Alcoholic Hepatitis Symptoms: Alcoholic hepatitis is a severe condition resulting from prolonged alcohol abuse. It is characterized by inflammation, swelling, and the destruction of liver cells.
This article aims to provide an in-depth understanding of the symptoms and causes of alcoholic hepatitis, offering valuable insights for those affected and their loved ones.
Understanding Alcoholic Hepatitis
Alcoholic hepatitis is a disease that stems from the excessive consumption of alcohol. The condition develops over years of heavy drinking, which gradually damages the liver, leading to inflammation and scarring (fibrosis). This liver damage can progress to cirrhosis, a late-stage liver disease.
Symptoms of Alcoholic Hepatitis
Let’s take an in-depth look at the common symptoms of alcoholic hepatitis, how they differ from other liver-related conditions, and the importance of early symptom recognition.
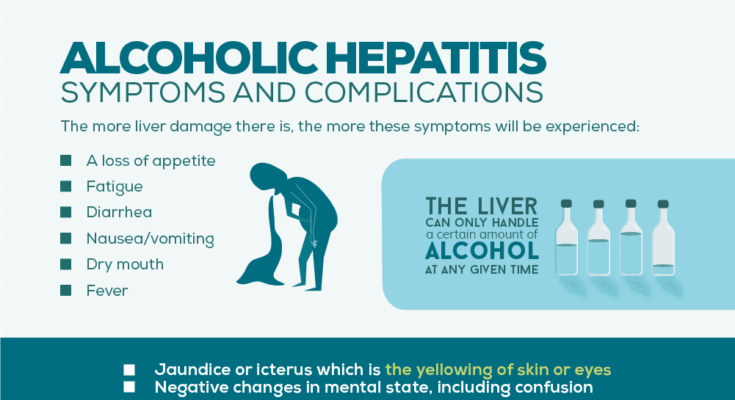
Common Symptoms of Alcoholic Hepatitis
- Jaundice: Yellowing of the skin and eyes, a classic sign differentiating alcoholic hepatitis from other liver conditions.
- Abdominal Pain and Swelling: Often localized in the upper right side, distinct from other liver issues which might cause diffuse abdominal discomfort.
- Nausea and Vomiting: Persistent and sometimes severe, differing in intensity from other liver diseases.
- Loss of Appetite: Leading to significant weight loss, a symptom that’s more acute in alcoholic hepatitis.
- Fatigue and Weakness: More pronounced than in other liver conditions.
- Fever: A symptom not always present in other liver diseases.
- Changes in Mental State: Including confusion and impaired judgment, often more severe than in other liver-related illnesses.
Differentiating Alcoholic Hepatitis from Other Liver Conditions
While some symptoms overlap with other liver diseases, certain aspects like the severity of jaundice, the pattern of abdominal pain, and specific changes in mental state are more characteristic of alcoholic hepatitis. Additionally, the presence of fever and the progression of symptoms can help distinguish it from other liver-related conditions.
The Importance of Early Symptom Recognition
Early detection of alcoholic hepatitis symptoms can lead to more effective treatment and a better prognosis. Understanding these symptoms and how they differ from other liver conditions is key to seeking timely medical intervention. Delay in recognizing and addressing these symptoms can lead to irreversible liver damage and other serious health complications.
Causes of Alcoholic Hepatitis
Understanding the causes of alcoholic hepatitis is essential for prevention and early intervention.
Alcohol Consumption: The primary cause of alcoholic hepatitis is the excessive and prolonged consumption of alcohol. Heavy drinking over an extended period can lead to liver damage.
Alcohol Metabolism: When alcohol is consumed, the liver metabolizes it. However, excessive alcohol overwhelms the liver’s capacity to process it, leading to inflammation and liver damage.
Genetic Factors: Some individuals may be genetically predisposed to a higher risk of developing alcoholic hepatitis. Family history and genetics can play a role in susceptibility.
Gender: Women are generally more susceptible to alcoholic hepatitis due to differences in alcohol metabolism and liver enzymes.
Amount and Duration: Both the amount of alcohol consumed and the duration of heavy drinking play a significant role. Long-term heavy drinkers are at a higher risk.
Nutritional Factors: Poor nutrition, often associated with heavy drinking, can exacerbate liver damage. Malnutrition can weaken the liver’s ability to recover.
Coexisting Liver Conditions: Individuals with pre-existing liver conditions, such as fatty liver disease, are at a higher risk of developing alcoholic hepatitis.
Age: Alcoholic hepatitis can occur at any age, but older individuals who have been heavy drinkers for a long time are more vulnerable.
Alcohol Type: The type of alcohol consumed, such as liquor, beer, or wine, can influence the risk of alcoholic hepatitis. Hard liquor tends to be more damaging.
Binge Drinking: Frequent episodes of binge drinking, even if not chronically heavy drinking, can contribute to the development of alcoholic hepatitis.
However, alcoholic hepatitis is primarily caused by prolonged and excessive alcohol consumption. However, genetic factors, gender, nutrition, and coexisting liver conditions can also influence an individual’s susceptibility. Understanding these causes is crucial for making informed choices about alcohol consumption and seeking medical help when needed.
Risk Factors for Alcoholic Hepatitis
Alcoholic hepatitis is a serious condition primarily affecting individuals who consume large amounts of alcohol. High-risk groups include:
- Heavy Drinkers: Those who regularly consume alcohol in large quantities are at the greatest risk.
- Genetic Predisposition: Individuals with a family history of alcohol-related liver disease.
- Co-existing Liver Conditions: People with pre-existing liver conditions like hepatitis B or C.
- Nutritional Deficiencies: Poor nutrition can exacerbate the effects of alcohol on the liver.
Understanding these risk groups is crucial for early detection and intervention.
Factors Increasing Likelihood of Developing Alcoholic Hepatitis
Several factors can heighten the risk of developing alcoholic hepatitis:
- Duration of Alcohol Consumption: Longer periods of heavy drinking significantly increase risk.
- Gender and Alcohol Metabolism: Women may be more susceptible due to differences in how alcohol is processed in the body.
- Age: Older individuals might have a higher risk due to cumulative effects of alcohol and decreased liver resilience.
- Binge Drinking: Episodes of heavy drinking can cause sudden and severe damage.
Awareness of these factors is key in assessing personal risk and making informed choices about alcohol consumption.
Preventive Measures and Lifestyle Recommendations
Preventing alcoholic hepatitis involves lifestyle changes and awareness:
- Moderate Alcohol Consumption: Adhering to recommended alcohol limits is essential.
- Healthy Diet: A balanced diet supports liver health and mitigates alcohol’s negative impact.
- Regular Medical Check-ups: Early detection of liver changes can prevent progression.
- Awareness and Education: Understanding the risks associated with excessive alcohol consumption.
By adopting these measures, individuals can significantly reduce their risk of developing alcoholic hepatitis.
Complications and Health Impacts of Alcoholic Hepatitis
It’s crucial to understand the potential complications and health impacts associated with this condition, as it affects not only the liver but also has widespread consequences for overall health.
Liver Cirrhosis: One of the most severe complications of alcoholic hepatitis is the progression to cirrhosis. This occurs when healthy liver tissue is replaced with scar tissue, severely impacting liver function. Cirrhosis can lead to a host of problems, including liver failure and the need for a liver transplant.
Increased Risk of Liver Cancer: Alcoholic hepatitis significantly raises the risk of developing liver cancer, a serious and potentially fatal condition. Regular monitoring and medical intervention are critical for individuals with a history of alcoholic hepatitis.
Ascites and Edema: Fluid retention in the abdomen (ascites) and swelling in the legs (edema) are common complications. These symptoms indicate advanced liver disease and require prompt medical attention.
Impaired Brain Function: The toxins that are normally filtered by the liver can build up in the body and affect the brain, leading to a condition called hepatic encephalopathy. This can result in confusion, changes in behavior, and even coma.
Malnutrition and Weight Loss: Alcoholic hepatitis can lead to malnutrition and significant weight loss, as the damaged liver struggles to process nutrients effectively.
Increased Bleeding Risks: The liver produces proteins that help your blood to clot. When it’s damaged, there’s a higher risk of bleeding, both internally and externally.
Other Systemic Impacts: The condition can also affect other organs and systems, leading to complications like kidney failure and susceptibility to infections.
Understanding these complications is vital for anyone dealing with alcoholic hepatitis. It underscores the importance of seeking prompt medical care and the need for lifestyle changes, primarily abstinence from alcohol, to mitigate these health risks.
Diagnosing Alcoholic Hepatitis
Here will guide you through the common diagnostic methods and tests, emphasizing the role of medical history and physical examination, and highlighting the importance of early and accurate diagnosis.
Common Diagnostic Methods and Tests
When suspecting alcoholic hepatitis, healthcare professionals utilize a variety of diagnostic tests. These typically include:
- Blood Tests: These are essential to check for elevated liver enzymes, which indicate liver damage. Complete blood counts and tests for liver function are standard.
- Imaging Tests: Ultrasound, CT scans, or MRI can be used to visualize the liver and assess the extent of damage.
- Liver Biopsy: In some cases, a biopsy is performed to confirm the diagnosis, where a small tissue sample from the liver is examined under a microscope.
Understanding these tests helps patients and their families comprehend the diagnostic process and prepares them for discussions with their healthcare providers.
The Role of Medical History and Physical Examination
A thorough medical history and physical examination are foundational in diagnosing alcoholic hepatitis. During this process, doctors will:
- Inquire about alcohol consumption habits to understand the potential cause of liver damage.
- Look for physical signs of liver disease, such as jaundice, enlarged liver, or fluid accumulation in the abdomen.
This comprehensive evaluation aids in ruling out other causes of liver disease and tailoring the most appropriate treatment plan.
Importance of Early and Accurate Diagnosis
Early and accurate diagnosis of alcoholic hepatitis is critical for several reasons:
- Prevents Progression: Early detection can prevent the disease from progressing to more severe stages like cirrhosis or liver failure.
- Guides Treatment: A timely and precise diagnosis allows for the implementation of effective treatment strategies, including lifestyle changes and medical interventions.
- Improves Prognosis: The sooner alcoholic hepatitis is diagnosed and treated, the better the chances of recovery and the lower the risk of complications.
In summary, diagnosing alcoholic hepatitis involves a combination of blood tests, imaging studies, and sometimes liver biopsy, underpinned by a thorough medical history and physical examination. Recognizing the importance of early and accurate diagnosis is key to managing this condition and improving patient outcomes.
By understanding these aspects, patients can engage more effectively in their healthcare and make informed decisions about their treatment and lifestyle modifications.
Treatment and Management of Alcoholic Hepatitis
The treatment and management of this condition require a multifaceted approach, focusing on both immediate medical intervention and long-term lifestyle modifications. Below are the key strategies for treating and managing alcoholic hepatitis:
Abstinence from Alcohol: The most crucial step in treating alcoholic hepatitis is the complete cessation of alcohol intake. This single action can significantly reduce liver inflammation and prevent further damage.
Nutritional Support: Patients with alcoholic hepatitis often suffer from malnutrition. A balanced diet, possibly supplemented with vitamins, particularly B vitamins, is essential for recovery and liver repair.
Medical Treatments: Depending on the severity, medications may be prescribed. These can include corticosteroids to reduce liver inflammation or pentoxifylline for severe cases.
Monitoring and Managing Complications: Regular monitoring for complications such as liver cirrhosis or failure is essential. In severe cases, a liver transplant may be considered.
Lifestyle Changes and Support: Long-term lifestyle changes, including maintaining a healthy diet, regular exercise, and avoiding alcohol, are vital. Support groups and counseling can also be beneficial in managing alcohol dependency.
Regular Medical Check-ups: Ongoing medical supervision is crucial to monitor liver function and overall health status, adjusting treatments as needed.
By implementing these strategies, individuals with alcoholic hepatitis can significantly improve their liver health and overall well-being. It’s essential to seek medical advice promptly if you suspect you or someone you know is suffering from this condition.
Prevention of Alcoholic Hepatitis
Alcoholic hepatitis is a serious liver condition caused by excessive alcohol consumption. Preventing it is crucial for maintaining liver health and overall well-being. Here’s a concise guide:
- Limit Alcohol Consumption: The most effective way to prevent alcoholic hepatitis is to limit or avoid alcohol. For those who drink, following recommended guidelines and reducing intake can significantly lower the risk.
- Healthy Diet and Exercise: A balanced diet rich in fruits, vegetables, and lean proteins, along with regular exercise, supports liver health and reduces the risk of liver diseases.
- Regular Health Check-ups: Regular medical check-ups help in early detection of any liver-related issues. This is particularly important for individuals with a history of alcohol use.
- Avoiding Risky Behaviors: Risky behaviors, like binge drinking or mixing alcohol with medications, can increase the likelihood of developing alcoholic hepatitis. Awareness and avoidance of these behaviors are crucial.
- Education and Support: Understanding the risks associated with excessive alcohol use, and seeking support from friends, family, or support groups can help in making healthier lifestyle choices.
- Vaccinations and Medications: In some cases, doctors may recommend vaccinations or medications to protect the liver from other potential harms.
By incorporating these strategies, individuals can significantly reduce their risk of developing alcoholic hepatitis. Remember, prevention is key to maintaining a healthy liver and overall health.
Conclusion
Prevention is always better than cure. Maintaining a healthy lifestyle, being mindful of alcohol consumption, and regular health check-ups play a significant role in preventing alcoholic hepatitis. We urge readers to take this information seriously, not only for their well-being but also for the benefit of their loved ones and the wider community.
By fostering awareness and advocating for early intervention, we can collectively make strides in managing and preventing alcoholic hepatitis. Let’s commit to a healthier future by embracing these principles in our daily lives.