Anaphylaxis Symptoms: Anaphylaxis is a severe, potentially life-threatening allergic reaction that can occur rapidly, often within minutes of exposure to an allergen.
It requires immediate medical attention and can be frightening both for the person experiencing it and those around them.
In this article, we delve into the symptoms and causes of anaphylaxis, aiming to provide a detailed understanding of this medical emergency.
Understanding Anaphylaxis: Key Insights and Definitions
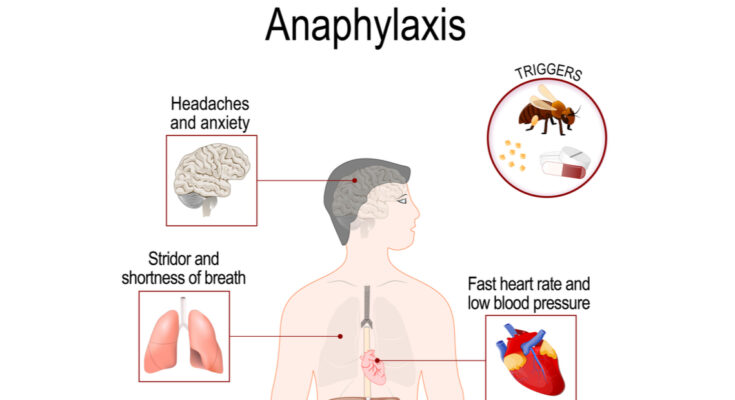
Anaphylaxis is a severe, potentially life-threatening allergic reaction that can occur rapidly and requires immediate medical attention. Unlike standard allergic reactions, anaphylaxis involves multiple body systems, including the skin, respiratory system, gastrointestinal tract, and cardiovascular system. It’s crucial to distinguish anaphylaxis from less severe allergic reactions due to its swift progression and intensity.
What Sets Anaphylaxis Apart from Other Allergic Reactions?
- Speed and Severity: Anaphylaxis typically develops quickly, often within minutes of exposure to an allergen, and can become life-threatening. This is much faster than common allergic reactions.
- Systemic Impact: While ordinary allergic reactions usually affect only one body system (like hives on the skin), anaphylaxis affects multiple systems simultaneously.
- Symptom Diversity: Symptoms of anaphylaxis can include difficulty breathing, hives, swelling, a rapid drop in blood pressure, and severe gastrointestinal symptoms. These are more diverse and severe than those of standard allergic reactions.
How Anaphylaxis Affects the Body
Anaphylaxis triggers an overwhelming immune response, releasing a flood of chemicals that can cause your body to go into shock. The airways can narrow, leading to wheezing and difficulty breathing. Blood pressure may plummet, leading to fainting or dizziness. Skin reactions, such as hives and swelling, can also occur. The gastrointestinal system might react with symptoms like vomiting or diarrhea. This multi-system involvement makes anaphylaxis a medical emergency.
Understanding the difference between anaphylaxis and more common allergic reactions is vital for both individuals and healthcare providers. Recognizing the signs can lead to quicker response times, potentially saving lives. If you suspect someone is experiencing anaphylaxis, seek emergency medical help immediately.
Symptoms of Anaphylaxis
Understanding its symptoms is crucial for prompt and effective treatment. This guide provides a comprehensive overview of the symptoms of anaphylaxis.
Primary Symptoms of Anaphylaxis
- Skin Reactions: One of the most common indicators, skin reactions include hives, itching, and flushed or pale skin.
- Swelling: This can occur in the face, lips, tongue, or throat, leading to difficulty in breathing or swallowing.
- Respiratory Symptoms: These include wheezing, shortness of breath, and a feeling of tightness in the chest.
- Cardiovascular Symptoms: Anaphylaxis can cause a significant drop in blood pressure, leading to dizziness, fainting, or a rapid heartbeat.
Less Common Symptoms
- Gastrointestinal Issues: Symptoms like nausea, vomiting, or diarrhea can also be associated with anaphylactic reactions.
- Neurological Symptoms: Confusion, headache, and a feeling of impending doom are less common but serious signs.
Timeline of Symptom Appearance
- Rapid Onset: Anaphylactic symptoms usually appear within minutes after exposure to the allergen.
- Delayed Reactions: In some cases, the symptoms can emerge hours after exposure, making vigilance crucial.
Variability Among Individuals
- Diverse Symptoms: The symptoms of anaphylaxis can vary greatly from person to person. Some might experience mild symptoms initially, while others may have severe reactions right away.
- Previous Reactions: Past reactions to allergens are not always predictive of future anaphylactic responses.
Understanding the various symptoms and their potential rapid onset is vital for anyone susceptible to severe allergic reactions. If you suspect anaphylaxis, seek immediate medical attention as it requires prompt treatment. Remember, each individual’s experience with anaphylaxis can differ, emphasizing the importance of personalized medical advice and intervention.
Common Causes of Anaphylaxis
Understanding the common triggers of anaphylaxis is crucial for both prevention and effective management. This article outlines the most prevalent allergens that can induce anaphylactic reactions, explains the underlying mechanisms of these reactions, and provides real-world examples to illustrate these triggers in action.
List of Most Common Allergens Triggering Anaphylaxis
Food Allergens: Foods are among the top culprits for anaphylactic reactions. Common food allergens include:
- Peanuts and tree nuts (like almonds, walnuts, and cashews)
- Shellfish (such as shrimp, lobster, and crab)
- Fish
- Milk and dairy products
- Eggs
- Soy
- Wheat
Insect Stings and Bites: Insect venom from stings or bites can cause anaphylaxis in sensitive individuals. The primary insects to be aware of are:
- Bees and wasps
- Hornets
- Yellow jackets
- Fire ants
Medications: Certain drugs can provoke anaphylactic reactions, including:
- Antibiotics, especially penicillins
- Nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin
- Anesthesia drugs
- Chemotherapy agents
Latex: Natural rubber latex found in medical gloves, balloons, and some types of medical equipment can trigger anaphylaxis in susceptible individuals.
How These Allergens Cause Anaphylaxis
When a person with allergies is exposed to a specific allergen, their immune system overreacts, mistaking the substance as harmful. This reaction leads to the release of chemicals like histamine, causing symptoms ranging from mild allergic reactions to severe anaphylaxis. Anaphylaxis symptoms can include difficulty breathing, hives, swelling, a rapid drop in blood pressure, and even loss of consciousness.
Case Studies and Examples
- Food-Induced Anaphylaxis: A case study highlighted a child with a peanut allergy who experienced anaphylaxis after consuming a cookie containing peanut traces. This incident underscores the importance of label reading and awareness for those with food allergies.
- Insect Sting-Triggered Anaphylaxis: Another example involves an adult who was stung by a bee and subsequently developed anaphylactic symptoms, necessitating emergency treatment. This case emphasizes the need for individuals allergic to insect stings to carry emergency medication like epinephrine auto-injectors.
- Medication-Related Anaphylaxis: A patient reported an anaphylactic reaction to penicillin, which they were unaware they were allergic to. This situation highlights the importance of allergy testing and communication with healthcare providers about potential allergies.
Understanding these common triggers of anaphylaxis and how they provoke reactions is essential for managing allergies and preventing serious consequences. Always consult a healthcare professional for personalized advice and treatment options.
Risk Factors for Anaphylaxis
Understanding the risk factors is crucial for prevention and preparedness. Here, we will delves into the various aspects that can increase the likelihood of experiencing anaphylaxis, including past allergic reactions, and the influence of genetic and environmental factors.
Previous Allergic Reactions: A Key Indicator
The history of allergic reactions plays a pivotal role in assessing the risk of anaphylaxis. Individuals who have experienced any form of allergy, especially severe reactions, are at a higher risk. This includes reactions to foods, insect stings, medications, or other allergens. Each allergic episode should be evaluated, as repeated exposures can escalate the severity of reactions, potentially leading to anaphylaxis.
Genetic Predisposition: The Inherited Risk
Genetics can also influence the likelihood of anaphylaxis. If immediate family members have a history of severe allergic reactions or related conditions like asthma, eczema, or hay fever, the risk is notably higher. This genetic link suggests that certain individuals are predisposed to more intense immune responses to allergens.
Environmental Influences: External Triggers
Environmental factors play a significant role in triggering anaphylaxis. These include exposure to specific allergens, such as certain foods (like peanuts, shellfish, eggs, and milk), insect stings (bees, wasps), latex, or certain medications. The risk is not limited to just these common triggers; almost any substance can potentially cause anaphylaxis in sensitive individuals.
Recognizing and understanding the risk factors for anaphylaxis is vital. Those with a history of allergies, a genetic predisposition, or exposure to environmental triggers should be particularly cautious. Awareness and preparedness, including carrying emergency medication like epinephrine, are key to managing this serious condition. Always consult healthcare professionals for personalized advice and treatment plans.
Diagnosing Anaphylaxis: A Comprehensive Guide
This article aims to provide a clear understanding of how to diagnose anaphylaxis.
Diagnostic Criteria for Anaphylaxis
Medical professionals use specific criteria to diagnose anaphylaxis. These criteria include:
- Rapid onset of symptoms: Symptoms typically develop within minutes to hours after exposure to an allergen.
- Involvement of multiple body systems: Anaphylaxis affects more than one part of the body, such as the skin, respiratory system, and circulatory system.
- Response to allergen exposure: A history of exposure to a known allergen significantly increases the likelihood of anaphylaxis.
Diagnostic Tests for Anaphylaxis
While there are no specific tests to diagnose anaphylaxis, certain tests can support the diagnosis:
- Blood tests: To measure levels of tryptase, which may increase during anaphylactic reactions.
- Skin tests: To identify specific allergens after recovery.
Medical History and Physical Examination
A detailed medical history and physical examination are vital. Doctors will inquire about:
- Past allergic reactions: Previous episodes can indicate a higher risk of anaphylaxis.
- Exposure to allergens: Information about recent exposures to foods, medications, or insect stings can be crucial.
Immediate Management and Referral
Prompt treatment is essential in suspected cases of anaphylaxis. Emergency management includes:
- Administration of epinephrine: The first line of treatment for anaphylaxis.
- Calling emergency services: Immediate medical attention is crucial.
After stabilization, referral to an allergy specialist for further evaluation and management is recommended.
Diagnosing anaphylaxis requires a swift and comprehensive approach, focusing on symptom recognition, medical history, and physical examination. While there are supportive tests, the immediate administration of epinephrine and emergency care are the priorities. Awareness and understanding of anaphylaxis can save lives, making this information critical for both healthcare providers and the general public.
Anaphylaxis Treatment and Management
Immediate Steps During an Anaphylactic Reaction
Anaphylaxis is a severe, potentially life-threatening allergic reaction that requires immediate action. The first step in managing an anaphylactic reaction is to recognize the symptoms, which may include difficulty breathing, swelling, hives, and a drop in blood pressure. If these symptoms are observed, it is crucial to act fast.
- Call Emergency Services: The first and most important step is to call for emergency medical help. Anaphylaxis is a medical emergency that requires immediate professional attention.
- Use an Epinephrine Auto-Injector: If the individual has a prescribed epinephrine auto-injector, use it immediately as directed. Epinephrine is the first-line treatment for anaphylaxis and can be life-saving.
- Lie Down and Raise Legs: Have the person lie flat on their back and raise their legs. This position helps maintain blood flow and can prevent shock.
- Administer CPR if Necessary: If the person is not breathing or their heart stops, administer CPR if you are trained to do so.
Medical Treatments for Anaphylaxis
Epinephrine is the primary treatment for anaphylaxis. However, additional medical treatments may be administered by healthcare professionals:
- Additional Doses of Epinephrine: In some cases, more than one dose of epinephrine may be necessary.
- Oxygen Therapy: To assist with breathing difficulties, oxygen may be provided.
- Intravenous Fluids: These may be administered to maintain blood pressure and treat shock.
- Antihistamines and Steroids: These can help manage and reduce allergic reaction symptoms.
Long-term Management for Those at Risk
For individuals at risk of anaphylaxis, long-term management strategies are vital:
- Avoid Known Allergens: Identifying and avoiding triggers is crucial. This may include certain foods, insect stings, medications, or other allergens.
- Carry an Epinephrine Auto-Injector: Always have an epinephrine auto-injector available and ensure that it is within its expiration date.
- Wear a Medical Alert Bracelet: This can inform others of your allergy in an emergency.
- Develop an Anaphylaxis Action Plan: Work with a healthcare provider to create a plan that outlines what to do in case of an allergic reaction.
- Regular Check-ups: Regular visits to an allergist or healthcare provider can help manage risks and update treatment strategies.
Remember, anaphylaxis is a medical emergency. Understanding the steps to take during an anaphylactic reaction and implementing long-term management strategies can be lifesaving for those at risk.
Prevention Strategies for Anaphylaxis
The cornerstone of these strategies is the identification and avoidance of known allergens. Here’s what you need to know:
- Identify Your Triggers: The first step in preventing anaphylaxis is to recognize the substances that trigger your allergic reactions. Common allergens include certain foods, medications, insect stings, and latex.
- Read Labels Carefully: For food allergies, it’s crucial to read ingredient labels meticulously. Be aware of food labeling laws and look out for hidden allergens in processed foods.
- Communicate Your Allergies: Always inform healthcare providers, restaurant staff, and others about your allergies to ensure safety in medical treatments and food preparations.
- Avoid Cross-Contamination: Be cautious about cross-contact in food preparation areas, especially when dining out or attending social events.
The Role of Allergy Testing and Desensitization Therapies
Understanding your allergies is a key component in prevention. Here’s how allergy testing and desensitization therapies can help:
- Allergy Testing: Consult an allergist for testing to determine specific allergens. Skin prick tests, blood tests, and oral food challenges are commonly used methods.
- Desensitization Therapies: For some allergies, desensitization (immunotherapy) can be effective. It involves gradually exposing the body to larger amounts of the allergen to build tolerance.
Importance of Emergency Preparedness
Being prepared for an allergic reaction is vital. Here are steps to ensure you’re ready:
- Carry Epinephrine: Always have an epinephrine auto-injector available. Know how to use it and make sure it’s within its expiration date.
- Wear Medical ID: Consider wearing a medical ID bracelet or necklace that details your allergies.
- Educate Yourself and Others: Be knowledgeable about the signs of anaphylaxis and educate those around you. Quick recognition and response can save lives.
- Have an Action Plan: Develop an allergy action plan with your healthcare provider. This should include steps to take in case of an allergic reaction.
By adopting these strategies, individuals with allergies can significantly reduce their risk of experiencing anaphylaxis and ensure they are prepared to handle it effectively if it occurs.
FAQs About Anaphylaxis
What is Anaphylaxis?
Anaphylaxis is a severe, potentially life-threatening allergic reaction. It can occur within seconds or minutes of exposure to something you’re allergic to, such as peanuts or bee stings.
How Common is Anaphylaxis?
Anaphylaxis is relatively rare, but its incidence is on the rise, particularly among children and young adults. Awareness and preparedness are key to managing this condition.
What Are the Symptoms of Anaphylaxis?
Symptoms can include a rapid, weak pulse, a skin rash, and nausea and vomiting. It’s important to recognize these symptoms early, as anaphylaxis requires immediate treatment.
Can Anaphylaxis Be Treated at Home?
Immediate treatment with an epinephrine auto-injector, such as an EpiPen, is crucial. However, this should be followed by emergency medical treatment. Home remedies are not sufficient for treating anaphylaxis.
Are There Long-Term Effects of Anaphylaxis?
Most people recover completely from anaphylaxis with proper treatment, but repeated episodes can have a more lasting impact on your health. Consulting with an allergist for long-term management is recommended.
Can Anaphylaxis Be Prevented?
Avoiding known allergens is the best way to prevent anaphylaxis. For those with severe allergies, carrying an epinephrine auto-injector and wearing a medical alert bracelet can be lifesaving.
Is Anaphylaxis a Sign of Other Allergies?
Experiencing anaphylaxis may indicate a severe allergy to specific triggers, and it’s a sign to get tested for other potential allergies.
Do Children Outgrow Anaphylaxis?
Some children may outgrow certain food allergies that can cause anaphylaxis, but this varies. Regular allergy testing and consultation with an allergist are important.
What Lifestyle Changes Can Help Manage Anaphylaxis?
Being aware of your triggers and educating those around you, including at schools and workplaces, can help manage anaphylaxis. Dietary modifications and having emergency action plans are also crucial.
Are There Misconceptions About Anaphylaxis?
A common misconception is that mild allergies can’t lead to anaphylaxis. Any allergy has the potential to become severe, so it’s important to take all allergies seriously.
Conclusion
While this article serves as a valuable resource for understanding anaphylaxis, it’s important to remember that personalized medical advice is crucial. Each individual’s situation is unique, and what works for one person may not be suitable for another.
Therefore, we strongly encourage our readers to consult healthcare professionals for tailored advice and guidance. These experts can provide individual assessments and recommend specific strategies for managing anaphylaxis, ensuring the best possible care.
In conclusion, arming yourself with knowledge about anaphylaxis and seeking professional medical advice are key steps in effectively managing this condition. Remember, awareness is your first line of defense, and professional guidance is your personalized shield in ensuring safety and well-being.