Achalasia Treatment: Achalasia is a rare disorder affecting the esophagus, causing difficulty in swallowing and often leading to regurgitation.
While relatively uncommon, understanding its symptoms, diagnosis, and treatment options is crucial for both medical practitioners and affected individuals.
In this article, we provide a comprehensive overview of achalasia, its diagnosis, and the treatment options available today.
Understanding Achalasia
Achalasia is a rare but noteworthy esophageal disorder that can significantly impact a person’s ability to eat and swallow. Let’s dive deeper into understanding this condition, its causes, how it differentiates from other esophageal disorders, and its key symptoms.
What is Achalasia?
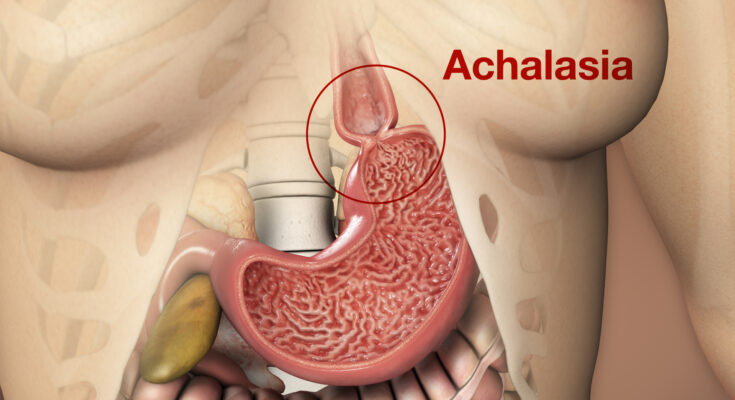
Achalasia is a neuro-muscular disorder of the esophagus. In essence, the lower esophageal sphincter, which is the muscular valve between the esophagus and the stomach, fails to relax properly. This makes it difficult for food and liquids to pass into the stomach, often causing them to back up into the esophagus.
Etiology and Pathophysiology
The exact cause of achalasia remains unknown. However, it’s believed to result from a combination of hereditary and environmental factors. The nerve cells in the esophagus deteriorate, leading to muscle dysfunction. Over time, this leads to the absence of normal esophageal contractions and the failure of the lower esophageal sphincter to relax, causing food to become trapped.
Differences from Other Esophageal Disorders
Achalasia has distinct features that differentiate it from other esophageal disorders. For instance:
1. Dysfunction of Muscular Contractions: Unlike other disorders where there might be irregular or spastic contractions, achalasia is characterized by the absence of normal contractions.
2. Unique Radiographic Appearance: Barium swallow studies of patients with achalasia will often show a characteristic “bird’s beak” appearance.
3. Absence of Structural Obstruction: While other disorders might have structural blockages, achalasia’s obstruction is functional due to muscle and nerve dysfunction.
Symptoms and Clinical Manifestations
Achalasia presents with a variety of symptoms, including:
1. Dysphagia: Difficulty swallowing, which is the most common symptom.
2. Regurgitation: The backflow of undigested food.
3. Chest Pain: Often mistaken for heart-related pain.
4. Heartburn: A burning sensation in the chest.
5. Weight Loss: Due to difficulties in swallowing and food intake.
However, achalasia is a significant esophageal disorder that necessitates comprehensive understanding and medical intervention. Its unique characteristics set it apart from other esophageal conditions, and timely diagnosis is crucial for effective management.
Diagnosis of Achalasia
Early and accurate diagnosis is essential for effective treatment. Here’s a breakdown of how the condition is usually diagnosed:
Initial Clinical Assessment
Before delving deep into specific tests, physicians begin with an initial assessment to understand the symptoms and rule out other conditions.
1. Patient History: One of the first steps is taking a comprehensive patient history. Questions might revolve around the onset of symptoms, the type of food that triggers discomfort, any weight loss, and history of similar complaints in the family. The duration, frequency, and progression of symptoms like difficulty in swallowing or chest pain can provide significant clues.
2. Physical Examination: While achalasia primarily concerns the esophagus, a general physical examination is done to rule out other causes and check for any noticeable symptoms like undernutrition or dehydration resulting from swallowing difficulties.
Diagnostic Tests and Procedures
Once the preliminary assessment is done, specific diagnostic tests are employed to confirm the diagnosis:
1. Esophageal Manometry: This test measures the rhythmic muscle contractions inside the esophagus. In achalasia, these contractions are typically abnormal or absent. The test can pinpoint the specific type of achalasia and guide treatment decisions.
2. Barium Swallow Study: Patients are asked to swallow a barium solution, which is then tracked using X-rays as it travels down the esophagus. In achalasia patients, the barium often shows a distinctive ‘bird’s beak’ appearance, indicative of the narrowed lower esophagus.
3. Endoscopy: Using a flexible tube with a camera (endoscope), doctors inspect the esophagus directly. This helps in ruling out other potential causes like tumors and offers a clear view of the esophageal structure.
Challenges and Common Misconceptions in Diagnosing Achalasia
Diagnosing achalasia is not always straightforward. A significant challenge is its symptom overlap with conditions like gastroesophageal reflux disease (GERD). Thus, many patients are mistakenly treated for acid reflux before a correct diagnosis is made.
Common misconceptions include:
1. It’s just chronic indigestion or heartburn: Due to similar symptoms, many assume achalasia is a simple digestive issue that can be treated with over-the-counter meds.
2. Dietary habits are the cause: While diet can exacerbate symptoms, achalasia is not caused by dietary choices.
3. It’s an age-related problem: Though more common in adults, achalasia can affect people of any age, including children.
However, an accurate diagnosis of achalasia requires a combination of clinical assessments and specific tests. Being aware of the condition and its nuances can ensure timely and appropriate care.
Comprehensive Achalasia Treatment Options
Patients with achalasia face difficulty in passing food from the esophagus to the stomach. Fortunately, there are several treatment options available. Let’s delve deeper into these options to help individuals make informed decisions about their health.
Non-Surgical Treatments
1. Medications: Two common types of medications prescribed are:
- Nitrates: These help in relaxing the lower esophageal sphincter, making it easier to swallow.
- Calcium channel blockers: Similarly, they aid in muscle relaxation and can reduce the difficulty in swallowing. Regular intake as prescribed is essential for maintaining their effect.
2. Botox injections: This treatment involves injecting botulinum toxin into the lower esophageal sphincter. The Botox temporarily paralyzes the muscles, aiding in easier food passage. However, the effects of these injections are temporary, typically lasting for six months, after which repeated treatments might be necessary.
Surgical Treatments
1. Heller Myotomy: This is a surgical procedure where small incisions are made to access the lower esophagus. The muscles are then partially cut to aid in easier food passage. The outcomes are generally positive with a significant reduction in swallowing difficulties.
2. Peroral endoscopic myotomy (POEM): A minimally invasive procedure, POEM involves creating a tunnel inside the esophagus wall to cut the muscle. It has the advantage of being less invasive than other surgeries. However, potential complications might include reflux or perforation, so it’s essential to discuss these with your healthcare provider.
Balloon Dilation
This treatment involves placing a balloon in the esophagus and inflating it, aiming to widen the area and facilitate easier swallowing. While it’s a less invasive option than surgery, risks include potential tears in the esophagus. The benefits, however, include improved food passage and reduced symptoms.
Post-Treatment Care and Considerations
1. Diet modifications: After undergoing treatment, it’s often recommended to modify one’s diet. This might include eating softer foods, smaller meals, and ensuring a more gradual introduction of regular foods.
2. Follow-up visits and ongoing care: Regular check-ups with healthcare professionals are crucial. They help in monitoring the progress, addressing any concerns, and ensuring the effectiveness of the treatment.
Remember, it’s vital to discuss the potential risks and benefits of each treatment option with a healthcare provider to make the best decision tailored to individual needs.
Potential Complications of Untreated Achalasia
Untreated achalasia can lead to a variety of health issues. Being aware of these complications can help individuals understand the importance of timely intervention.
Esophageal Damage and Its Consequences:
Over time, untreated achalasia can cause the esophagus to become stretched and dilated. This can lead to a condition called megaesophagus. As the esophagus enlarges, it becomes increasingly difficult for food and liquids to pass into the stomach, leading to food stasis or buildup. This can subsequently cause the esophagus to become inflamed, or in more severe cases, the tissue may break down leading to esophageal ulcers or even increase the risk of esophageal cancer.
Risk of Aspiration and Associated Respiratory Issues:
When food and liquids cannot pass easily into the stomach, there’s a heightened risk of them being aspirated, or entering the windpipe and lungs. Aspiration can lead to pneumonia, a serious lung infection, or even cause choking. Over time, recurrent aspirations can damage the lungs and lead to chronic respiratory problems.
Malnutrition and Weight Loss:
Achalasia can make it challenging for individuals to eat and drink properly. If the condition is left untreated, it can result in significant weight loss. As the body struggles to receive the necessary nutrients, there’s a risk of malnutrition. This can further weaken the immune system, making individuals more susceptible to illnesses and reducing their overall quality of life.
However, it’s crucial to seek medical attention if you suspect you have achalasia. Timely diagnosis and treatment can help prevent these potential complications and improve overall well-being.
The Importance of Early Detection and Treatment of Achalasia
When not addressed promptly, it can lead to severe health complications and decline in quality of life. Here’s why early detection and treatment are crucial.
Prognosis with Timely Treatment versus Delay
1. Faster Recovery: Recognizing and treating achalasia in its initial stages can lead to quicker recovery times and less invasive treatment options.
2. Prevention of Complications: Delay in treatment increases the risk of complications, such as esophageal dilation or the possibility of the esophagus becoming unresponsive to treatment. Early intervention can help mitigate these risks.
3. Enhanced Treatment Outcomes: Patients who seek treatment early often experience better overall outcomes compared to those who wait. The progression of the disease can be halted or even reversed if addressed promptly.
Quality of Life Considerations for Patients
1. Improved Daily Functioning: Achalasia can make simple tasks like eating or drinking a challenging ordeal. Timely treatment restores the ability to enjoy meals and prevents malnutrition.
2. Psychological Well-being: Struggling with swallowing and the constant fear of food getting stuck can cause stress and anxiety. Early treatment can alleviate these psychological strains, allowing patients to lead a more confident and worry-free life.
3. Social Benefits: Eating is a communal activity. By addressing achalasia early on, patients can continue to participate in social gatherings, family dinners, and other events without feeling alienated or self-conscious.
However, the early detection and treatment of achalasia are not just about medical intervention. They play a pivotal role in enhancing the quality of life, mental well-being, and social interactions of patients. Prioritizing early intervention can lead to a healthier, happier, and more fulfilling life for those affected.
Frequently Asked Questions on Achalasia
What is Achalasia?
Achalasia is a rare disorder of the esophagus, where the muscles fail to function normally, leading to difficulties in swallowing and sometimes chest pain.
What causes Achalasia?
The exact cause remains unknown. However, it’s believed to be due to the loss of nerve cells in the esophagus, which can be due to factors like genetics, autoimmune responses, or infections.
What are the symptoms of Achalasia?
Common symptoms include difficulty swallowing, regurgitation of undigested food, chest pain, weight loss, and heartburn.
How is Achalasia diagnosed?
Doctors usually diagnose Achalasia through a combination of symptoms, barium swallow studies, endoscopy, and esophageal manometry.
How is Achalasia treated?
Treatment options can vary but may include medications, Botox injections, balloon dilation, or surgery like Heller myotomy.
Is Achalasia life-threatening?
While Achalasia is not directly life-threatening, untreated cases can lead to severe weight loss, malnutrition, and the risk of aspiration pneumonia.
Can you live a normal life with Achalasia?
With appropriate treatment and management, many individuals with Achalasia can lead a near-normal life, although dietary and lifestyle modifications might be needed.
Is Achalasia hereditary?
While the exact cause is still under research, there’s no concrete evidence suggesting that Achalasia is hereditary. However, there have been rare familial cases reported.
How common is Achalasia?
Achalasia is considered rare, affecting about 1 in every 100,000 people annually.
Can Achalasia be prevented?
Since the exact cause remains uncertain, there’s no known way to prevent Achalasia. However, early diagnosis and treatment can manage its symptoms effectively.
Conclusion
In wrapping up, it’s imperative to stress the profound significance of comprehending, diagnosing, and effectively treating Achalasia. This condition, while often overlooked, can profoundly impact one’s quality of life. Equipped with the right knowledge, early detection becomes possible, paving the way for timely and effective treatment.
If you or someone you know is experiencing symptoms associated with Achalasia, don’t delay. Be proactive about your health. Seek medical attention immediately, and prioritize your well-being. Remember, early intervention can make all the difference. Your health is worth it.