Achilles Tendinitis Symptoms: The Achilles tendon, a pivotal part of our anatomy, is the strongest and largest tendon in the human body. However, it’s also susceptible to a condition known as Achilles tendinitis.
In this comprehensive guide, we delve deep into the symptoms, causes, and intricacies of Achilles tendinitis, shedding light on this common but often misunderstood ailment.
What is Achilles Tendinitis?
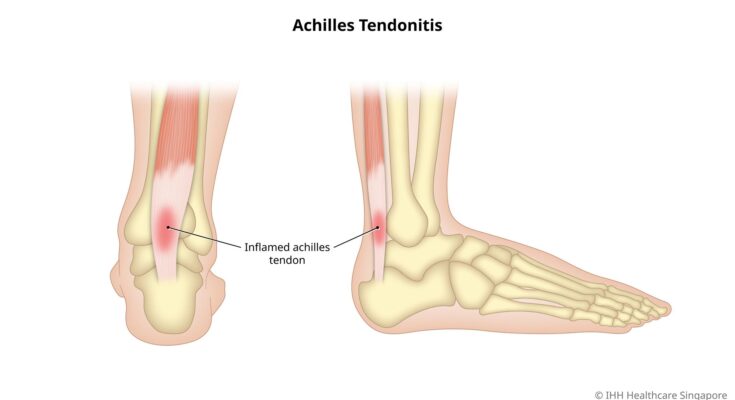
Achilles tendinitis is an inflammation of the Achilles tendon, the strong and thick tendon that connects the calf muscles to the heel bone. This condition often results from overuse or excessive strain, especially in athletes and individuals who engage in activities that put repetitive stress on the tendon. Symptoms typically include pain, swelling, and stiffness near the heel, which may worsen with activity.
The Difference Between Tendinitis and Tendinosis:
While both tendinitis and tendinosis involve the tendons, their primary distinction lies in the nature of the injury and the duration of symptoms.
- Tendinitis: Refers to acute inflammation of the tendon resulting from micro-tears due to sudden trauma or overuse. The inflammation is the body’s natural response to injury. With proper rest and treatment, tendinitis often heals within a few weeks.
- Tendinosis: On the other hand, is a chronic condition characterized by the degeneration of the tendon’s collagen due to long-term wear and tear, without significant inflammation. This condition is typically more prolonged than tendinitis and may require a more extended period of treatment and recovery.
By understanding the differences between these conditions, individuals can seek the most appropriate treatment and care for their specific needs.
Symptoms of Achilles Tendinitis
1. Persistent Pain: One of the primary indicators of Achilles tendinitis is a dull or sharp pain at the back of the lower leg or just above the heel. This pain may intensify after prolonged periods of rest or at the start of exercise.
2. Stiffness: Many individuals report stiffness in the heel area, especially during the morning or after prolonged periods of inactivity.
3. Swelling: The area around the Achilles tendon may become swollen, and this can sometimes be accompanied by warmth or redness.
4. Reduced Range of Motion: As the condition progresses, the individual might experience a decreased range of motion in the ankle, especially when flexing the foot.
5. Tendon Thickening: Over time, the Achilles tendon can thicken, which can be felt as a small lump on the tendon.
Underlying Causes of Achilles Tendinitis
Understanding the root causes of Achilles tendinitis is essential for both prevention and treatment.
1. Excessive Strain: Frequently subjecting the Achilles tendon to high levels of stress, such as intensive training or not allowing enough recovery time between workouts, can result in tendinitis.
2. Inadequate Footwear: Wearing shoes that do not offer adequate support or cushioning can put extra stress on the Achilles tendon.
3. Physical Misalignment: Conditions like flat feet or overpronation can exert undue strain on the Achilles tendon, elevating the risk of tendinitis.
4. Age Factor: As we age, our tendons lose flexibility and become more prone to injury, making older individuals more susceptible to Achilles tendinitis.
5. Medical Conditions: Some medical conditions, including high blood pressure and certain types of antibiotics, can increase the risk of Achilles tendon issues.
6. Sudden Increase in Activity: Jumping into a new or intensified exercise regimen without a gradual buildup can overtax the Achilles tendon.
Prevention and Proactive Measures
While understanding the symptoms and causes is crucial, taking preventive measures can keep this condition at bay.
1. Gradual Progression: Always ensure that any increase in exercise intensity or duration is gradual to give the tendon time to adapt.
2. Strength Training: Strengthening calf muscles can help in reducing the strain on the Achilles tendon.
3. Flexibility Exercises: Regular stretching of the calf muscles and the Achilles tendon enhances flexibility and reduces the risk of injury.
4. Appropriate Footwear: Always opt for shoes that offer sufficient arch support and cushioning.
5. Regular Rest: It’s essential to listen to your body and allow ample recovery time between rigorous exercises.
Risk Factors and Populations Most Affected
Understanding these factors can help in prevention and early diagnosis, ensuring timely treatment and reducing complications.
1. Age, Gender, and Physical Activity Level:
Age: As we age, our tendons naturally lose their flexibility and strength. This makes older individuals more susceptible to injuries like Achilles tendinitis. Typically, individuals in their 30s and 40s are at a higher risk.
2. Gender: Research indicates that men are more likely to develop Achilles tendinitis than women. The reasons for this gender disparity are multifaceted and may include differences in physical activity patterns, hormonal factors, and biomechanical differences between men and women.
3. Physical Activity Level: Individuals who are suddenly more active or increase the intensity of their workouts without proper conditioning are at a greater risk. For instance, weekend warriors or those who undergo intense training spurts without adequate preparation may be more prone to Achilles issues.
2. Certain Sports and Their Association with Achilles Tendinitis:
1. Running: Due to its repetitive impact nature, long-distance running can put immense strain on the Achilles tendon. Runners, especially those who don’t engage in proper stretching or wear appropriate footwear, are at an elevated risk.
2. Basketball and Tennis: Sports that involve frequent starts and stops, jumping, and rapid directional changes can exert a lot of pressure on the Achilles tendon. Athletes playing basketball or tennis need to be particularly mindful of the potential risks.
3. Soccer and Football: Given the nature of these sports, with their rapid changes in direction and speed, players are prone to Achilles injuries. Proper conditioning and training can help mitigate these risks.
4. Dance: Dancers, especially ballet performers who frequently go on their toes, put immense strain on the Achilles tendon. It’s crucial for them to engage in regular conditioning exercises to maintain tendon health.
However, while Achilles tendinitis can affect anyone, understanding the populations and activities most at risk can guide prevention and treatment strategies. Regular stretching, appropriate footwear, and gradual increases in physical activity can significantly reduce the chances of developing this condition.
Frequently Asked Questions on Achilles tendinitis
What is Achilles tendinitis?
Achilles tendinitis is an overuse injury of the Achilles tendon, the band of tissue connecting calf muscles at the back of the lower leg to your heel bone.
What causes Achilles tendinitis?
This condition often arises due to repetitive stress on the Achilles tendon. Common causes include increased activity levels, wearing inappropriate footwear, or failing to stretch before physical activities.
How can I recognize Achilles tendinitis?
Symptoms often include pain and swelling around the heel, stiffness in the tendon, especially in the morning, and increased pain after physical activity.
How is Achilles tendinitis treated?
Treatment often involves rest, ice, over-the-counter pain relievers, and physical therapy. In severe cases, surgery might be necessary.
Can I prevent Achilles tendinitis?
Yes. Regularly stretch your Achilles tendon, gradually increase activity levels, and wear appropriate footwear to reduce your risk.
How long does recovery typically take?
Most people recover within a few months with proper treatment. However, severe cases may take longer.
Remember, if you’re experiencing symptoms of Achilles tendinitis, it’s important to consult with a healthcare professional.
Conclusion
In wrapping up, it’s crucial to underscore the significance of promptly identifying Achilles tendinitis symptoms. Early recognition not only aids in faster recovery but also prevents potential complications and long-term damage.
If you notice persistent discomfort or any of the typical symptoms, don’t hesitate to consult a medical professional. Your health is paramount, and timely medical advice can be the difference between quick relief and prolonged pain.
Always prioritize your well-being by staying informed and proactive.