Angina Symptoms: Angina pectoris, commonly known as angina, is a medical condition characterized by chest pain or discomfort, typically triggered by physical exertion or stress. It’s a symptom of an underlying heart problem, usually coronary heart disease (CHD).
Understanding the symptoms and causes of angina is crucial for early diagnosis and effective management.
What is Angina?
Angina is a term that often surfaces in discussions about heart health, but what exactly is it? At its core, angina refers to chest pain or discomfort caused by reduced blood flow to the heart muscle. This condition is a symptom of an underlying heart problem, usually coronary heart disease (CHD).
Types of Angina
Angina is classified into three primary types, each with distinct characteristics:
- Stable Angina: The most common form, stable angina, occurs when the heart is working harder than usual, such as during exercise. It has a predictable pattern and can be managed with medication and lifestyle changes.
- Unstable Angina: This type is more concerning. Unstable angina is unpredictable and occurs at rest. It’s a sign that a heart attack could happen soon and requires immediate medical attention.
- Variant (Prinzmetal’s) Angina: Less common, this type occurs at rest and is due to a spasm in a coronary artery. It can be painful and usually happens during the night or early morning hours.
Prevalence and Risk Factors
Angina is a fairly prevalent condition, especially in older adults. It’s a key symptom of heart disease, which is one of the leading causes of death worldwide. Risk factors for angina include high blood pressure, high cholesterol, smoking, diabetes, a sedentary lifestyle, and a family history of heart disease. Understanding these risks is crucial for prevention and management.
However, angina is not a disease in itself but a critical symptom of potential heart problems. Recognizing the types of angina and being aware of the risk factors are important steps in maintaining heart health. If you experience chest pain or discomfort, it’s essential to consult a healthcare provider for a proper diagnosis and treatment plan.
Angina Symptoms
This comprehensive guide aims to enhance your understanding of angina symptoms, helping you distinguish them from other cardiac conditions and identify when immediate medical attention is necessary.
Common Angina Symptoms
- Chest Pain or Discomfort: The hallmark of angina is a feeling of pain or discomfort in the chest, often described as squeezing, pressure, heaviness, or tightness.
- Radiating Pain: This discomfort may radiate to the arms, neck, jaw, shoulder, or back.
- Shortness of Breath: Many individuals experience breathlessness alongside chest discomfort.
- Other Symptoms: Nausea, fatigue, dizziness, and sweating can also accompany angina.
Differentiating Symptoms of Angina from Other Cardiac Conditions
- Stable vs. Unstable Angina: Stable angina is predictable and occurs during physical exertion or stress, while unstable angina is unexpected and more alarming.
- Intensity and Duration: Angina pain typically lasts for a few minutes and is alleviated by rest or medication. This differs from heart attack symptoms, which are more intense and prolonged.
- Trigger Factors: Angina is often triggered by physical activity or emotional stress, unlike heart attacks which can occur without a trigger.
Symptoms That Warrant Immediate Medical Attention
- Sudden Intense Chest Pain: If the chest pain is severe and doesn’t subside with rest, it’s critical to seek immediate medical help.
- Long-Lasting Discomfort: Pain or discomfort lasting more than a few minutes and not relieved by angina medications should be treated as a medical emergency.
- Accompanied by Other Symptoms: If chest pain is accompanied by shortness of breath, sweating, nausea, or fainting, it’s essential to call emergency services right away.
Understanding these symptoms is key in managing angina and preventing potential cardiac complications. Always consult with a healthcare professional for an accurate diagnosis and appropriate treatment plan. This knowledge not only empowers you to take charge of your health but also ensures you’re prepared to act swiftly in case of a cardiac emergency.
Causes of Angina
Understanding the causes of angina is essential for both prevention and treatment. Angina, a symptom of coronary artery disease, occurs when the heart muscle doesn’t receive enough oxygen-rich blood. This section delves into the various factors that contribute to the development of angina, offering insight into heart conditions, risk factors, and lifestyle influences.
Heart Conditions Leading to Angina
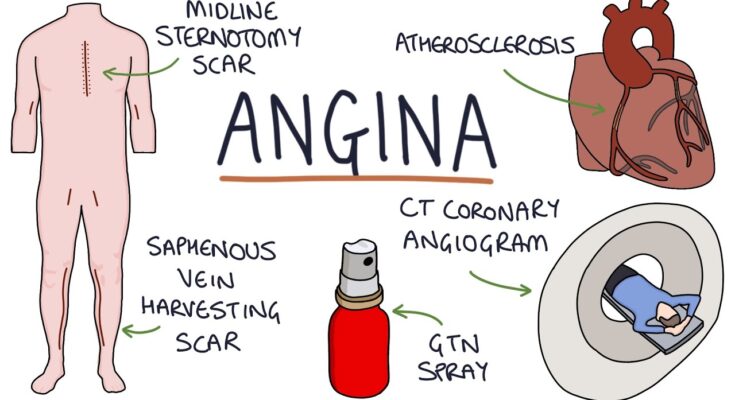
The heart, a vital organ, requires a constant supply of oxygen-rich blood to function effectively. Angina typically arises when the coronary arteries, responsible for supplying blood to the heart, become narrowed or blocked. This condition, often due to atherosclerosis (the buildup of plaques in the artery walls), restricts blood flow. Understanding this mechanism is crucial in grasping how heart conditions lead to angina. Other heart-related issues, such as irregular heart rhythms or heart valve diseases, can also contribute to the onset of angina by affecting the heart’s efficiency.
Risk Factors Contributing to Angina
Certain risk factors increase the likelihood of developing angina. These include:
- Age: The risk increases with age, particularly over 45 for men and 55 for women.
- Family History: A family history of heart disease elevates the risk.
- High Blood Pressure: This can cause hardening and thickening of arteries, limiting blood flow.
- High Cholesterol Levels: High levels of cholesterol in the blood can contribute to the formation of plaques and atherosclerosis.
- Diabetes: Diabetes is associated with an increased risk of angina and heart diseases due to its impact on blood vessels.
- Smoking: Smoking damages the interior walls of arteries and promotes plaque buildup.
Lifestyle and Environmental Factors
Lifestyle choices and environmental factors play a significant role in the development and management of angina. Key aspects include:
- Diet: A diet high in saturated fats, trans fats, salt, and cholesterol can contribute to the development of heart disease and angina.
- Physical Activity: Lack of regular exercise can contribute to obesity and high blood pressure, leading to angina.
- Stress: Chronic stress may damage arteries and worsen other risk factors for heart disease.
- Alcohol Consumption: Excessive alcohol intake can lead to high blood pressure, heart failure, and increased caloric intake, contributing to angina.
Understanding these factors is crucial in managing and preventing angina. Lifestyle modifications, along with medical treatment, can significantly reduce the risk and impact of angina, leading to a healthier heart and overall well-being.
Diagnosis of Angina: A Comprehensive Guide
Understanding the diagnosis of angina is crucial for effective management and treatment. This guide offers an in-depth look into the process of diagnosing angina, ensuring clarity and accessibility for all readers.
Initial Consultation and History Taking
The journey to diagnosing angina begins with a detailed patient history. During the initial consultation, healthcare providers focus on understanding the patient’s symptoms, lifestyle, and medical history. Key areas of inquiry include:
- Symptom Analysis: Identifying chest pain characteristics, such as onset, duration, and triggers.
- Medical and Family History: Exploring past health issues and family history of heart disease.
- Lifestyle Assessment: Evaluating factors like diet, exercise, and stress levels.
Physical Examination
A thorough physical examination follows the initial consultation. This step involves:
- Checking Vital Signs: Monitoring blood pressure, heart rate, and respiratory rate.
- Heart and Lung Examination: Listening for any abnormal heart sounds or breathing difficulties.
Diagnostic Testing
To confirm a diagnosis of angina, several diagnostic tests may be employed:
- Electrocardiogram (ECG): This test records the heart’s electrical activity, identifying any irregularities that might suggest angina.
- Stress Testing: Patients undergo physical exertion while their heart activity is monitored to observe how the heart responds under stress.
- Echocardiogram: This ultrasound test provides images of the heart’s structure and function.
- Blood Tests: These can identify markers that indicate heart damage or risk factors for heart disease.
- Coronary Angiography: A more invasive test, this involves using dye and X-rays to view the heart’s blood vessels.
Interpreting Results
After conducting these tests, healthcare professionals analyze the results to determine the presence and severity of angina. This step is vital in formulating an effective treatment plan.
The diagnosis of angina is a multifaceted process involving patient history, physical examination, and various diagnostic tests. Understanding this process can empower patients and caregivers, leading to better health outcomes and management of this condition.
Managing and Treating Angina
Managing and treating angina effectively involves a combination of medical treatments, lifestyle modifications, and timely medical intervention. This comprehensive approach aims to alleviate symptoms, improve the quality of life, and prevent the progression of the condition.
Common Treatments and Medications for Managing Angina
Medications: Key medications include:
- Nitrates (like nitroglycerin) to relieve chest pain.
- Beta-blockers to decrease heart workload and lower blood pressure.
- Calcium channel blockers to relax blood vessels.
- Statins to lower cholesterol levels.
- Aspirin to prevent blood clots.
Medical Procedures: In more severe cases, procedures like angioplasty, stenting, or coronary artery bypass grafting (CABG) may be necessary.
Lifestyle Changes and Home Remedies to Alleviate Symptoms
- Healthy Diet: Eating heart-healthy foods, reducing salt intake, and avoiding large meals can help manage angina.
- Regular Exercise: Under a doctor’s guidance, regular physical activity can strengthen the heart.
- Stress Management: Techniques like deep breathing, meditation, or yoga can reduce stress, a known trigger for angina attacks.
- Quitting Smoking and Limiting Alcohol: Smoking cessation and moderate alcohol consumption are crucial in managing angina.
- Maintaining a Healthy Weight: Losing weight if overweight can reduce the burden on the heart.
When to Seek Medical Intervention for Angina Management
- Persistent Symptoms: If chest pain or other symptoms persist despite medication, it’s crucial to seek medical advice.
- Worsening Symptoms: An increase in the frequency, duration, or intensity of symptoms is a sign to consult a healthcare provider.
- Emergency Situations: Severe chest pain, breathing difficulty, or symptoms resembling a heart attack require immediate medical attention.
However, managing and treating angina involves a multi-faceted approach, incorporating medical treatments, lifestyle adjustments, and being vigilant about changes in symptoms. Regular consultations with healthcare providers are essential to tailor treatment plans and ensure the best possible outcomes for individuals with angina.
Prevention Strategies for Angina: Essential Tips and Health Monitoring
Preventing angina involves managing risk factors and leading a heart-healthy lifestyle. Here, we discuss vital tips and strategies to prevent angina and emphasize the importance of regular health check-ups and heart monitoring.
1. Embrace a Heart-Healthy Diet
- Eat Balanced Meals: Focus on a diet rich in fruits, vegetables, whole grains, and lean proteins.
- Limit Unhealthy Fats: Reduce intake of saturated and trans fats to lower cholesterol levels.
- Control Salt and Sugar: Limiting salt and sugar helps in maintaining healthy blood pressure and weight.
2. Regular Physical Activity
- Stay Active: Engage in at least 30 minutes of moderate exercise most days of the week.
- Exercise Variety: Combine aerobic exercises, strength training, and flexibility workouts.
- Consult a Doctor: Always check with a healthcare professional before starting any new exercise regime, especially if you have existing health conditions.
3. Maintain a Healthy Weight
- Weight Management: Achieving and maintaining a healthy weight reduces the strain on your heart.
- Monitor BMI: Keep track of your Body Mass Index (BMI) and waist circumference.
4. Avoid Tobacco and Limit Alcohol
- No Smoking: Smoking is a major risk factor for heart disease. Quitting smoking can significantly reduce the risk of angina.
- Moderate Alcohol: Limit alcohol consumption as it can raise blood pressure.
5. Manage Stress
- Reduce Stress: Engage in stress-reducing activities like yoga, meditation, or deep breathing exercises.
- Seek Support: Talking to a professional or joining support groups can be beneficial.
6. Regular Health Check-Ups and Heart Monitoring
- Routine Check-Ups: Regular visits to your healthcare provider can help in early detection and management of risk factors.
- Blood Pressure and Cholesterol Checks: Keeping these under control is crucial for preventing angina.
- Heart Health Monitoring: Regular heart health assessments, including ECGs or stress tests, as recommended by your doctor.
Preventing angina involves a comprehensive approach that includes lifestyle changes, regular exercise, diet modifications, and consistent monitoring of heart health. Regular health check-ups play a critical role in detecting potential issues early and managing them effectively. By adopting these preventive strategies, you can significantly reduce your risk of angina and maintain a healthy heart.
FAQ Section: Understanding Angina
1. What is Angina?
Angina is a type of chest pain caused by reduced blood flow to the heart. It’s a symptom of coronary artery disease and is often described as squeezing, pressure, heaviness, or tightness in the chest.
2. What Causes Angina?
Angina is primarily caused by reduced blood flow to the heart muscle. This can result from coronary artery disease (where the arteries are narrowed or blocked), blood clots, or arterial spasms. Lifestyle factors like smoking, high cholesterol, and high blood pressure can increase the risk.
3. Are There Different Types of Angina?
Yes, there are several types of angina: stable angina (occurs during physical exertion and follows a predictable pattern), unstable angina (more unpredictable and can occur at rest), variant angina (occurs at rest due to a spasm in a coronary artery), and microvascular angina (affects the heart’s smallest coronary artery blood vessels).
4. What are Common Symptoms of Angina?
Common symptoms include chest pain or discomfort, pain in arms, neck, jaw, shoulder, or back accompanying chest pain, nausea, fatigue, shortness of breath, sweating, and dizziness.
5. How Can Angina be Differentiated from Other Types of Chest Pain?
Angina differs from other types of chest pain in its triggers and relief patterns. For instance, angina pain usually occurs with exertion and eases with rest, whereas other types of chest pain may not follow this pattern.
6. Is Angina a Sign of a Heart Attack?
Angina itself isn’t a heart attack, but it indicates an increased risk. Unstable angina, which can occur without any physical exertion and doesn’t go away with rest, may be a sign of an impending heart attack.
7. How is Angina Diagnosed?
Doctors typically perform a physical exam, review your symptoms and medical history, and may conduct several tests, such as an electrocardiogram (ECG), stress tests, blood tests, chest X-rays, coronary angiography, or CT scans.
8. Can Lifestyle Changes Help Manage Angina?
Yes, lifestyle changes can significantly help manage angina. These include quitting smoking, eating a heart-healthy diet, exercising regularly, maintaining a healthy weight, and managing stress.
9. Are There Treatments for Angina?
Treatment for angina includes lifestyle changes, medications (like nitrates, beta-blockers, statins, aspirin), and in some cases, medical procedures such as angioplasty and stent placement or coronary artery bypass surgery.
10. When Should You Seek Medical Help for Angina?
You should seek immediate medical attention if you experience unexplained chest pain or discomfort, especially if it’s a new symptom or different from previous episodes of angina.
Conclusion
It’s essential to recognize that angina serves as a warning sign of underlying heart problems. Therefore, if you experience symptoms consistent with angina, it’s crucial to seek medical advice promptly. Early diagnosis and treatment can significantly reduce the risk of more severe heart conditions, such as heart attacks.
Remember, heart health is paramount. Regular check-ups, a healthy lifestyle, and being aware of symptoms can go a long way in preventing and managing angina. If you’re experiencing any of the symptoms described above, don’t hesitate to consult a healthcare professional. Your heart deserves the utmost care and attention.