Acute Flaccid Myelitis Treatment: Acute Flaccid Myelitis (AFM) is a rare but serious condition that affects the nervous system, specifically the area of the spinal cord called gray matter.
This condition leads to sudden and rapid muscle weakness and loss of muscle tone and reflexes. AFM is often preceded by a viral infection, making early diagnosis and treatment crucial for patient outcomes.
In this comprehensive guide, we explore the diagnostic process and treatment options for AFM, offering valuable insights for healthcare providers and patients alike.
Understanding the Symptoms of AFM
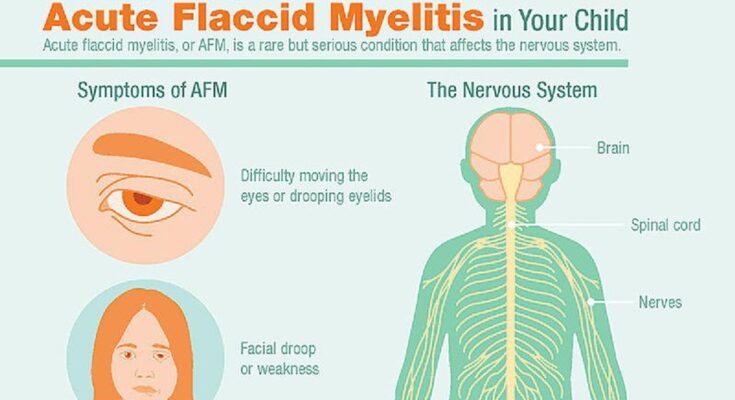
The onset of AFM is characterized by a sudden weakness in the arms or legs, loss of muscle tone, and absent reflexes. Additional signs can include facial drooping, difficulty moving the eyes, drooping eyelids, difficulty with swallowing, and slurred speech. Respiratory failure can occur in severe cases due to weakness of the respiratory muscles. Identifying these symptoms promptly can lead to a quicker diagnosis and more effective treatment.
Recognizing the Symptoms of Acute Flaccid Myelitis
The initial symptoms of AFM are similar to those of other viral illnesses and may include:
- Fever
- Respiratory illness
- Gastrointestinal issues
As AFM progresses, additional signs and symptoms may manifest, including:
- Facial droop/weakness
- Difficulty moving the eyes
- Drooping eyelids
- Difficulty with swallowing
- Slurred speech
In severe cases, AFM can lead to respiratory failure when the muscles involved with breathing become weakened. This is a medical emergency requiring immediate intervention.
Causes of Acute flaccid myelitis (AFM)
While the exact cause of AFM remains uncertain, epidemiologists have linked several factors to the condition:
- Viral infections, particularly those caused by enteroviruses such as EV-D68 and EV-A71, are the most commonly identified precedents of AFM.
- Environmental toxins and genetic disorders are also being explored as potential contributors to the development of AFM.
Prevention of Acute Flaccid Myelitis
There’s no specific way to prevent acute flaccid myelitis. However, preventing a viral infection can help reduce the risk of developing acute flaccid myelitis.
Take these steps to help protect yourself or your child from getting or spreading a viral infection:
- Wash your hands often with soap and water.
- Avoid touching your face with unwashed hands.
- Avoid close contact with people who are sick.
- Clean and disinfect frequently touched surfaces.
- Cover coughs and sneezes with a tissue or upper shirt sleeve.
- Keep sick children at home.
Diagnostic Approaches for Acute Flaccid Myelitis
To diagnose AFM, healthcare professionals rely on a combination of patient history, physical examination, and diagnostic tests. The process often includes:
- Magnetic Resonance Imaging (MRI): An MRI can detect inflammation and lesions on the spinal cord, which are indicative of AFM.
- Cerebrospinal Fluid (CSF) Analysis: A lumbar puncture is performed to collect a sample of CSF for analysis, which may show signs of inflammation consistent with AFM.
- Electromyography (EMG) and Nerve Conduction Studies: These tests measure the electrical activity of muscles and the speed of nerve signals, respectively, to determine the presence of nerve damage.
- Laboratory Tests: Blood tests and viral studies can help identify the presence of enteroviruses, which are commonly associated with AFM.
Treatment Strategies for Acute Flaccid Myelitis (AFM)
While there is no specific cure for AFM, treatment is focused on managing symptoms and supporting recovery. Treatment options may include:
- Physical and Occupational Therapy: To improve mobility and address muscle weakness, physical and occupational therapy are critical components of the rehabilitation process.
- Pain Management: Pain associated with AFM can be significant, and managing it is a key aspect of treatment.
- Respiratory Support: For patients experiencing respiratory weakness, support ranges from noninvasive ventilation to mechanical ventilation in more severe cases.
- Immunomodulatory Therapies: Although the effectiveness is still under study, treatments such as intravenous immunoglobulin (IVIG), corticosteroids, and plasma exchange (PLEX) have been used in an attempt to reduce inflammation and improve outcomes.
Navigating Challenges in AFM Recovery
The recovery from AFM can be a lengthy process, with some patients making a full recovery and others continuing to have residual weakness. Early and aggressive physical rehabilitation is crucial for maximizing recovery of function. In addition, psychological and emotional support for both patients and their families cannot be overstated, as AFM can be a traumatic experience with long-term implications.
Prevention and Awareness
While not all cases of AFM can be prevented, staying informed about the condition and practicing good hygiene can reduce the risk of enterovirus infections, which are often linked to AFM. This includes handwashing, avoiding close contact with sick individuals, and staying up to date with vaccinations.
FAQs About Acute Flaccid Myelitis Treatment
Below, we’ve compiled a list of common questions with expert answers to help guide you through understanding this condition.
What is the most effective treatment for AFM?
The treatment for AFM is primarily supportive, which means it focuses on managing symptoms and complications as there is no specific cure. Physical therapy and rehabilitation are crucial to improve muscle strength and function. In some cases, doctors may use medications to fight infections or inflammation that might trigger AFM.
Can AFM be cured completely?
Since AFM can be caused by a variety of factors, complete recovery can vary from person to person. Some individuals may recover quickly, while others may have lingering effects and require long-term treatment. Early intervention with physical therapy and rehabilitation offers the best chance for improvement.
Is physical therapy a long-term requirement for AFM patients?
Physical therapy is a cornerstone of AFM treatment and may be a long-term requirement for some. The duration depends on the severity of the condition and the rate of recovery. Regular assessments by healthcare providers help to tailor the therapy to the patient’s evolving needs.
Are there any new treatments being researched for AFM?
Researchers are continually exploring new treatments for AFM. This includes studies on antiviral drugs, immunoglobulin therapies, and interventions to boost the immune system. Clinical trials are also ongoing to evaluate the effectiveness of these potential treatments.
How do I find a specialist who can treat AFM?
Finding a specialist for AFM treatment involves seeking out a neurologist or a pediatric infectious disease specialist with experience in dealing with neuroimmunological disorders. Contacting national health organizations or hospitals with specialized neurology departments can be a good starting point.
Can vaccines prevent AFM?
Some instances of AFM are thought to be caused by viral infections, such as enterovirus D68. Staying up to date with vaccinations can protect against some of the viruses associated with AFM, thus potentially reducing the risk. It’s important to discuss vaccination options with a healthcare provider.
What supportive treatments are available for AFM?
Supportive treatments for AFM include respiratory therapy for those with breathing difficulties, pain management, and occupational therapy to help with daily activities. Mental health support is also important, as dealing with a chronic condition can be emotionally challenging.
How quickly should treatment for AFM start?
Treatment for AFM should begin as soon as possible after diagnosis. Early treatment can significantly affect the outcome and may improve the chances of recovery. If AFM is suspected, immediate medical attention is crucial.
Remember, every AFM case is unique, so treatment and recovery can vary greatly. It’s essential to work closely with a healthcare team to tailor the treatment plan to individual needs. If you have more questions or concerns about AFM treatment, don’t hesitate to reach out to a medical professional for personalized advice.
Conclusion
Early intervention is critical in the treatment of AFM. Immediate care from a team of experts can significantly affect outcomes, helping to manage symptoms and potentially mitigate long-term effects. Families and caregivers also play a pivotal role in the ongoing care and rehabilitation process, providing the essential support that complements medical interventions.
As research continues to advance, there is hope for new and improved treatment protocols. Meanwhile, the current focus remains on tailoring therapies to individual needs, ensuring the best possible support for those affected by this challenging condition.
In conclusion, understanding and addressing AFM through a multidisciplinary approach is crucial. It provides a holistic framework for treatment that can help patients navigate the complexities of AFM, maximizing their recovery potential and ensuring a better quality of life. With a cooperative strategy, healthcare providers can deliver targeted and effective care that speaks to the urgency and specificity of acute flaccid myelitis.