolapse, it’s crucial to consult with a healthcare professional. Early diagnosis and intervention can prevent the progression of the condition and improve your quality of life.
Medical advice tailored to your specific condition is essential, as treatment options vary based on the severity and individual circumstances. Remember, seeking professional help is a proactive step towards your health and well-being.