Benign Prostatic Hyperplasia Symptoms: Benign Prostatic Hyperplasia (BPH), commonly known as prostate gland enlargement, is a prevalent condition affecting middle-aged and elderly men.
This comprehensive guide aims to delve into the symptoms and causes of BPH, providing insightful knowledge for those seeking to understand this condition.
What is Benign Prostatic Hyperplasia?
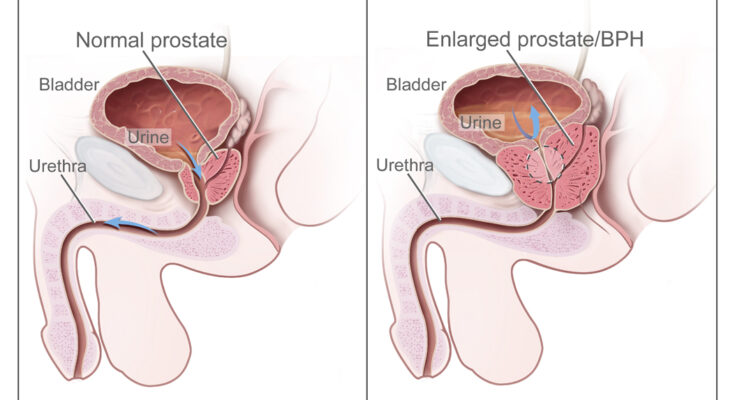
Benign Prostatic Hyperplasia (BPH), commonly referred to as an enlarged prostate, is a non-cancerous increase in the size of the prostate gland. This enlargement can lead to urinary problems such as difficulty in starting urination, a weak stream, and frequent urination, especially at night. It’s important to understand that BPH is a normal part of aging for men and not necessarily a cause for alarm.
Prevalence and Demographic Most Affected
BPH predominantly affects older men. The prevalence of BPH increases significantly with age. It is estimated that approximately 50% of men in their 50s have some degree of prostate enlargement, and this figure jumps to about 90% for men in their 80s. Therefore, age is a major factor in the likelihood of developing BPH. While this condition is rare in men under 40, its occurrence becomes more common as men age.
Difference Between BPH and Prostate Cancer
While both BPH and prostate cancer involve the prostate gland, they are fundamentally different conditions. BPH is a benign condition meaning it is not cancerous and does not spread to other parts of the body. Prostate cancer, on the other hand, is a malignant growth that can potentially be life-threatening and spread to other parts of the body.
One key difference is the nature of cell growth. In BPH, the enlargement is due to an increase in the number of cells (hyperplasia), whereas prostate cancer involves uncontrolled, abnormal cell growth. Symptoms can be similar in early stages, but prostate cancer may have other symptoms like erectile dysfunction, blood in urine or semen, and pain in the hips, back, or chest as it advances.
It’s crucial for men, especially those over the age of 50, to have regular check-ups that include prostate examinations to distinguish between BPH and prostate cancer. Early detection is key in the management of both conditions.
Understanding the differences between these two prostate conditions is vital for proper diagnosis and treatment. Remember, having BPH does not mean you will develop prostate cancer, but routine medical check-ups are essential for maintaining good health.
Symptoms of Benign Prostatic Hyperplasia (BPH)
Understanding its symptoms is crucial for early detection and effective management. This section delves into the various symptoms associated with BPH, their impact on daily life, and when it’s advisable to seek medical advice.
Detailed List of Common Symptoms
1. Frequent Urination: One of the earliest signs of BPH is the need to urinate more often, especially at night (nocturia).
2. Difficulty Starting Urination: Men may experience hesitancy or struggle to initiate urination.
3. Weak Urine Stream: A noticeable decrease in the strength and caliber of the urine stream.
4. Feeling of Incomplete Bladder Emptying: There’s often a sensation that the bladder isn’t completely empty after urination.
5. Dribbling at the End of Urination: An involuntary release of a few drops of urine after finishing.
6. Urgency to Urinate: A sudden, strong urge to urinate is common.
7. Urinary Retention: In severe cases, there can be a complete inability to urinate.
How BPH Symptoms Impact Daily Life
The symptoms of BPH can significantly affect a man’s quality of life. Frequent trips to the bathroom, especially at night, can disrupt sleep, leading to fatigue and decreased energy levels. The urgency and difficulty in urination can also cause anxiety and stress, particularly in social or work situations where bathroom access is limited. Moreover, sexual dysfunction is a potential consequence, impacting intimate relationships.
When to Seek Medical Advice
It’s crucial to consult a healthcare professional if you experience any of the above symptoms. Early medical intervention is particularly important in cases of:
- Persistent discomfort or pain during urination.
- Blood in urine, signaling a possible infection or other complications.
- Inability to urinate, which can be a medical emergency.
- Noticeable decline in the quality of life due to urinary symptoms.
Proactive management of BPH can mitigate its impact on your health and daily life. Regular check-ups and early detection are key in preventing complications associated with this condition. Remember, BPH is a common issue among aging men, and effective treatments are available to alleviate its symptoms.
Causes and Risk Factors of Benign Prostatic Hyperplasia (BPH)
Understanding the causes and risk factors associated with BPH is crucial for prevention and effective management. This article provides a comprehensive overview of the biological causes, lifestyle and environmental risk factors, and the role of age and genetics in BPH development.
Biological Causes of BPH
Hormonal Changes: As men age, hormonal fluctuations occur, notably in testosterone and estrogen levels. These changes can contribute to prostate growth, leading to BPH.
Cellular Changes: At the cellular level, an imbalance between cell proliferation (growth) and cell death can result in prostate enlargement. This imbalance is often influenced by hormonal shifts.
Prostatic Tissue Inflammation: Chronic inflammation in the prostate tissue can stimulate prostate enlargement, thus contributing to BPH.
Prostate Growth Factors: Certain growth factors, proteins that stimulate cell growth, are more active in men with BPH. These factors contribute to the abnormal growth of prostate cells.
Lifestyle and Environmental Risk Factors
Diet: A diet high in red meat and fatty foods and low in fruits and vegetables may increase BPH risk.
Obesity: Excess body weight has been linked to an increased risk of BPH, potentially due to hormonal changes associated with obesity.
Lack of Physical Activity: A sedentary lifestyle may increase the risk of BPH. Regular exercise can help reduce this risk.
Smoking and Alcohol Consumption: Smoking and excessive alcohol use have been associated with an increased risk of developing BPH.
Exposure to Certain Chemicals: Occupational exposure to certain chemicals, like cadmium, can increase BPH risk.
The Role of Age and Genetics in BPH
Age: BPH is more common in older men. The risk increases significantly after the age of 50, with most cases occurring in men over 60.
Genetic Factors: Genetics play a significant role in BPH. Men with a family history of BPH are more likely to develop the condition.
Ethnicity: Certain ethnic groups, such as African-American men, are at a higher risk of developing BPH.
However, BPH is a multifactorial condition influenced by biological factors, lifestyle choices, environmental exposures, age, and genetics. Awareness and management of these risk factors can help in the prevention and treatment of BPH. Regular check-ups and discussions with healthcare professionals are essential for early detection and effective management of BPH.
Understanding the Pathophysiology of Benign Prostatic Hyperplasia (BPH)
Let’s delves into the intricate pathophysiology of BPH, aiming to provide a clear understanding of its development, the underlying science of prostate enlargement, and its impact on the urinary tract and bladder.
1. How BPH Develops in the Prostate
Hormonal Changes: Central to the development of BPH are hormonal changes, particularly in testosterone and dihydrotestosterone (DHT) levels. These hormonal shifts trigger prostate growth.
Cellular Proliferation: An increase in the number of cells (proliferation) within the prostate contributes to its enlargement. This growth is not cancerous but can lead to urinary symptoms.
Age-Related Factors: The risk of developing BPH increases with age. By understanding the specific age-related changes in the prostate, we can better grasp the onset of BPH.
2. The Science Behind the Enlargement of the Prostate Gland
Prostatic Growth: The prostate gland surrounds the urethra. As it enlarges, it can constrict or block the urethra, leading to urinary symptoms.
Molecular Mechanisms: Research into the molecular pathways, such as growth factors and inflammatory responses, provides insight into why and how the prostate enlarges in BPH.
Genetic Factors: Genetic predisposition plays a role in BPH. Understanding these genetic components can help predict susceptibility and guide treatment options.
3. Impact on Urinary Tract and Bladder
Urinary Symptoms: BPH can lead to lower urinary tract symptoms (LUTS), including difficulty in urinating, increased frequency, nocturia (night-time urination), and a weak urinary stream.
Bladder Function: Over time, BPH can affect bladder function, leading to incomplete emptying, increased risk of urinary tract infections, and in severe cases, bladder stones or kidney damage.
Quality of Life: The impact of BPH on daily activities can be significant, affecting the quality of life. Early diagnosis and management are crucial in mitigating these effects.
However, understanding the pathophysiology of BPH is vital for effective management and treatment of this common condition. By exploring the development, science behind prostate enlargement, and its impact, healthcare professionals and patients can work together towards improving outcomes and quality of life for those affected by BPH.
Diagnosis of Benign Prostatic Hyperplasia
Benign Prostatic Hyperplasia (BPH) is a common condition affecting older men, involving the enlargement of the prostate gland. Understanding the diagnosis process is crucial for early intervention and effective management.
Common Diagnostic Tests and Procedures
Digital Rectal Examination (DRE): A fundamental initial test where a doctor feels the prostate through the rectum to check for enlargement, lumps, or abnormalities.
Prostate-Specific Antigen (PSA) Test: This blood test measures the level of PSA, a substance produced by the prostate. Elevated levels can indicate BPH or other prostate issues.
Urine Flow Test: Helps in assessing the strength and steadiness of urine flow. A reduced flow can suggest BPH.
Postvoid Residual Volume Test: Determines the amount of urine left in the bladder after urination, using ultrasound. High residual urine volume can be a sign of BPH.
Prostate Ultrasound: Provides images of the prostate, aiding in assessing its size and condition.
Role of Medical History and Physical Examination
A thorough medical history and physical examination are pivotal in diagnosing BPH. Doctors inquire about urinary symptoms, health history, and any medications. This holistic approach helps differentiate BPH from other conditions with similar symptoms, like prostate cancer or urinary tract infections.
The Importance of Early Diagnosis
Early diagnosis of BPH is vital for several reasons:
- Preventing Complications: Untreated BPH can lead to urinary tract infections, bladder stones, and kidney damage.
- Quality of Life: Early treatment can alleviate symptoms, improving sleep quality and daily comfort.
- Treatment Planning: Early detection allows more treatment options with potentially fewer side effects.
Regular check-ups and awareness of BPH symptoms are crucial, especially for men over 50. Early diagnosis and treatment can significantly improve quality of life and prevent serious complications.
Complications Associated with Untreated Benign Prostatic Hyperplasia (BPH)
Benign Prostatic Hyperplasia (BPH), commonly known as an enlarged prostate, is a condition that affects many men as they age. While it’s non-cancerous, neglecting treatment can lead to significant health complications. Awareness of these risks is crucial for early intervention and maintaining a healthy lifestyle.
1. Potential Health Risks of Untreated BPH
Untreated BPH can lead to a range of health issues, each progressively impacting a man’s well-being. One of the primary concerns is urinary retention, where the bladder doesn’t completely empty. This can cause urinary tract infections (UTIs), bladder stones, and in severe cases, bladder damage. Recognizing these risks is the first step towards proactive healthcare.
2. Long-Term Effects on Urinary Health and Quality of Life
Chronic BPH can severely disrupt daily life. Men may experience frequent urination, particularly at night (nocturia), leading to sleep disturbances and fatigue. The constant need to find a restroom can limit social activities and travel, impacting overall quality of life. Addressing BPH early can help preserve daily routines and personal well-being.
3. Connection with Kidney Problems
Perhaps the most serious complication of untreated BPH is its potential impact on kidney function. When the bladder doesn’t empty properly, it can lead to increased pressure and eventual kidney damage. In extreme cases, this can progress to kidney failure, a condition requiring dialysis or transplantation. Early treatment of BPH can be a key factor in preventing these severe outcomes.
However, while BPH is a common and often treatable condition, ignoring its symptoms can lead to serious health complications. Regular medical check-ups and addressing symptoms early can help prevent long-term damage to urinary and kidney health, ensuring a better quality of life.
Treatment Options for Benign Prostatic Hyperplasia (BPH)
Understanding the variety of treatment options available is crucial for those seeking relief from BPH symptoms. In this comprehensive guide, we will delve into the current treatment methodologies, compare medication versus surgical options, and explore emerging treatments and therapies.
Current Treatment Methodologies
Medications: The first line of treatment often involves medications such as alpha-blockers (e.g., Tamsulosin) and 5-alpha reductase inhibitors (e.g., Finasteride). These drugs work by relaxing bladder neck muscles and shrinking the prostate, respectively, easing urinary symptoms.
Minimally Invasive Therapies: Procedures like Transurethral Microwave Thermotherapy (TUMT) and Transurethral Needle Ablation (TUNA) offer less invasive alternatives to surgery. They use heat to reduce prostate size and alleviate symptoms.
Surgical Options: For severe cases, surgical interventions may be necessary. These include Transurethral Resection of the Prostate (TURP), Laser Therapy, and Prostatectomy, each with specific indications and recovery profiles.
Comparison of Medication vs. Surgical Options
Medications: Generally preferred for mild to moderate symptoms. They are less invasive, have fewer risks, and require no recovery time. However, they may need to be taken long-term and can have side effects.
Surgical Options: Recommended for more severe symptoms or when medications are ineffective. Surgery offers a more permanent solution, but with increased risks, longer recovery periods, and potential side effects like incontinence or sexual dysfunction.
Emerging Treatments and Therapies
Aquablation Therapy: A novel treatment using waterjet technology to remove prostate tissue while sparing surrounding structures, potentially offering fewer side effects.
Prostatic Artery Embolization (PAE): A minimally invasive procedure where the blood supply to the prostate is reduced, causing it to shrink. Early studies show promising results with minimal side effects.
High-Intensity Focused Ultrasound (HIFU): This emerging therapy uses ultrasound waves to target and destroy prostate tissue, offering a less invasive option with a quicker recovery.
However, treatment for BPH ranges from medications and minimally invasive procedures to traditional surgery. The choice of treatment should be based on the severity of symptoms, overall health, and personal preferences. Emerging therapies like Aquablation, PAE, and HIFU are expanding the horizon of BPH treatment, offering new hope for patients seeking effective and less invasive options.
Lifestyle Management and Preventive Measures for BPH
Tips for Managing Symptoms of BPH
Benign Prostatic Hyperplasia (BPH), commonly known as an enlarged prostate, can significantly impact the quality of life. Managing its symptoms effectively is crucial. Here are some tips:
Stay Active: Regular exercise helps maintain a healthy weight and reduces the symptoms of BPH.
Bladder Training: Practice holding your urine for longer periods to train your bladder.
Limit Fluid Intake at Night: Reducing fluid consumption before bedtime can lessen nighttime urination.
Avoid Triggers: Caffeine and alcohol can exacerbate symptoms, so it’s advisable to limit their intake.
Dietary and Lifestyle Changes to Alleviate BPH Symptoms
Diet plays a pivotal role in managing BPH symptoms. Here’s what you can do:
Increase Fiber Intake: A diet rich in fruits, vegetables, and whole grains can improve prostate health.
Opt for Plant-based Proteins: Soybeans and lentils can be beneficial.
Include Healthy Fats: Omega-3 fatty acids found in fish and flaxseed are good for prostate health.
Stay Hydrated: Regular water consumption is important, but balance it to avoid frequent urination.
Importance of Regular Check-ups and Monitoring
Regular medical check-ups are vital for monitoring BPH:
Routine Exams: Regular prostate exams help in early detection and management.
Discuss Changes: Inform your doctor about any new symptoms or changes in existing ones.
Medication Review: Regularly review your medications with your doctor to manage side effects and interactions.
Stay Informed: Keeping abreast of the latest research and treatment options can empower you in managing BPH.
Incorporating these lifestyle and dietary changes, along with regular medical supervision, can significantly alleviate BPH symptoms and improve your quality of life. Remember, an informed and proactive approach is key to managing BPH effectively.
Conclusion
If you or someone you know is experiencing symptoms suggestive of BPH, it’s vital to consult a healthcare professional. Early medical advice can lead to better management of the condition, potentially preventing complications such as urinary tract infections, bladder stones, or kidney damage. Remember, BPH is a common condition, and seeking help is a sign of taking proactive steps towards your health and well-being.
Managing BPH is a multifaceted approach involving lifestyle changes, medication, and in some cases, surgery. Staying informed about the condition, understanding the symptoms, and keeping open communication with your healthcare provider are key to effective management.
In conclusion, Benign Prostatic Hyperplasia is a condition that can significantly impact quality of life but is manageable with the right approach and medical guidance. Awareness, early detection, and proactive management are the cornerstones of living well with BPH.