Anal Fistula Treatment: An anal fistula is a medical condition that can cause significant discomfort and requires effective management.
This article provides a comprehensive overview of the diagnosis and treatment of anal fistulas, aiming to offer valuable insights for those seeking in-depth understanding and effective solutions.
Understanding Anal Fistulas
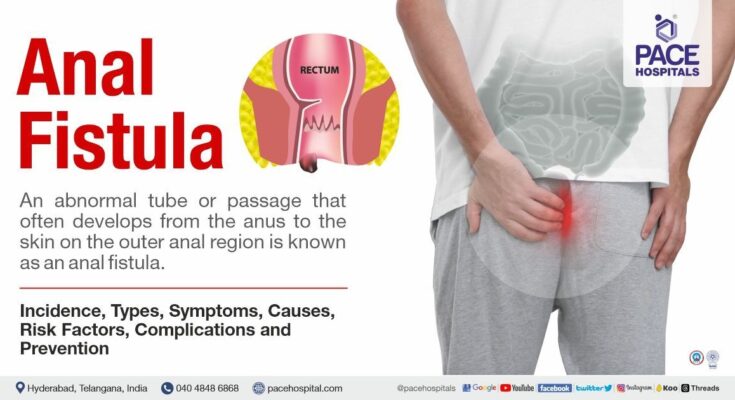
An anal fistula is a medical condition characterized by an abnormal connection between the epithelialized surface of the anal canal and the perianal skin. This tunnel-like formation is often a result of an infection near the anus, leading to an abscess that drains to the skin. Understanding its nature is crucial for effective treatment and management.
Causes and Risk Factors
Anal fistulas commonly arise from an anal abscess, a collection of pus near the anus, often due to infection in the anal glands. Certain conditions can increase the risk of developing anal fistulas, including:
- Inflammatory Bowel Disease (IBD): Conditions like Crohn’s disease and ulcerative colitis can cause inflammation of the digestive tract, leading to fistulas.
- Infections: Bacterial, fungal, or viral infections can lead to abscess formation and subsequent fistula.
- Surgery: Previous anal surgery can predispose to fistula formation.
- Trauma: Injury to the anal area can lead to fistula development.
- Other Risk Factors: Conditions like tuberculosis, cancer, or radiation therapy near the anal area.
Symptoms to Be Aware Of
Recognizing the signs and symptoms of an anal fistula can lead to early diagnosis and treatment, which is critical for reducing complications. Key symptoms include:
- Pain and Discomfort: Persistent pain in the anal area, which may worsen when sitting.
- Swelling and Redness: Around the anus, indicating inflammation or infection.
- Discharge: Pus or blood discharge from an opening near the anus.
- Fever: A sign of infection that may accompany an anal fistula.
Early detection and treatment are vital in managing anal fistulas effectively. Understanding these aspects can help in preventing serious complications and improve outcomes for those affected.
Diagnosis of Anal Fistulas
Initial Assessment and When to See a Doctor
When it comes to the diagnosis of anal fistulas, understanding when to seek medical attention is crucial. The initial assessment typically starts with recognizing symptoms such as pain, swelling, and discharge near the anal area. These symptoms can often be mistaken for other conditions, so it’s essential to be vigilant. If you experience persistent or severe discomfort, it’s time to consult a healthcare professional. Early consultation can prevent complications and lead to more effective treatment.
Different Diagnostic Methods
1. Physical Examination: The first step in diagnosing an anal fistula is usually a thorough physical examination. Doctors look for external signs of the fistula and may also perform a digital rectal examination to feel for abnormalities.
2. Imaging Tests: Advanced diagnostic methods play a pivotal role. These may include:
- Anoscopy: A specialized instrument to view the inside of the anus and rectum.
- Ultrasound: Offers a detailed image of the fistula tract.
- Magnetic Resonance Imaging (MRI): Provides a comprehensive view of the fistula and surrounding tissues, helping in complex cases.
3. Other Tests: In some cases, additional tests like a fistulogram or endoanal ultrasound may be required for a clearer understanding of the fistula’s path.
Importance of a Thorough Diagnosis
A thorough diagnosis is imperative in the treatment of anal fistulas. Accurate identification of the fistula’s type, location, and any connection to the sphincter muscles is essential. This information guides the treatment plan, ensuring the most effective and minimally invasive approach. A detailed diagnosis also helps in avoiding recurrence and managing potential complications. Therefore, patients and doctors alike should prioritize a comprehensive diagnostic process to achieve the best possible outcomes.
Treatment Options for Anal Fistulas
The primary goal in treating anal fistulas is to effectively heal the fistula while maintaining the integrity of the anal sphincter muscles, thus preventing incontinence. Treatment choices depend on the complexity of the fistula and the patient’s overall health.
Non-Surgical Treatments
In certain cases, non-surgical options may be considered, especially for simple and superficial fistulas. These include:
- Antibiotics: Primarily used to treat infection associated with the fistula. However, they do not typically heal the fistula.
- Fibrin Glue Injection: A less invasive procedure involving the injection of a biodegradable glue into the fistula tract.
- Fistula Plug: Involves the placement of a biodegradable plug to block the fistula tract, promoting healing.
The effectiveness of non-surgical treatments can vary, and they are often less successful compared to surgical methods. They are typically recommended for patients who are at higher risk of incontinence from surgery.
Surgical Options and Procedures
Most anal fistulas require surgery for effective treatment. The choice of surgical procedure depends on the fistula’s complexity and the patient’s condition:
- Fistulotomy: The most common procedure, involving cutting open the entire length of the fistula to flush out contents and allow healing. It is highly effective but may not be suitable for fistulas that pass through significant amounts of sphincter muscle.
- Seton Placement: Used for complex fistulas. A seton (a thread) is placed through the fistula to help it drain and heal over time. Sometimes used as a step before other surgeries.
- Advancement Flap Procedures: Involves creating a flap of tissue to cover the internal fistula opening and is used for higher or more complicated fistulas.
- LIFT Procedure (Ligation of the Intersphincteric Fistula Tract): A newer technique that involves the ligation of the fistula from the intersphincteric space.
The choice of surgical treatment is tailored to each patient, focusing on maximizing healing while minimizing the risk of incontinence.
Advanced Treatment Techniques for Anal Fistula
In recent years, the advancement in medical science has introduced innovative and less invasive treatment techniques that are transforming patient care. This article delves into these cutting-edge methods, emphasizing the role of technology and innovation in treating anal fistulas.
Embracing Minimally Invasive Approaches
- Fistula Laser Closure (FiLaC™): This modern technique utilizes laser energy to seal the fistula tract. The precision of laser technology allows for targeted treatment, minimizing damage to surrounding tissues. This approach is notable for its reduced recovery time and lower recurrence rates compared to traditional methods.
- Video-Assisted Anal Fistula Treatment (VAAFT): VAAFT combines a minimally invasive approach with the precision of endoscopic technology. By providing a direct view inside the fistula tract, surgeons can accurately identify the internal opening and treat the fistula with greater precision. This method reduces post-operative pain and speeds up recovery.
The Role of Bio-Technological Innovations
- Stem Cell Therapy: Stem cells offer a revolutionary approach in treating anal fistulas, particularly in complex cases. By harnessing the regenerative potential of stem cells, this therapy can promote healing from within, reducing the need for extensive surgical intervention.
- Bioprosthetic Plugs: Bioprosthetic plugs, made from biocompatible materials, are used to block and heal the fistula tract. They encourage tissue growth around the plug, leading to the natural closure of the fistula. This method stands out for its minimal invasiveness and effectiveness in certain types of fistulas.
Technology Integration for Enhanced Outcomes
- 3D Imaging and Modeling: The integration of 3D imaging in preoperative planning has revolutionized fistula surgery. Surgeons can now create a detailed 3D model of the fistula tract, enabling precise surgical planning and reducing operative risks.
- Robotic Surgery: Robotic-assisted surgery is gaining traction in the realm of fistula treatment. The enhanced precision, flexibility, and control offered by robotic systems allow for more accurate and less invasive surgeries, potentially improving patient outcomes and reducing recovery times.
The advent of these advanced treatment techniques marks a significant leap in the management of anal fistulas. By embracing minimally invasive approaches, leveraging biotechnological innovations, and integrating cutting-edge technology, medical professionals can offer effective, patient-friendly treatments. These developments not only improve the quality of life for patients but also signify a remarkable progression in medical science and surgical techniques.
Post-Treatment Care and Management of Anal Fistula
After undergoing treatment for an anal fistula, it’s crucial to follow specific care guidelines to ensure a smooth recovery and prevent potential complications. This section provides essential advice on post-treatment care, lifestyle modifications, and monitoring for any signs of complications.
Guidelines for Post-Treatment Care and Recovery
- Follow Doctor’s Instructions: Adhere strictly to any care instructions provided by your healthcare provider. This may include wound care, medication schedules, and follow-up appointments.
- Wound Care: Keep the surgical area clean and dry. Follow instructions for dressing changes and wound cleaning to prevent infection.
- Pain Management: Use prescribed pain relief medications as directed. If you experience increased pain, contact your healthcare provider.
- Dietary Adjustments: Incorporate high-fiber foods into your diet to ease bowel movements. Stay hydrated to prevent constipation.
- Activity Level: Gradually resume normal activities as recommended by your doctor. Avoid strenuous activities until fully recovered.
Lifestyle Changes and Home Care Tips
- Maintain Hygiene: Regular bathing and gentle cleaning of the anal area are important to prevent infection.
- Exercise Regularly: Engage in light exercise like walking to promote healing and bowel regularity.
- Avoid Straining: Do not strain during bowel movements. Use stool softeners if recommended by your doctor.
- Sitz Baths: Consider sitz baths to reduce discomfort and aid healing. Soak the affected area in warm water several times a day.
- Healthy Diet: Focus on a balanced diet rich in fruits, vegetables, and whole grains to support recovery.
Monitoring and Managing Potential Complications
- Infection Signs: Watch for signs of infection such as increased pain, redness, or discharge from the surgical site.
- Bowel Movements: Monitor your bowel movements. Report any significant changes or difficulties to your healthcare provider.
- Regular Check-Ups: Attend all scheduled follow-up appointments for proper monitoring of your recovery progress.
- Seek Immediate Help: If you experience severe pain, fever, or unusual symptoms, seek immediate medical attention.
By following these guidelines, patients can effectively manage their recovery from an anal fistula treatment and reduce the risk of complications. Remember, every individual’s recovery process is unique, so it’s important to maintain open communication with your healthcare team for personalized advice.
Prevention and Long-term Management of Anal Fistulas
1. Prevention of Anal Fistulas
Preventing anal fistulas largely revolves around maintaining good anal and overall health. Here are key tips:
- Maintain Proper Hygiene: Regular and thorough cleaning of the anal area can prevent infections that may lead to fistulas.
- Healthy Diet: A diet rich in fiber helps in smooth bowel movements, reducing the risk of constipation and subsequent strain that can lead to anorectal problems.
- Adequate Fluid Intake: Drinking plenty of water is essential to prevent constipation, a risk factor for the development of anal fistulas.
- Regular Exercise: Physical activity helps in maintaining a healthy bowel function.
- Avoid Straining: Overexertion during bowel movements can increase the risk of developing anal fistulas. It’s important to avoid straining.
- Prompt Treatment of Anorectal Disorders: Conditions like hemorrhoids, anal abscesses, and Crohn’s disease should be treated promptly to reduce the risk of fistulas.
2. Long-term Management Strategies for Those at Risk
For individuals at a higher risk of developing anal fistulas, long-term management is crucial. This includes:
- Regular Medical Check-ups: Regular visits to a healthcare provider for those with chronic digestive issues or previous anorectal problems.
- Managing Underlying Conditions: Effective management of conditions like Crohn’s disease, diverticulitis, or previous anorectal infections can mitigate the risk of fistula formation.
- Dietary Adjustments: Continuous monitoring and adjustments of diet to ensure healthy bowel movements.
- Stress Management: Stress can aggravate digestive issues, so incorporating stress-reducing activities like yoga or meditation can be beneficial.
- Avoiding Certain Activities: Activities that put excessive strain on the anorectal area, like heavy lifting, should be avoided if possible.
- Smoking Cessation: Smoking can exacerbate digestive problems and should be avoided.
By implementing these prevention and long-term management strategies, individuals can significantly reduce their risk of developing anal fistulas and maintain a healthier digestive system.
FAQs About Anal Fistula Treatment
Our goal is to enhance understanding and ease concerns by offering reliable information in an accessible format.
What is an Anal Fistula?
An anal fistula is a small tunnel that forms between the end of the bowel and the skin near the anus. It’s often the result of an infection near the anal glands.
How is an Anal Fistula Diagnosed?
Diagnosis typically involves a physical examination. In some cases, additional tests like an MRI or ultrasound may be necessary to assess the fistula’s depth and direction.
What are the Treatment Options?
Treatment varies depending on the fistula’s complexity. Common methods include fistulotomy, seton placement, and advanced techniques like LIFT (ligation of the intersphincteric fistula tract) or flap procedures.
Is Surgery Always Necessary?
While surgery is the most common treatment, not every case requires it. Your doctor will recommend the best approach based on the fistula’s characteristics.
What Can I Expect After Surgery?
Post-surgery, you may experience some discomfort and discharge. Recovery time varies, but following your doctor’s advice on care and hygiene is crucial for healing.
Are There Any Risks or Complications?
As with any surgery, there are risks such as infection or incontinence. Discussing potential risks with your healthcare provider is important for informed decision-making.
How Can I Prevent an Anal Fistula?
Preventive measures include maintaining good hygiene, managing conditions like Crohn’s disease effectively, and treating anal abscesses promptly.
Can an Anal Fistula Heal on Its Own?
It’s unlikely for an anal fistula to heal by itself. Medical intervention is usually necessary to prevent infection and other complications.
What Lifestyle Changes Can Aid Recovery?
Eating a high-fiber diet, staying hydrated, and avoiding straining during bowel movements can aid in recovery and prevent future issues.
Where Can I Find More Information?
For more information, consult your healthcare provider or visit reputable medical websites.
Conclusion
Healthcare providers offer a range of treatments, tailored to the severity and specific characteristics of the fistula. These treatments may include medication, lifestyle adjustments, or surgical procedures, each designed to effectively address the condition and improve patient outcomes.
By consulting a medical expert, patients ensure they receive accurate diagnosis and appropriate treatment, minimizing risks and complications. This approach also provides the necessary support and guidance through the healing process, ensuring a safer and more effective recovery journey.
Remember, while information about anal fistula can be informative and useful, it is not a substitute for professional medical advice. Always consult a healthcare provider for diagnosis and treatment of any medical condition, including anal fistulas.
For those who may be experiencing symptoms or concerns related to this condition, prompt consultation with a medical professional is crucial. Early intervention not only aids in effective treatment but also helps in preventing complications associated with this condition. Prioritizing professional medical advice is the best step towards a healthy recovery and management of anal fistula.