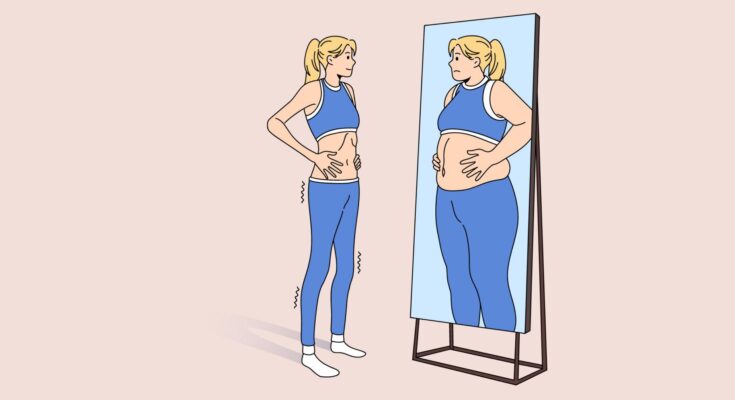
Body Dysmorphic Disorder Treatment: Body Dysmorphic Disorder (BDD) is a complex psychological condition where a person spends a lot of time worrying about flaws in their appearance.
These flaws are often unnoticeable to others. Understanding BDD is crucial for effective diagnosis and treatment.
This comprehensive guide delves into the intricacies of BDD, offering insight into its diagnosis, treatment options, and management strategies.
What is Body Dysmorphic Disorder?
Body Dysmorphic Disorder (BDD) is a mental health condition characterized by an obsessive focus on perceived flaws in one’s appearance. These flaws are often minor or invisible to others, yet for individuals with BDD, they can become the center of intense and distressing preoccupation. This disorder can lead to significant emotional distress and impact daily functioning.
BDD is more than just an insecurity or a lack of confidence. It’s a chronic condition where the affected individual constantly worries about their looks, often for hours each day. These concerns can focus on any part of the body but commonly involve the skin, hair, or nose. People with BDD may frequently check their appearance in mirrors, seek reassurance about their looks, or engage in behaviors to fix or hide the perceived flaw.
The condition is often accompanied by a high level of shame, anxiety, and sometimes depression. BDD can affect anyone, regardless of age or gender, and has been linked to other mental health disorders like social anxiety, depression, and obsessive-compulsive disorder (OCD).
Statistics: Prevalence and Demographics Affected
Body Dysmorphic Disorder affects a significant portion of the population, with estimates suggesting that about 1-2% of the general population suffers from BDD. However, these figures might be higher as the condition often goes undiagnosed due to the shame and secrecy that surround it.
BDD can begin in adolescence and continue into adulthood. It affects both men and women, though there may be slight differences in the focus of their preoccupation (e.g., women may focus more on their skin and weight, while men might be more concerned about hair loss and body build). It’s also been observed across various cultures and ethnicities, indicating that BDD is a global issue, not limited to any specific demographic.
The condition is also prevalent among certain groups. For example, higher rates of BDD have been reported in people seeking cosmetic procedures. It’s important to understand that BDD is a serious mental health issue that requires appropriate treatment and support. Early diagnosis and intervention can significantly improve the quality of life for those suffering from this disorder.
Signs and Symptoms of Body Dysmorphic Disorder (BDD)
Understanding the signs and symptoms of BDD is crucial for early identification and treatment. Here, we delve into the common signs, differentiate BDD from normal body image concerns, and explore its psychological and emotional impacts.
Common Signs and Symptoms of BDD
- Persistent Preoccupation: Individuals with BDD have a relentless fixation on specific body parts or features, believing them to be ugly, abnormal, or deformed.
- Excessive Grooming: Engaging in excessive grooming rituals, such as excessive makeup application, hair styling, or skin picking, is common.
- Mirror Checking: Frequent or prolonged mirror checking, or conversely, avoiding mirrors altogether.
- Camouflaging: Attempts to hide perceived flaws with clothing, makeup, or body positioning.
- Seeking Reassurance: Regularly seeking reassurance about appearance from others.
- Social Withdrawal: Avoiding social situations due to embarrassment or fear of judgment about one’s appearance.
- Repeated Cosmetic Procedures: Undergoing multiple, often unnecessary, cosmetic surgeries to “fix” perceived flaws.
Differentiating BDD from Normal Body Image Concerns
While it’s normal to have concerns about one’s appearance, BDD is distinguished by the excessive nature and intensity of the worry. In BDD, concerns about appearance dominate one’s thoughts and often lead to significant distress, impacting daily functioning. Unlike typical dissatisfaction with one’s appearance, BDD involves intrusive, unwanted thoughts and repetitive behaviors related to perceived appearance flaws.
Psychological and Emotional Impacts
The effects of BDD extend beyond physical appearance concerns:
- Anxiety and Depression: High levels of anxiety and depression are common in individuals with BDD.
- Low Self-Esteem: Persistent negative thoughts about one’s body image contribute to a deep sense of inadequacy and low self-esteem.
- Relationship Challenges: BDD can strain personal relationships due to the individual’s self-consciousness and need for reassurance.
- Risk of Substance Abuse: To cope with the distress, some individuals with BDD may resort to substance abuse.
- Suicidal Thoughts: In severe cases, BDD can lead to suicidal ideation or attempts.
Recognizing these signs and seeking professional help is vital for managing BDD. If you or someone you know exhibits these symptoms, consulting a mental health professional can provide the necessary support and treatment.
Causes and Risk Factors of Body Dysmorphic Disorder (BDD)
Body Dysmorphic Disorder (BDD) is a complex mental health condition where an individual obsessively focuses on perceived flaws in their appearance, often not noticeable to others. Understanding the causes of BDD is critical for effective treatment and support.
- Genetic Factors: Research indicates a possible genetic link in BDD. Individuals with a family history of BDD or related disorders might be at a higher risk. This genetic predisposition suggests that certain individuals are more likely to develop BDD due to their biological makeup.
- Environmental Influences: Environmental factors play a significant role in the development of BDD. Traumatic events, such as bullying or abuse, can trigger or exacerbate the condition. Additionally, growing up in a family or social environment that places excessive emphasis on physical appearance can contribute to the development of BDD.
- Psychological Elements: Psychological factors, including low self-esteem and perfectionism, are closely associated with BDD. Individuals who are overly critical of themselves and those with a tendency towards obsessive-compulsive behaviors are more likely to develop this disorder.
The Role of Media and Societal Pressures
Constant exposure to idealized body standards through social media, advertising, and entertainment can create unrealistic expectations about physical appearance. This relentless bombardment of ‘ideal’ body images can lead to dissatisfaction with one’s own body, potentially triggering BDD symptoms in vulnerable individuals.
- Media Influence: The portrayal of beauty and body standards in the media often leads to a skewed perception of what is normal and desirable. This can result in individuals feeling inadequate and obsessing over altering their appearance.
- Societal Expectations: Societal norms and expectations about appearance and beauty can pressure individuals to conform to certain standards. When these standards are not met, it can lead to feelings of inadequacy and heightened self-consciousness, fueling BDD.
However, Body Dysmorphic Disorder is a multifaceted condition influenced by genetic, environmental, and psychological factors. The role of media and societal pressures in shaping body image perceptions cannot be overlooked. Recognizing these influences is vital in understanding, preventing, and treating BDD effectively.
Diagnosing Body Dysmorphic Disorder
BDD, a complex mental health condition, involves a preoccupation with one or more perceived flaws in physical appearance, which are often unnoticeable to others. This can lead to significant distress and impact on daily functioning.
Criteria for Diagnosis: DSM-5 Guidelines
The diagnosis of Body Dysmorphic Disorder is grounded in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). The key criteria include:
- Obsessive Focus on Perceived Flaws: The individual obsesses over perceived defects or flaws in their appearance, which are often slight or invisible to others.
- Repetitive Behaviors: Engaging in repetitive behaviors like mirror checking, excessive grooming, or skin picking, driven by appearance concerns.
- Clinical Significance: The preoccupation causes clinically significant distress or impairment in social, occupational, or other important areas of functioning.
- Differentiation from Other Disorders: The preoccupation is not better accounted for by concerns with body fat or weight in an eating disorder.
Understanding these criteria helps in accurately identifying BDD, distinguishing it from related disorders such as anorexia nervosa or obsessive-compulsive disorder.
Common Challenges and Misconceptions in Diagnosing BDD
Diagnosing BDD presents unique challenges. Common misconceptions include:
- Mislabeling as Vanity: BDD is often mistakenly seen as vanity, but it’s a serious mental health issue.
- Confusion with Other Disorders: Symptoms of BDD can overlap with other mental health conditions, leading to misdiagnosis.
- Patient Hesitancy: Individuals with BDD may be reluctant to seek help due to embarrassment or the belief that their concerns are valid.
Awareness and education about BDD are crucial in overcoming these challenges.
The Role of Healthcare Professionals in Diagnosis
Healthcare professionals play a pivotal role in the diagnosis of BDD. They are responsible for:
- Conducting Thorough Evaluations: This includes detailed patient history and symptom assessment.
- Providing Education: Informing patients about BDD and dispelling myths and misconceptions.
- Referral and Treatment: Guiding patients to appropriate mental health services and support.
However, diagnosing Body Dysmorphic Disorder requires a nuanced understanding of its DSM-5 criteria, an awareness of common diagnostic challenges, and an active role by healthcare professionals in recognizing and addressing this condition.
Treatment Options for Body Dysmorphic Disorder
Body Dysmorphic Disorder (BDD), a mental health condition where a person obsesses over perceived flaws in their appearance, often requires comprehensive treatment. Understanding the available options can significantly help in managing and overcoming BDD.
Psychotherapy
Cognitive Behavioral Therapy (CBT) is the cornerstone of psychotherapy for BDD. This approach focuses on identifying negative thoughts and beliefs about one’s body image and learning how to change these perceptions. CBT aims to reduce obsessive behaviors and improve self-esteem. It often involves:
- Exposure and Response Prevention (ERP): Patients are gradually exposed to anxiety-provoking situations and taught to refrain from the compulsive behaviors typically used to alleviate anxiety.
- Mindfulness Techniques: These help patients stay grounded in the present moment, reducing obsessive thoughts.
Medication
Medications, particularly Selective Serotonin Reuptake Inhibitors (SSRIs), are frequently prescribed for BDD. SSRIs can help reduce the obsessive-compulsive behaviors and anxiety associated with BDD. Common SSRIs include:
- Fluoxetine (Prozac)
- Sertraline (Zoloft)
- Paroxetine (Paxil)
It’s important to note that medications may have side effects and should be taken under the guidance of a healthcare professional.
Personalized Treatment Plans
Every individual’s experience with BDD is unique, making personalized treatment plans vital. These plans typically involve a combination of psychotherapy and medication, tailored to the individual’s specific needs and symptoms. The importance of a personalized approach cannot be overstated, as it:
- Addresses the unique patterns of thought and behavior in each patient.
- Considers the individual’s overall mental health, co-occurring disorders, and personal preferences.
- Allows flexibility in treatment, adapting to changes in the patient’s condition and response to therapy.
However, while BDD can be challenging, effective treatment options like psychotherapy, particularly CBT, and medication, mainly SSRIs, are available. A personalized treatment plan, devised in collaboration with healthcare professionals, can lead to a successful management and recovery from BDD.
Living with Body Dysmorphic Disorder
Living with BDD can be challenging, but with the right strategies and support, individuals can manage symptoms effectively and lead fulfilling lives.
Managing Symptoms: Daily Strategies and Self-Care
- Mindfulness and Meditation: Regular mindfulness practices can help individuals with BDD ground themselves in the present moment and reduce negative thoughts about their body image.
- Routine Exercise: Engaging in physical activity not only improves physical health but also boosts mental well-being.
- Healthy Eating Habits: A balanced diet contributes to overall health, impacting how one feels and perceives their body.
- Setting Realistic Goals: Establishing achievable goals can provide a sense of accomplishment and help shift focus away from appearance.
- Cognitive Behavioral Therapy (CBT): CBT is particularly effective in treating BDD, as it addresses the negative thought patterns associated with the disorder.
Support Systems: Family, Friends, and Support Groups
- Open Communication: Sharing feelings and experiences with trusted family members and friends can provide emotional relief and understanding.
- Professional Counseling: Seeking professional help can offer personalized strategies and coping mechanisms.
- Support Groups: Joining BDD-specific support groups provides a community of individuals who understand and share similar experiences, fostering a sense of belonging and mutual support.
Long-Term Outlook and Managing Relapses
- Ongoing Therapy: Continued engagement in therapy can help maintain progress and manage any potential relapses.
- Education and Awareness: Staying informed about BDD helps in recognizing early signs of relapse, allowing for prompt intervention.
- Self-Acceptance Practices: Cultivating a practice of self-acceptance and self-compassion can significantly impact long-term outlook positively.
- Lifestyle Adjustments: Making lifestyle changes that prioritize mental health is crucial for long-term management.
Living with Body Dysmorphic Disorder is a journey that involves learning, growing, and adapting. With effective daily strategies, a strong support system, and a focus on long-term management, individuals with BDD can navigate the challenges of the disorder and lead a healthier, more balanced life.
Advancements in Body Dysmorphic Disorder Treatment
Recent Research and Developments in BDD Treatment
Recent research has led to a deeper understanding of BDD, paving the way for more effective interventions. Cognitive-behavioral therapy (CBT) remains a cornerstone in treating BDD, with studies showcasing its ability to alter negative thought patterns and behaviors associated with body image concerns. In addition to traditional CBT, exposure therapy, and response prevention have also been gaining traction. These techniques help individuals confront their body image fears in a controlled environment, reducing avoidance behaviors.
Pharmacotherapy has made strides as well. Selective serotonin reuptake inhibitors (SSRIs), typically used for depression and anxiety, have shown promise in alleviating BDD symptoms. Research into the neurobiological underpinnings of BDD has opened doors for potential new drug therapies targeting specific brain pathways involved in obsessive-compulsive behaviors.
Teletherapy and digital interventions have become increasingly relevant, especially in the wake of the COVID-19 pandemic. Online CBT programs and support groups provide accessible options for those who might face barriers to traditional in-person therapy.
Emerging Therapies and Future Prospects
The future of BDD treatment looks promising, with emerging therapies exploring novel approaches. One such area is the use of virtual reality (VR) to create immersive environments for exposure therapy. VR can simulate real-life scenarios that individuals with BDD might find triggering, allowing for a safe space to practice coping strategies.
Mindfulness-based therapies are also gaining attention. These approaches focus on cultivating present-moment awareness and acceptance, helping individuals with BDD to break free from the cycle of obsessive thoughts and compulsive behaviors related to their body image.
Genetic research offers another exciting avenue. Understanding the genetic factors that contribute to BDD could lead to more personalized treatment strategies, tailoring interventions to individual genetic profiles.
However, the landscape of BDD treatment is evolving rapidly, with a blend of traditional and innovative approaches showing promise. As research continues to uncover the complexities of this disorder, the prospects for more effective and personalized treatments grow, offering new hope to those affected by BDD.
Conclusion:
Encouragement is key in breaking these stigmas. If you or someone you know is struggling with symptoms of BDD, it’s important to seek professional help. Mental health professionals can provide effective treatments, such as cognitive-behavioral therapy, which have been proven to alleviate the symptoms of BDD. Remember, seeking help is a sign of strength, not weakness.
Moreover, fostering an environment where open discussions about mental health are normalized can greatly contribute to reducing the stigma surrounding BDD and other mental health conditions. This can encourage more people to seek the help they need without fear of judgment or misunderstanding.
In summary, recognizing and treating Body Dysmorphic Disorder is essential. It’s a journey that requires courage, support, and professional guidance. By seeking help and advocating for greater awareness, we can break down the barriers of stigma and move towards a healthier, more understanding society.