Acute Flaccid Myelitis (AFM) Treatment: In today’s digital age, health information is abundant, yet deciphering conditions and their implications can be challenging. One such condition, Acute Flaccid Myelitis (AFM), stands out in this spectrum.
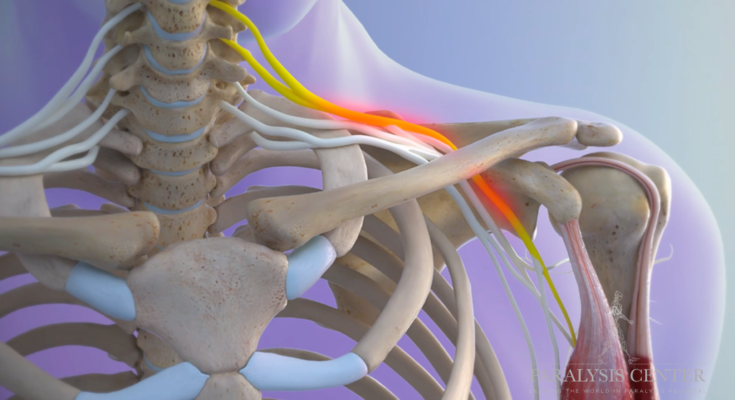
AFM is a rare, but severe, neurological disorder that primarily affects the spinal cord, causing muscles and reflexes in the body to weaken suddenly. The origins of AFM are not entirely known, but it is believed to be caused by a combination of various viruses and environmental factors.
The most striking feature of AFM is its rapid onset, which is why timely diagnosis and treatment are paramount. Delaying intervention can lead to worsening symptoms and long-term complications.
In this section, we’ll delve deeper into AFM, underscoring the vital importance of early detection and prompt medical attention.
What is Acute Flaccid Myelitis (AFM)?
Acute Flaccid Myelitis (AFM) is a rare but serious neurological condition that affects the spinal cord. It primarily manifests in sudden onset muscle weakness, often following a viral infection. Affected individuals may display symptoms ranging from drooping eyelids, difficulty in moving the eyes, difficulty swallowing, and slurred speech. The most severe cases can lead to respiratory failure, necessitating the use of ventilators.
Epidemiology: Prevalence and Risk Factors
The exact prevalence of AFM is still under investigation, but occurrences often show a spike every two years, predominantly in late summer and early fall. While AFM can affect individuals of all ages, children seem to be at a higher risk. A notable risk factor is a prior respiratory illness or fever, commonly from viral infections, although not every person with AFM has these preceding symptoms. Research is ongoing to determine other potential risk factors and underlying causes.
Differentiating AFM from Other Neurological Conditions
It’s vital to distinguish AFM from other neurological disorders, as the presentation can sometimes be similar. Key differentiators include:
- Rapid Onset: AFM typically has a sudden onset of muscle weakness.
- MRI Findings: Imaging studies of patients with AFM often show gray matter lesions in the spinal cord.
- No Known Unifying Cause: Unlike conditions with specific triggers (e.g., polio with the poliovirus), AFM doesn’t have a singular identified cause, even though it’s linked with several viruses.
Early and accurate diagnosis of AFM is crucial to manage and potentially mitigate its effects. If one suspects AFM, immediate medical attention should be sought, and healthcare providers should be informed of any recent illnesses or fevers.
Symptoms of Acute Flaccid Myelitis
Acute Flaccid Myelitis (AFM) is a rare but serious neurological condition that affects the spinal cord, primarily in children. Recognizing its symptoms early is crucial for timely intervention. Here’s a detailed look into its symptoms and how they may differ across various age groups and demographics:
Early Signs and Progression:
- Sudden Weakness in the Arms or Legs: One of the hallmark signs of AFM is a sudden onset of arm or leg weakness. This can occur in one or more limbs.
- Facial Droop or Weakness: This can include drooping of the eyelids or difficulty moving the eyes.
- Difficulty in Swallowing or Slurred Speech: Some individuals may find it hard to swallow or may begin to slur their words without a known reason.
- Pain in Limbs: Though less common, some may experience pain in the affected limb or limbs.
- Stiff Neck: A stiff neck can develop, making it difficult to turn the head.
As the condition progresses, respiratory failure might occur due to muscle weakness, requiring ventilator support.
Differences in Symptoms Among Age Groups or Demographics:
- Children: The majority of AFM cases have been reported in children. They might not be able to express pain or weakness clearly, making it imperative for caregivers to watch for physical signs like limping or refusal to use an arm.
- Adults: Though rare in adults, when affected, they may describe muscle pain, weakness, or numbness. Adults might also experience more severe respiratory issues sooner than children.
- Demographics: Currently, there’s no evidence to suggest that AFM symptoms differ significantly across different racial or ethnic groups.
Long-term Complications and Prognosis:
- Lasting Muscle Weakness: Even with treatment, some individuals may continue to experience muscle weakness or other neurologic complications for months or even years.
- Respiratory Challenges: Due to muscle weakness, some individuals might need long-term support with breathing using machines.
- Physical Therapy Requirement: To regain muscle strength and function, many individuals require ongoing physical therapy.
- Prognosis: The outcome can vary. Some individuals recover fully, while others may have lasting impairments. Early detection and intervention are key to a more favorable prognosis.
It’s essential to consult a healthcare professional if any of these symptoms are observed. Timely intervention can make a significant difference in the outcome.
Causes and Transmission of Acute Flaccid Myelitis (AFM)
Understanding its causes and transmission can help in both awareness and prevention. Let’s delve deeper into the known causative agents and the modes of transmission.
Known Causative Agents
- Enteroviruses: Most cases of AFM are believed to be linked to enteroviruses, especially the EV-D68. Enteroviruses are common viruses, and while they can cause mild respiratory illness, in rare cases, they can also lead to AFM.
- Other Viruses: Some other viruses, like the West Nile Virus or adenoviruses, have also been found in patients with AFM, though the connection is not as established as with enteroviruses.
- Environmental Toxins: Although less common, environmental toxins have been investigated as potential causative agents. However, their direct role in causing AFM is yet to be conclusively determined.
- Genetic Factors: There’s ongoing research to determine if some people have a genetic predisposition making them more susceptible to developing AFM after viral infections.
Mode of Transmission and Preventive Measures
- Respiratory Droplets: AFM-linked enteroviruses are primarily spread through respiratory droplets when an infected person coughs or sneezes. It can also spread by having direct contact with an infected person.Preventive Measures: Practice good respiratory hygiene by covering your mouth and nose with a tissue or your elbow when coughing or sneezing. Also, avoid close contact with people who are sick.
- Contact with Contaminated Surfaces: Touching surfaces or objects that have the virus on them, and then touching the mouth, nose, or eyes can lead to transmission.Preventive Measures: Regular hand washing with soap and water for at least 20 seconds is vital. Avoid touching the face with unwashed hands, and ensure the frequent cleaning of commonly touched surfaces.
- Mosquito Bites: In the case of viruses like West Nile Virus, mosquito bites can be the mode of transmission.Preventive Measures: Use insect repellent, wear long sleeves and pants, and ensure you have mosquito nets or screens to protect against bites.
However, while AFM is rare, awareness of its causative agents and modes of transmission is essential for prevention. Following good hygiene practices and taking preventive measures can significantly reduce the risk of transmission.
Diagnosing Acute Flaccid Myelitis (AFM)
To ensure timely treatment and mitigate potential complications, it’s crucial to recognize and diagnose AFM at its earliest. Here’s a deep dive into how this condition is diagnosed:
Importance of Early Diagnosis
Swift Action: Early diagnosis of AFM can make a significant difference in treatment outcomes. The sooner the condition is identified, the better healthcare providers can address and manage its effects.
Prevention of Complications: Delayed diagnosis may lead to increased severity of symptoms and long-term complications. Early detection minimizes these risks.
Clinical Assessments and History Taking
Symptom Check: Patients often present with sudden muscle weakness in their arms or legs. They might also have facial droop, difficulty swallowing, or slurred speech.
Medical History: A detailed history can provide clues. Have there been any recent illnesses or respiratory issues? Was there a recent exposure to certain environmental factors or potential triggers?
Imaging Studies: MRI Findings and Their Significance
Spotting Abnormalities: MRI (Magnetic Resonance Imaging) is a vital tool in diagnosing AFM. It can detect changes or inflammation in the spinal cord.
Grey Matter Involvement: A hallmark of AFM is the presence of lesions predominantly in the grey matter of the spinal cord. Such findings on an MRI can strongly suggest AFM.
Lab Tests and Spinal Fluid Analysis
Cerebrospinal Fluid (CSF) Examination: Obtaining and analyzing CSF can be instrumental. Elevated levels of white cells or proteins in the CSF can indicate inflammation, a common feature of AFM.
Viral Testing: Checking for the presence of certain viruses can be helpful, as some are known to be potential triggers for AFM.
Differential Diagnosis: Ruling Out Other Conditions
Other Neurological Conditions: It’s essential to differentiate AFM from other neurological disorders that might present with similar symptoms, like Guillain-Barré syndrome or transverse myelitis.
Systematic Approach: A systematic approach to ruling out other diseases can help ensure that the diagnosis is accurate, enabling tailored treatments and interventions for AFM.
However, diagnosing AFM requires a combination of clinical assessments, imaging studies, lab tests, and a keen understanding of the patient’s history. Prioritizing early detection and adopting a thorough and systematic approach can significantly improve patient outcomes.
Acute Flaccid Myelitis (AFM) Treatment Options
Managing and treating AFM effectively requires a comprehensive approach. Below we delve into the primary treatment options available for patients diagnosed with AFM.
Initial Management
Hospitalization and Supportive Care: Upon diagnosis, patients often need hospitalization to ensure they receive the right care. Supportive care focuses on alleviating symptoms and preventing complications, ensuring the patient’s comfort and safety.
Monitoring Respiratory Function and Other Vital Signs: Respiratory function can be compromised in AFM patients. Continuous monitoring of breathing and other vital signs like heart rate and blood pressure is crucial to detect any changes in the patient’s condition promptly.
Medications and Therapies
Use of Antiviral Drugs and Their Efficacy: Antiviral drugs are sometimes prescribed to AFM patients, especially if a viral cause is suspected. Their efficacy can vary, but they aim to reduce the severity and duration of the condition.
Immune Therapies and Plasma Exchange: Some patients benefit from immune therapies, which modulate the body’s immune response. Plasma exchange, also known as plasmapheresis, involves removing and replacing the patient’s plasma to eliminate harmful antibodies.
Physical and Occupational Therapy for Rehabilitation: Muscle weakness is a prominent symptom of AFM. To aid recovery, patients often undergo physical and occupational therapy. These therapies help restore strength, improve mobility, and ensure patients can perform daily activities independently.
Emerging Treatments
Ongoing Research and Trials: As AFM is still not fully understood, continuous research and clinical trials are underway to uncover more effective treatments. These studies are vital for enhancing our understanding and approach to managing the condition.
Potential Breakthroughs and Future Directions: The medical community is optimistic about potential breakthroughs in AFM treatment. With ongoing research, there’s hope for more effective therapies or even a cure in the future.
However, treating Acute Flaccid Myelitis requires a multifaceted approach, combining immediate care with rehabilitation and promising new treatments. As research continues, the future looks brighter for those affected by AFM. If you or a loved one is diagnosed, it’s essential to consult with a medical professional to understand the best treatment options available.
Living with Acute Flaccid Myelitis (AFM)
Those who find themselves diagnosed with AFM face numerous challenges. However, with the right coping mechanisms, support systems, long-term care, and management strategies, living with AFM becomes manageable. Here’s a closer look at how patients cope with AFM and the stories that resonate with many.
Coping Mechanisms and Support Systems
Understanding the Condition: Knowledge is empowering. Understanding AFM, its causes, and its implications can help individuals feel more in control. Many online resources and local organizations offer information on AFM.
Physical Therapy: Engaging in regular physical therapy can help maintain muscle strength and flexibility. It also provides an opportunity for patients to engage in regular activity, promoting mental well-being.
Mental Health Support: Living with AFM can be emotionally taxing. It’s crucial to have a robust mental health support system, including therapy, counseling, or support groups.
Connecting with Others: Joining online forums or local support groups can be beneficial. Sharing experiences, frustrations, and successes with others can provide immense relief.
Long-term Care and Management Strategies
Personalized Treatment Plans: Every AFM patient is different. Work closely with neurologists and other healthcare professionals to design a treatment plan tailored to individual needs.
Regular Check-ups: Keeping up with regular medical appointments can help track the progression of the disease and adjust treatments as needed.
Assistive Devices: Depending on the severity of AFM, devices such as braces or wheelchairs might be needed. Being open to using these aids can significantly enhance quality of life.
Stay Updated: Medical research is ongoing. New treatments and management strategies are being developed. Staying updated can provide hope and newer ways to manage AFM.
Patient Stories and Experiences
Sarah’s Journey: At 29, Sarah was diagnosed with AFM. Initially overwhelmed, she found strength in an online community of AFM patients. Through shared experiences and support, she’s now an advocate, helping others navigate the challenges of AFM.
Michael’s Resilience: A former athlete, Michael’s life took a turn when he contracted AFM. But with the support of his family and intense physical therapy, he’s relearned many of his favorite sports, adapting to his new reality.
Liam and Hope: Liam, a 7-year-old with AFM, showcases the importance of hope and a positive attitude. His heartwarming story of learning to walk again with the help of his dedicated therapist has inspired many.
Living with AFM undoubtedly presents its set of challenges, but with the right support and strategies, one can lead a fulfilling life. The key is to stay informed, connected, and hopeful. The stories of countless patients highlight the resilience of the human spirit, demonstrating that with perseverance, any obstacle can be overcome.
FAQs about Actinic Acute Flaccid Myelitis (AFM)
What is Actinic Acute Flaccid Myelitis (AFM)?
Actinic Acute Flaccid Myelitis (AFM) is a rare but serious neurological condition that affects the spinal cord, leading to muscle weakness and even paralysis. Its exact causes are still under investigation, but it’s believed that certain viral infections might play a role.
How is AFM diagnosed?
AFM is diagnosed based on a combination of factors. These include clinical examination to assess muscle strength and reflexes, magnetic resonance imaging (MRI) to view the spinal cord, and laboratory testing of cerebrospinal fluid. Early and accurate diagnosis is crucial for the best possible outcomes.
What are the symptoms of AFM?
Symptoms of AFM can range from mild to severe. Common signs include sudden arm or leg weakness, loss of muscle tone, and decreased or absent reflexes. In severe cases, patients may experience difficulty moving their eyes, drooping facial muscles, or difficulty swallowing.
How is AFM treated?
There is currently no specific treatment for AFM. However, doctors may recommend certain interventions to manage symptoms and improve the patient’s quality of life. These can include physical therapy to improve muscle strength, pain management, and respiratory support in severe cases where breathing becomes difficult.
Is there a vaccine or prevention method for AFM?
As of now, there isn’t a specific vaccine for AFM. However, it’s believed that certain viral infections may trigger AFM. Getting vaccinated against these viruses, like poliovirus and enterovirus, can potentially reduce the risk. Practicing good hygiene, like frequent hand washing, can also help in preventing the spread of viruses that might lead to AFM.
How common is AFM?
AFM is a rare condition, with only a few hundred cases reported in the U.S. each year. However, it’s essential to be aware of its symptoms and seek medical attention immediately if any are noticed.
Is AFM contagious?
AFM itself is not contagious. However, if it is triggered by a viral infection, that virus can be contagious. It’s always essential to practice good hygiene and avoid close contact with sick individuals to reduce the risk of infection.
Remember, while this information provides a general overview, it’s always best to consult with a healthcare professional for personalized advice and information about Actinic Acute Flaccid Myelitis (AFM).
Conclusion
In the journey of understanding and combating diseases, the significance of early diagnosis and treatment cannot be emphasized enough. Recognizing symptoms at the outset not only increases the likelihood of a successful recovery but also reduces the strain on healthcare systems and alleviates potential long-term health implications.
As readers and responsible individuals, we have a pivotal role to play. If you or someone you know exhibits concerning symptoms, don’t hesitate—seek medical attention promptly. But our responsibility doesn’t end at personal vigilance. It extends to raising awareness among our communities, ensuring that everyone understands the criticality of early intervention.
Furthermore, supporting research is fundamental. Continuous advancements in medical science hinge on our collective backing—both in terms of awareness and funding. By advocating for and investing in research, we pave the way for groundbreaking discoveries that can change the course of health outcomes.
In conclusion, let’s champion the cause of early diagnosis and treatment. Your proactive steps today can be the difference-maker for many tomorrow. Let’s unite in this endeavor, seeking medical attention when necessary, raising awareness, and wholeheartedly supporting research. Together, we can make a substantial difference.