Ankylosing Spondylitis Treatment: Ankylosing spondylitis (AS) is a chronic inflammatory disease that primarily affects the spine and sacroiliac joints, causing pain and stiffness. Over time, it can lead to a fusion of the spine, affecting posture and mobility.
This article provides an in-depth analysis of the diagnosis and treatment options for Ankylosing Spondylitis, guiding patients and caregivers through the journey of managing this condition.
What is Ankylosing Spondylitis?
Ankylosing Spondylitis (AS) is a chronic inflammatory disease primarily affecting the spine and sacroiliac joints, leading to pain and stiffness. Over time, it can cause the vertebrae in your spine to fuse, making the spine less flexible and potentially resulting in a hunched-forward posture. AS is part of the larger family of diseases called spondyloarthritis.
Epidemiology: Prevalence and Demographics
AS typically begins in early adulthood, with a higher prevalence in men compared to women. The exact prevalence varies globally, but it’s estimated to affect about 0.1% to 0.5% of the adult population. It’s more common in certain ethnic groups and has a strong genetic link, particularly associated with the HLA-B27 gene.
Risk Factors
- Genetic Factors: The presence of the HLA-B27 gene is the most significant risk factor. About 90% of individuals with AS have this gene.
- Age and Gender: AS commonly starts in late adolescence or early adulthood. Men are more frequently affected than women.
- Family History: A family history of AS increases an individual’s risk, pointing towards a hereditary aspect of the disease.
- Chronic Inflammation: Those with chronic inflammatory conditions may be at a higher risk of developing AS.
Understanding these risk factors can help in early detection and management of Ankylosing Spondylitis. It’s important for individuals who suspect they have AS to consult a healthcare professional for a proper diagnosis and treatment plan.
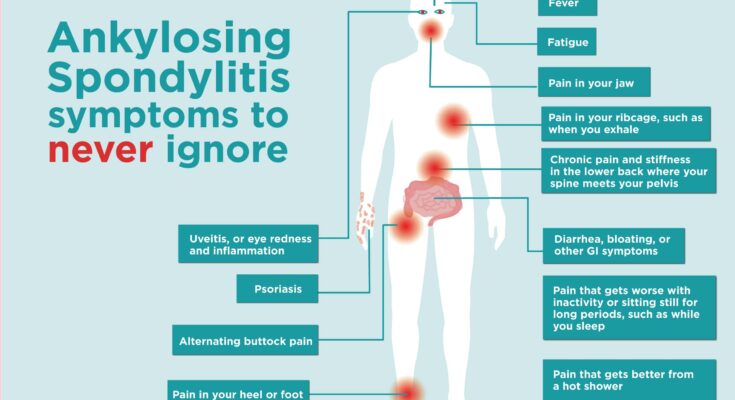
Symptoms and Early Signs of Ankylosing Spondylitis
Common Symptoms of Ankylosing Spondylitis (AS)
Ankylosing Spondylitis (AS) presents with specific symptoms that gradually evolve. Understanding these can aid in early diagnosis and management.
- Chronic Back Pain and Stiffness: Unlike ordinary back pain, AS typically causes discomfort in the lower back or buttocks, which worsens after periods of inactivity or during the night.
- Bony Fusion: AS can lead to the spinal bones fusing together, resulting in a rigid spine. This fusion can also affect the ribs, restricting lung capacity and function.
- Pain in Ligaments and Tendons: AS frequently affects the areas where ligaments and tendons attach to bones. Pain and stiffness in the heel, the soles of the feet, or around the knees are common.
- Fatigue: The chronic inflammation associated with AS often leads to general fatigue and tiredness.
- Eye Inflammation (Uveitis): Approximately 30% of people with AS experience eye inflammation, causing pain, sensitivity to light, and blurred vision.
Differentiating AS from Other Back Pain Conditions
AS is often mistaken for more common back pain issues due to early symptom similarities. However, certain characteristics distinguish AS:
- Age of Onset: AS symptoms usually begin in late adolescence or early adulthood.
- Pain Duration and Pattern: AS pain is persistent, lasting for more than three months. It improves with exercise but not with rest, which is contrary to many other back pain types.
- Inflammatory Nature: The pain in AS is due to inflammation, not just physical strain or injury.
Importance of Recognizing Early Signs
Identifying early signs of AS is crucial for several reasons:
- Preventing Severe Complications: Early diagnosis and treatment can prevent or delay spinal damage, including fusion.
- Improving Quality of Life: Timely intervention can significantly reduce pain and stiffness, improving daily function and quality of life.
- Monitoring Associated Conditions: People with AS are at increased risk of certain conditions like heart disease and inflammatory bowel disease. Early recognition allows for comprehensive care.
However, distinguishing the symptoms of Ankylosing Spondylitis from other back pain conditions is vital. Recognizing these early signs and seeking medical advice can lead to better outcomes and a healthier, more active life.
Diagnosis of Ankylosing Spondylitis
Understanding how to diagnose this condition is crucial for effective management and treatment.
Diagnostic Criteria for Ankylosing Spondylitis
The diagnosis of Ankylosing Spondylitis is based on a combination of clinical criteria and imaging findings. The most widely recognized criteria are the Modified New York Criteria, which include:
- Lower Back Pain and Stiffness: Persistent pain and stiffness in the lower back for more than three months, which improves with exercise but is not relieved by rest.
- Sacroiliitis on Imaging: Evidence of sacroiliitis (inflammation of the sacroiliac joint) on X-rays.
- Genetic Marker HLA-B27: The presence of the HLA-B27 gene, although its absence does not rule out AS.
Role of Medical History and Physical Examination
A thorough medical history and physical examination are fundamental in diagnosing AS. Key aspects include:
- Duration and Nature of Symptoms: Chronic back pain starting at a young age (typically under 45 years).
- Family History: A family history of AS or related conditions.
- Response to NSAIDs: A positive response to nonsteroidal anti-inflammatory drugs (NSAIDs) can support the diagnosis.
- Physical Findings: Reduced flexibility of the spine, limited chest expansion, and the presence of other symptoms like eye inflammation.
Imaging Tests in AS Diagnosis
Imaging is a cornerstone in the diagnosis of AS. X-rays of the spine and sacroiliac joints are usually the first step. However, these might not show early changes, and in such cases, MRI can be more useful. MRI is sensitive to early inflammatory changes and can detect sacroiliitis before it’s visible on X-rays.
Biomarkers in AS Diagnosis
While there is no specific blood test for AS, certain biomarkers can be helpful:
- HLA-B27 Testing: While not definitive, a positive HLA-B27 test increases the likelihood of AS, particularly in the presence of typical symptoms.
- Inflammatory Markers: Elevated levels of C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) can indicate inflammation, though they are not specific to AS.
Diagnosing Ankylosing Spondylitis involves a comprehensive approach, considering clinical history, physical examinations, imaging tests, and biomarkers. Early diagnosis and treatment are vital to managing symptoms and preventing complications. If you suspect you have symptoms of AS, consult with a healthcare provider for a thorough evaluation.
Treatment Options for Ankylosing Spondylitis
Here, we delve into the diverse treatment options available, emphasizing the importance of patient education and self-management in coping with this condition.
Non-Pharmacological Treatments for Ankylosing Spondylitis
- Physical Therapy: Tailored physical therapy is crucial in maintaining joint flexibility and posture. Regular sessions with a physical therapist can help alleviate stiffness and pain.
- Exercise: Regular exercise, including stretching and strengthening routines, plays a key role in managing symptoms and maintaining spinal mobility.
- Lifestyle Changes: Modifying daily activities and incorporating ergonomic practices at work and home can significantly reduce strain on affected joints.
Pharmacological Treatments for Ankylosing Spondylitis
- NSAIDs (Nonsteroidal Anti-Inflammatory Drugs): NSAIDs are often the first line of pharmacological treatment, offering relief from pain and inflammation.
- DMARDs (Disease-Modifying Antirheumatic Drugs): DMARDs, including sulfasalazine, can be used in cases where NSAIDs are insufficient.
- Biologics: Biologic agents, like TNF inhibitors, have transformed the management of AS, especially for those with severe symptoms.
- New Therapies: Ongoing research is continuously leading to the development of new medications, offering hope for improved treatment outcomes.
Emphasizing Patient Education and Self-Management
Educating patients about AS and its management is vital. Understanding the disease process, treatment options, and the importance of adherence to therapy empowers patients to take an active role in their care. Self-management techniques, including stress management and diet modifications, can also play a significant role in managing AS.
Living with Ankylosing Spondylitis: A Comprehensive Guide
Managing Day-to-Day Life with Ankylosing Spondylitis (AS)
Living with Ankylosing Spondylitis (AS) presents unique challenges in daily life. Adapting to these challenges is crucial for maintaining a good quality of life. It’s important to focus on:
- Effective Pain Management: Regular consultations with healthcare providers to manage pain through medication, physical therapy, or alternative therapies.
- Exercise and Physical Activity: Incorporating low-impact exercises like swimming, yoga, or walking can help maintain flexibility and reduce stiffness.
- Posture and Ergonomics: Adopting correct posture and ergonomic practices at work and home to minimize stress on the spine.
- Diet and Nutrition: Following a balanced diet, possibly with anti-inflammatory foods, can support overall health and potentially reduce symptoms.
- Mental Health: Addressing the emotional and psychological impact of AS through counseling, support groups, or mindfulness practices.
Long-Term Outlook and Quality of Life with AS
The long-term outlook for individuals with AS varies. Advances in treatments have improved the prognosis significantly. Key factors in managing long-term quality of life include:
- Regular Medical Care: Ongoing monitoring and treatment adjustments with a healthcare team.
- Lifestyle Adjustments: Making sustainable lifestyle changes to accommodate the condition.
- Awareness of Comorbid Conditions: Being vigilant about related health issues like cardiovascular diseases or osteoporosis.
- Staying Informed: Keeping up-to-date with the latest research and treatment options.
Support Systems and Resources for AS Patients
Building a strong support system is vital for those living with AS. Resources include:
- Support Groups: Joining AS-specific support groups, either in-person or online, for shared experiences and advice.
- Educational Resources: Utilizing materials from reputable health organizations for accurate information about AS.
- Professional Help: Seeking guidance from rheumatologists, physiotherapists, or mental health professionals specializing in chronic illnesses.
- Community Involvement: Participating in community events or advocacy groups to connect with others and raise awareness about AS.
However, while living with Ankylosing Spondylitis involves facing various challenges, effective management strategies, a supportive environment, and access to quality healthcare can significantly enhance the quality of life. Staying informed, proactive in care, and connected with a supportive community are key elements in navigating life with AS.
Preparing for your appointment
You might first bring your symptoms to the attention of your family health care provider. Your provider may refer you to a specialist in inflammatory disorders called a rheumatologist.
Here’s some information to help you get ready for your appointment.
What you can do
Make a list of:
- Your symptoms, including any that may seem unrelated to the reason you made the appointment, and when they began.
- Key personal information, including major stresses, recent life changes and family medical history.
- All medicines, vitamins and other supplements you take and their doses.
- Questions to ask your doctor.
Take a family member or friend along, if possible, to help you remember the information you’re given.
For ankylosing spondylitis, basic questions to ask your health care team include:
- What’s likely causing my symptoms?
- Other than the most likely cause, what are other possible causes for my symptoms?
- What tests do I need?
- Is my condition likely temporary or lifelong?
- What’s the best course of action?
- What are the alternatives to the primary approach you’re suggesting?
- I have other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Should I see a specialist?
- Are there brochures or other printed material I can have? What websites do you recommend?
What to expect from your doctor
Your doctor is likely to ask you questions, such as:
- Where is your pain?
- How severe is your pain?
- Have your symptoms been continuous or occasional?
- What, if anything, seems to worsen or improve your symptoms?
- Have you taken medicines to relieve the pain? What helped most?
Conclusion
To empower individuals with AS, ongoing patient education and self-advocacy are paramount. Patients should actively seek information about their condition, treatment options, and lifestyle choices that can positively impact their well-being. By becoming informed advocates for their own health, AS patients can collaborate effectively with healthcare professionals and make informed decisions about their care.
In conclusion, the journey of living with Ankylosing Spondylitis is marked by hope, progress, and the potential for improved quality of life. With continued research, clinical trials, and patient empowerment, the outlook for individuals with AS is brighter than ever. Together, we can strive for a future where AS is better understood, effectively treated, and ultimately, no longer a barrier to living life to the fullest.