Ankylosing Spondylitis Symptoms: Ankylosing Spondylitis (AS) is a chronic condition primarily affecting the spine and the sacroiliac joints, which connect the spine to the pelvis. It is a form of arthritis that leads to inflammation and can cause severe, chronic pain and discomfort.
Understanding the symptoms and causes of Ankylosing Spondylitis is crucial for early diagnosis and effective management of the condition.
What is Ankylosing Spondylitis?
Ankylosing Spondylitis (AS) is a chronic inflammatory disease primarily affecting the spine and sacroiliac joints, leading to pain and stiffness. Over time, it can cause the vertebrae in your spine to fuse, making the spine less flexible and potentially resulting in a hunched-forward posture. AS is part of the larger family of diseases called spondyloarthritis.
Brief History and Prevalence of AS
The exact origins of AS are not clear, but historical records suggest its presence in human populations for centuries. The condition was first distinguished from rheumatoid arthritis in the early 20th century. Ankylosing Spondylitis affects millions worldwide, with its onset typically occurring in late adolescence or early adulthood. The prevalence varies globally, but it’s estimated that up to 0.1-0.5% of the adult population is affected, showing a higher prevalence in some ethnic groups and familial tendencies.
How It Is Generally Diagnosed
Diagnosing AS involves a combination of patient history, physical examinations, and medical imaging. Symptoms like chronic back pain and stiffness that improve with exercise but not with rest, and pain at night, are key indicators. Blood tests may be conducted to check for markers of inflammation and the presence of the HLA-B27 gene, which is commonly associated with AS. X-rays or MRI scans are used to detect changes in the joints and bones, though these signs often appear later in the disease progression. Early diagnosis and treatment are crucial for managing symptoms and preventing severe complications.
Symptoms of Ankylosing Spondylitis
It’s crucial for individuals to recognize its symptoms for early diagnosis and effective management.
Early Signs and Symptoms
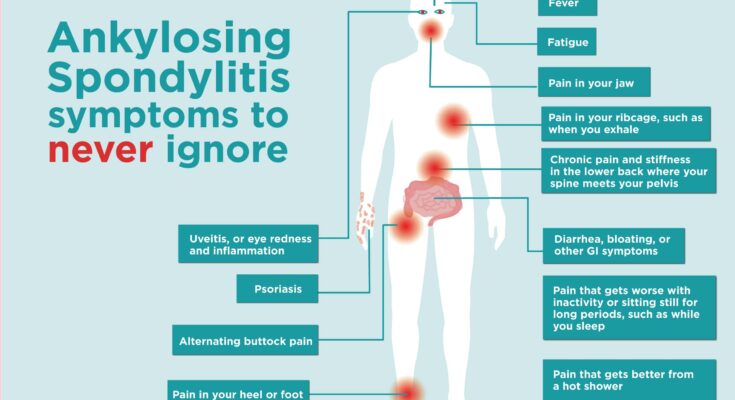
The initial signs of AS typically include:
- Pain and Stiffness in Lower Back and Hips: Often, individuals experience discomfort in these areas, particularly noticeable in the morning or after periods of inactivity.
- Morning Discomfort and Improvement with Exercise: The stiffness and pain are usually more pronounced in the morning and may decrease with physical activity or exercise.
Advanced Symptoms
As the condition progresses, other symptoms may emerge:
- Expansion of Pain: Pain may extend beyond the lower back and hips to other parts of the body, including the shoulders and ribs.
- Fatigue and Inflammation-Related Symptoms: Persistent fatigue is a common complaint, often accompanied by symptoms related to inflammation in the body.
Atypical Symptoms in Different Individuals
AS can manifest differently in individuals, making it vital to understand its variability:
- Variability in Symptom Presentation: Symptoms can vary widely from person to person, with some experiencing mild discomfort while others face severe pain and stiffness.
- Less Common Symptoms: Some individuals may experience atypical symptoms like eye inflammation, heart problems, or lung issues, though these are less common.
Identifying these symptoms early can lead to prompt and more effective treatment strategies. If you experience any of these signs, it’s advisable to consult a healthcare professional for proper diagnosis and management.
Causes of Ankylosing Spondylitis
Understanding these causes is vital for both patients and healthcare professionals.
Genetic Factors
- HLA-B27 Gene: A significant marker in AS, the HLA-B27 gene plays a crucial role. While not everyone with this gene develops AS, its presence increases the risk.
- Family History: Having a family member with AS or related conditions suggests a genetic predisposition, making this an essential factor in risk assessment.
Environmental Factors
- Chronic Infections: Some theories suggest that chronic infections might act as triggers for AS, although this is still a subject of ongoing research.
- Research Insights: Current studies are exploring various environmental factors, but there are no definitive conclusions yet, highlighting the need for further research.
Immune System’s Role
- Autoimmune Connection: AS is believed to have autoimmune components, where the immune system mistakenly attacks the body’s tissues.
- Current Understanding and Gaps: Researchers are actively investigating how the immune system contributes to AS, but there are still significant gaps in our understanding.
However, Ankylosing Spondylitis is a multifaceted disease with genetic, environmental, and immunological components. Ongoing research is essential to unravel its complexities and improve patient care.
Risk Factors for Developing Ankylosing Spondylitis
Ankylosing spondylitis (AS), a form of arthritis primarily affecting the spine, has several risk factors that individuals should be aware of. Understanding these factors can aid in early detection and management.
Age and Gender Dynamics
AS tends to develop in younger individuals, most commonly surfacing between late adolescence and early adulthood. This disease shows a notable prevalence in males compared to females. The age factor is crucial, as symptoms often begin in the late teens to early thirties. Recognizing AS early in this age range can lead to more effective management of the condition.
Genetic Predispositions
Genetics play a significant role in the likelihood of developing AS. The most notable genetic marker is the presence of the HLA-B27 gene. While having this gene doesn’t guarantee the development of AS, its presence significantly increases the risk. It’s important for individuals with a family history of AS, particularly those carrying the HLA-B27 gene, to be vigilant about symptoms.
Environmental Influences
Environmental factors, although less understood, also contribute to the risk of developing AS. Chronic inflammation triggered by certain environmental factors may play a role. These include prolonged exposure to particular occupational environments or certain gut bacteria, which might influence the onset of the disease. However, research in this area is still ongoing, and conclusive connections between environmental factors and AS are yet to be firmly established.
Complications Associated with Ankylosing Spondylitis
Physical Complications
This condition can lead to several physical complications, significantly impacting an individual’s health and lifestyle.
- Joint Damage and Osteoporosis: AS often results in the inflammation of the spinal joints, which can lead to severe joint damage over time. This damage can cause stiffness and pain, severely limiting mobility. Additionally, AS patients are at an increased risk of developing osteoporosis, a condition that weakens bones, making them more prone to fractures.
- Eye Inflammation (Uveitis): A notable complication of AS is eye inflammation, specifically uveitis. Uveitis can cause redness, pain, and blurred vision in the eyes. If left untreated, it may lead to further complications, including cataracts, glaucoma, and even loss of vision. Regular eye examinations are crucial for AS patients to monitor and manage this risk.
Mental Health Considerations
Living with Ankylosing Spondylitis can also have significant mental health implications, affecting patients’ overall quality of life.
- Impact on Quality of Life: The chronic pain and decreased mobility associated with AS can lead to restrictions in daily activities, affecting both personal and professional life. This can result in feelings of frustration, dependency, and decreased self-esteem.
- Mental Well-Being: The ongoing battle with pain, coupled with the challenges of managing a chronic illness, can lead to mental health issues such as anxiety and depression. It is essential for individuals with AS to seek support, whether through counseling, support groups, or mental health professionals, to cope with these challenges effectively.
However, while Ankylosing Spondylitis primarily affects physical health, its impact extends to mental well-being, highlighting the need for a holistic approach to treatment and management. Regular medical check-ups, mental health support, and a supportive community are vital in managing the complications associated with Ankylosing Spondylitis.
Diagnosis and Early Detection of Ankylosing Spondylitis
Emphasizing the Importance of Early Detection
Early detection of Ankylosing Spondylitis (AS) is crucial for managing symptoms and preventing the progression of the disease. Identifying AS in its initial stages can significantly improve the quality of life for patients, as it allows for timely intervention and more effective treatment strategies. This proactive approach not only helps in alleviating pain and stiffness but also minimizes the risk of long-term complications.
Diagnostic Methods: Imaging and Blood Tests
To diagnose AS, medical professionals rely on a combination of imaging and blood tests.
- Imaging: Advanced imaging techniques like X-rays, MRI (Magnetic Resonance Imaging), and CT (Computed Tomography) scans are instrumental in visualizing the extent of inflammation and structural changes in the spine and sacroiliac joints, which are typical in AS cases. These imaging modalities help in distinguishing AS from other forms of arthritis.
- Blood Tests: Blood tests play a supportive role in the diagnosis. They are used to detect inflammation markers such as C-reactive protein (CRP) and Erythrocyte Sedimentation Rate (ESR). Additionally, the presence of the HLA-B27 gene can be identified through blood tests, which is often associated with AS, though its absence does not rule out the disease.
Challenges in Diagnosing Ankylosing Spondylitis
Diagnosing AS poses several challenges:
- Symptom Overlap: The initial symptoms of AS, like lower back pain and stiffness, are common and can be mistaken for more mundane conditions, leading to delays in proper diagnosis.
- Variable Progression: The progression of AS varies significantly among individuals, making it hard to establish a standard diagnostic procedure.
- Absence of Definitive Tests: There is no single test that can definitively diagnose AS. A combination of medical history, physical examinations, imaging, and blood tests are required, making the diagnostic process complex.
However, early detection of Ankylosing Spondylitis is vital for effective treatment. While imaging and blood tests are key in the diagnostic process, the challenges in diagnosis highlight the need for increased awareness and understanding of the disease among both patients and healthcare providers.
Management and Treatment of Ankylosing Spondylitis
Ankylosing spondylitis (AS), a chronic inflammatory disease, primarily affects the spine and sacroiliac joints. Effective management involves a combination of non-pharmacological treatments, medications, and lifestyle modifications. This holistic approach helps in managing symptoms, improving functionality, and enhancing the quality of life for individuals with AS.
Non-Pharmacological Treatments
- Physical Therapy and Exercise: Tailored physical therapy and regular exercise are pivotal in managing AS. They aid in maintaining spinal flexibility, improving posture, and reducing pain. Therapists may recommend specific stretching and strengthening exercises tailored to individual needs.
Medications
- NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs) are the first line of pharmacological treatment for AS. They help reduce inflammation and alleviate pain. Regular monitoring is essential to manage potential side effects.
- Advanced Treatment Options: For cases not adequately controlled by NSAIDs, advanced treatments like biologics or disease-modifying anti-rheumatic drugs (DMARDs) may be prescribed. These medications target specific pathways in the immune system to reduce inflammation and prevent disease progression.
Lifestyle Modifications
- Diet: Adopting a healthy diet, potentially rich in omega-3 fatty acids, can help reduce inflammation. It’s advisable to avoid foods that can trigger inflammation.
- Exercise: Regular exercise, apart from physical therapy, is crucial. Activities like swimming, walking, and yoga can be beneficial.
- Daily Routine Adjustments: Making ergonomic adjustments in daily activities can help in managing symptoms. It includes adopting a good posture, using supportive chairs, and modifying activities to reduce strain on the back.
Proactive management of ankylosing spondylitis through these strategies can significantly improve the well-being and daily functioning of individuals affected by this condition. Regular consultations with healthcare providers are essential for personalized treatment and monitoring the effectiveness of the management plan.
Conclusion
It’s essential for anyone experiencing symptoms suggestive of AS to seek professional medical advice. Early diagnosis and appropriate treatment can greatly improve the quality of life and help manage the symptoms effectively. Remember, self-diagnosis and treatment can lead to complications; thus, professional guidance is indispensable.
Finally, there’s promising news on the horizon. Ongoing research in the field of rheumatology is continuously uncovering new insights about the disease, leading to more effective treatments and, potentially, preventive strategies. The future outlook for individuals with AS is becoming increasingly positive, thanks to advancements in medical research and improved understanding of the disease.
This brief overview of Ankylosing Spondylitis underlines the importance of awareness, timely medical consultation, and the hope that future research brings. Stay informed and proactive in seeking medical advice for a better quality of life.