Burning Mouth Syndrome Treatment: Burning Mouth Syndrome (BMS) is a complex, vexing condition characterized by a persistent burning sensation in the mouth without any obvious cause.
This condition can affect anyone, but it predominantly occurs in middle-aged or older women.
Understanding BMS, its potential causes, diagnosis, and effective treatment strategies is crucial for those suffering from this condition.
What is Burning Mouth Syndrome?
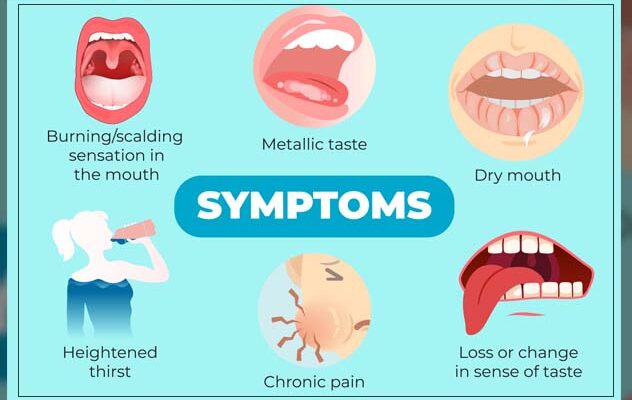
Burning Mouth Syndrome (BMS) is a complex and often misunderstood condition characterized by a persistent burning sensation in the mouth. This sensation can affect the tongue, gums, lips, inside of the cheeks, roof of the mouth, or widespread areas of the whole mouth. BMS is sometimes accompanied by a dry mouth sensation and/or a bitter or metallic taste.
Statistics: Prevalence and Demographics Affected
Burning Mouth Syndrome predominantly affects middle-aged and older adults, with a higher incidence reported among women, especially postmenopausal women. Although exact prevalence rates vary, studies suggest that BMS affects around 0.7% to 4.6% of the population. It is less common in younger individuals and in men. The condition can have a significant impact on the quality of life, affecting daily activities and mental health due to the chronic nature of the pain. Understanding the demographics and prevalence of BMS is crucial for healthcare providers in order to offer appropriate diagnosis and treatment.
Causes of Burning Mouth Syndrome
Understanding the potential causes is crucial for both patients and healthcare providers. Here’s a comprehensive list of potential causes that contribute to the development of BMS:
1. Hormonal Changes: Particularly in women, hormonal fluctuations during menopause can trigger BMS.
2. Nutritional Deficiencies: Deficiencies in essential nutrients like iron, zinc, and certain B vitamins (B1, B2, B6, B9, B12) can lead to symptoms of BMS.
3. Dry Mouth (Xerostomia): This condition reduces saliva production, leading to a dry mouth, which can cause or exacerbate BMS.
4. Oral Health Issues: Conditions such as oral thrush, geographic tongue, or dentures can contribute to BMS.
5. Medications and Medical Treatments: Certain medications, especially those for high blood pressure, can trigger BMS. Medical treatments like chemotherapy and radiation may also be contributing factors.
6. Allergies or Reactions to Foods, Food Additives, or Dental Work Materials: Some individuals may react to certain foods, flavors, preservatives, or even materials used in dental procedures.
7. Neurological Disorders: Conditions affecting the nerves, such as neuropathy, can lead to BMS symptoms.
8. Acid Reflux: Gastroesophageal reflux disease (GERD) can cause stomach acid to enter the mouth, potentially leading to BMS.
9. Stress and Anxiety: Emotional factors like stress and anxiety can manifest physically, leading to symptoms like those of BMS.
10. Endocrine Disorders: Conditions like diabetes or thyroid disorders can be associated with BMS.
11. Oral Habits: Habits like teeth grinding (bruxism) or tongue thrusting can contribute to BMS.
12. Infections: Certain viral infections, particularly in the herpes family, have been linked to BMS.
13. Immune System Disorders: Autoimmune conditions and immune system problems can sometimes cause BMS.
By identifying the underlying cause, appropriate treatment can be sought to alleviate the symptoms of BMS. If you’re experiencing a persistent burning sensation in your mouth, it’s important to consult with a healthcare professional for a proper diagnosis and treatment plan.
Diagnosing Burning Mouth Syndrome (BMS): Essential Steps and Procedures
For individuals experiencing a persistent burning sensation in the mouth, understanding the steps involved in diagnosing BMS is crucial. This article outlines the essential steps and highlights the importance of professional evaluation to differentiate BMS from other oral conditions.
Steps in Diagnosing Burning Mouth Syndrome
- Patient Interview and History: The process begins with a thorough patient interview. Healthcare providers will inquire about the onset, duration, and severity of symptoms. They also gather information about any existing medical conditions, medications, dietary habits, and lifestyle factors that could contribute to the symptoms.
- Clinical Examination: Despite BMS not displaying visible oral signs, a comprehensive oral examination is necessary. This helps rule out other conditions like oral thrush, geographic tongue, or vitamin deficiencies that may cause similar symptoms.
- Tests and Investigations: Depending on the individual’s history and clinical findings, various tests may be recommended. These can include blood tests to check for nutritional deficiencies, hormonal imbalances, or signs of infection. Allergy testing may also be conducted to rule out allergic reactions causing oral discomfort.
- Specialist Referrals: In some cases, referrals to specialists such as dentists, neurologists, or ENT doctors may be necessary. These professionals can provide more in-depth evaluations, particularly if underlying conditions like neuralgia or hormonal disorders are suspected.
Differentiating BMS from Other Oral Conditions
Differentiating BMS from other oral health issues is a critical step in the diagnostic process. Conditions like dry mouth (xerostomia), oral lichen planus, or certain types of oral cancer can mimic the symptoms of BMS. A detailed examination and appropriate tests are essential to distinguish BMS from these conditions.
Importance of Professional Evaluation
Professional evaluation is paramount in diagnosing BMS. Self-diagnosis or delay in seeking professional help can lead to mismanagement of the condition and unnecessary suffering. Healthcare providers not only help in accurately diagnosing BMS but also in developing a comprehensive treatment plan that may involve pain management, nutritional supplements, or therapies to address potential underlying causes.
However, diagnosing BMS requires a methodical approach involving patient interviews, clinical examinations, specific tests, and possibly specialist referrals. Differentiating it from other oral conditions is essential for accurate diagnosis and treatment. Professional evaluation plays a crucial role in the effective management of BMS, ensuring patients receive the correct diagnosis and appropriate care.
Treatment Options for Burning Mouth Syndrome
Managing BMS can be challenging, but various treatment options are available that can alleviate symptoms and improve quality of life. This section delves into these treatment options, focusing on both traditional medications and the potential benefits of alternative and complementary therapies.
Medications and Their Effectiveness
- Pain Relievers: Over-the-counter pain relievers can offer temporary relief from the discomfort of BMS. However, it’s important to consult with a healthcare professional before starting any medication regimen.
- Antidepressants: Certain low-dose antidepressants have been found effective in reducing mouth pain. Medications like tricyclic antidepressants or selective serotonin reuptake inhibitors (SSRIs) may be prescribed.
- Mouth Rinses: Mouth rinses containing lidocaine or other anesthetics can help numb mouth pain. It’s essential to use these under the guidance of a dentist or doctor.
- Saliva Replacements: For individuals with dry mouth symptoms, saliva replacements or medications that stimulate saliva production can be beneficial.
- Vitamin Supplements: If BMS is linked to nutritional deficiencies, vitamin supplements, particularly B vitamins, may be recommended.
- Capsaicin: A substance found in chili peppers, capsaicin, has been shown to alleviate pain in some people with BMS. It can be applied topically inside the mouth.
Alternative and Complementary Therapies
- Cognitive Behavioral Therapy (CBT): CBT can help manage the psychological impact of BMS, teaching coping strategies to deal with chronic pain.
- Acupuncture: Some patients find relief with acupuncture, which involves inserting thin needles into specific points on the body to relieve pain.
- Dietary Adjustments: Avoiding spicy, acidic foods and beverages can reduce irritation in the mouth. Additionally, increasing intake of foods rich in vitamins and minerals may help.
- Stress Management: Techniques like yoga, meditation, and deep-breathing exercises can help manage stress, which may exacerbate BMS symptoms.
- Herbal Remedies: Aloe vera, honey, and chamomile have been used traditionally to soothe oral discomfort, though more research is needed in their effectiveness for BMS.
- Hydration: Keeping well-hydrated can alleviate dry mouth symptoms associated with BMS.
Burning Mouth Syndrome can significantly impact daily life, but there are various treatment options available to manage its symptoms. While medications play a crucial role, alternative and complementary therapies can also provide significant relief. It’s important to work closely with healthcare professionals to tailor a treatment plan that suits your individual needs and effectively manages your symptoms.
Lifestyle and Home Remedies for Burning Mouth Syndrome
Self-Care Strategies for Symptom Relief
- Stay Hydrated: Keeping your mouth moist can help alleviate the burning sensation. Drink plenty of water throughout the day.
- Avoid Tobacco and Alcohol: Both can exacerbate symptoms. If you smoke or consume alcohol, consider reducing or eliminating these habits.
- Practice Good Oral Hygiene: Use a soft-bristled toothbrush and avoid mouthwashes containing alcohol. Good oral care can prevent additional mouth irritations.
- Manage Stress: Stress can worsen the symptoms of burning mouth syndrome. Techniques such as yoga, meditation, or other relaxation methods can be beneficial.
- Chew Sugarless Gum: This stimulates saliva flow, which can help keep your mouth moist and reduce discomfort.
- Avoid Overly Hot Foods and Beverages: They can aggravate your symptoms. Opt for foods and drinks that are at a comfortable temperature.
- Use Saliva Substitutes: Over-the-counter artificial saliva products can help in keeping your mouth moist.
- Consult with a Healthcare Professional: If symptoms persist, it’s important to seek advice from a dentist or doctor for potential treatments or underlying health issues.
Dietary Considerations and Avoidance of Irritants
- Identify and Avoid Trigger Foods: Spicy, acidic, and overly salty foods can trigger or worsen symptoms. Keep a food diary to identify potential triggers.
- Incorporate Soothing Foods: Foods like milk-based products can be soothing. Include mild, bland foods in your diet to minimize discomfort.
- Limit or Avoid Caffeine: Coffee, tea, and some sodas can irritate a sensitive mouth. Try reducing your intake to see if symptoms improve.
- Avoid Acidic Foods and Beverages: Citrus fruits, tomatoes, and certain juices can exacerbate symptoms. Opt for less acidic options.
- Opt for Nutrient-Rich Foods: A balanced diet is important. Ensure you’re getting a variety of nutrients to support overall health.
- Consider Supplements: In some cases, vitamin deficiencies (like B vitamins, iron, and zinc) can contribute to symptoms. Consult with a healthcare provider before starting any supplements.
By incorporating these lifestyle and dietary changes, individuals with burning mouth syndrome can often find symptom relief and improve their overall quality of life. Remember, it’s always best to consult with a healthcare professional for personalized advice and treatment options.
Coping and Support for Burning Mouth Syndrome (BMS)
Individuals with BMS often experience frustration, anxiety, and depression due to the persistent discomfort and the challenge of finding effective treatments. The lack of visible symptoms can lead to a sense of isolation and misunderstanding from others.
Tips for Coping with BMS
- Seek Professional Help: It’s crucial to consult healthcare providers who are familiar with BMS. They can offer tailored treatment plans and rule out underlying causes.
- Connect with Support Groups: Sharing experiences with others who have BMS can be incredibly comforting. Support groups provide a platform to exchange coping strategies and emotional support.
- Practice Stress Management: Stress can exacerbate BMS symptoms. Techniques like meditation, yoga, and deep breathing can help manage stress levels.
- Adopt a Healthy Lifestyle: Eating a balanced diet, staying hydrated, and avoiding tobacco and spicy foods can mitigate symptoms. Regular exercise also helps in reducing stress.
- Focus on Oral Care: Gentle oral hygiene practices can minimize discomfort. Avoid alcohol-based mouthwashes and opt for products designed for sensitive mouths.
- Educate Friends and Family: Helping those close to you understand BMS can build a supportive environment.
- Consider Therapy: Cognitive-behavioral therapy (CBT) or counseling can help in dealing with the emotional toll of BMS.
- Explore Alternative Remedies: Acupuncture or vitamin supplements (as advised by a healthcare provider) might offer relief.
- Journaling: Keeping a symptom diary can help in identifying triggers and effective coping strategies.
- Stay Positive: Focus on activities that bring joy and relaxation. A positive mindset can significantly impact how you cope with BMS.
Finding Support for BMS
- Healthcare Professionals: Regular check-ins with your doctor or dentist are essential for monitoring and managing BMS.
- Online Communities: Online forums and social media groups can provide a sense of belonging and valuable information.
- Local Support Groups: Check for local support groups where you can meet others dealing with BMS.
- Mental Health Professionals: Psychologists or therapists specializing in chronic pain can offer coping mechanisms and emotional support.
- Educational Resources: Stay informed about BMS through reputable websites and health blogs.
However, coping with Burning Mouth Syndrome requires a holistic approach, addressing both physical symptoms and emotional well-being. Through professional guidance, support networks, and personal coping strategies, it is possible to manage the symptoms and improve quality of life. Remember, you are not alone in this journey.
Prevention Strategies for Burning Mouth Syndrome
To mitigate the risk of developing this condition, adopting preventive measures is crucial. While there is no guaranteed way to prevent BMS, certain lifestyle adjustments can help reduce the likelihood of its occurrence.
- Oral Hygiene: Maintaining good oral health is essential. Regular brushing, flossing, and using an alcohol-free mouthwash can prevent infections and conditions that might trigger BMS.
- Avoid Irritants: Minimize consumption of spicy, acidic, or overly hot foods and drinks, as they can irritate the mouth lining.
- Quit Smoking: Smoking can exacerbate oral conditions and potentially lead to BMS, so quitting is advisable.
- Stress Management: Since stress can be a contributing factor, incorporating stress-reduction techniques like yoga, meditation, or other relaxation practices can be beneficial.
- Nutritional Balance: Ensure a well-balanced diet, rich in vitamins, especially B vitamins, iron, and zinc, which are crucial for oral health.
The Importance of Regular Dental and Health Check-Ups
Regular dental and health check-ups play a pivotal role in preventing Burning Mouth Syndrome. These check-ups help in:
- Early Detection: Dentists and doctors can identify early signs of conditions that might lead to BMS, such as hormonal imbalances, nutritional deficiencies, or oral infections.
- Professional Guidance: Regular visits allow healthcare professionals to offer personalized advice on oral care, dietary changes, and stress management based on individual health profiles.
- Monitoring Changes: Ongoing assessments help in monitoring any changes in oral health, ensuring timely interventions if potential BMS symptoms are detected.
However, while Burning Mouth Syndrome is a challenging condition, incorporating preventive strategies into daily routines and maintaining regular dental and health check-ups can significantly reduce the risk of its development. Adopting a proactive approach to oral and overall health is key to mitigating the likelihood of experiencing BMS.
Recent Advances in Burning Mouth Syndrome (BMS) Treatment
Burning Mouth Syndrome (BMS) is a complex condition characterized by a burning sensation in the mouth without an identifiable cause. Recent advancements in research have opened new avenues for its management and treatment.
One of the significant developments is the better understanding of the neurological aspects of BMS. Studies have shown that neuropathic mechanisms play a crucial role, leading to the exploration of various neuro-modulating medications. Antidepressants and anticonvulsants, previously used for neuropathic pain, are now being considered for BMS due to their ability to modulate nerve function.
Another promising area is the use of natural and alternative remedies. Omega-3 supplements, known for their anti-inflammatory properties, have shown potential in reducing BMS symptoms. Additionally, the application of capsaicin, a compound found in chili peppers, has been effective in some cases. It works by desensitizing pain receptors in the mouth.
The role of hormonal changes, particularly in post-menopausal women, is another area of research. Hormone replacement therapy has been suggested as a potential treatment for those whose BMS is linked to hormonal imbalances.
Furthermore, the psychological aspect of BMS is receiving more attention. Cognitive-behavioral therapy (CBT) and other psychological interventions are being explored to help patients cope with the chronic pain and stress associated with BMS.
Future Prospects in BMS Management
Looking to the future, personalized medicine appears to be a promising approach. As BMS can have multiple triggers and vary from person to person, treatments tailored to individual needs and underlying conditions are being considered.
Advancements in diagnostic tools are also on the horizon. Improved imaging techniques and more accurate diagnostic criteria are expected to aid in the early detection and better management of BMS.
Finally, ongoing research into the molecular and genetic aspects of BMS holds the promise of more targeted and effective treatments. Understanding the genetic predisposition to BMS could lead to breakthroughs in both prevention and management.
However, while BMS remains a challenging condition to treat, recent research and advancements provide hope for better management strategies and improved quality of life for those affected. The integration of multidisciplinary approaches, encompassing medical, psychological, and lifestyle modifications, is key to the future success of BMS treatment.
FAQs: Understanding and Treating Burning Mouth Syndrome
Q1: What is Burning Mouth Syndrome (BMS)?
A: Burning Mouth Syndrome (BMS) is a complex, painful condition characterized by a burning sensation in the mouth. This sensation can affect the tongue, gums, lips, inside of cheeks, or the whole mouth. BMS is often accompanied by a bitter or metallic taste.
Q2: Who is most at risk for developing BMS?
A: BMS primarily affects middle-aged or older women, but it can occur in anyone. Risk factors include hormonal changes, particularly in postmenopausal women, certain medications, nutritional deficiencies, and chronic medical conditions.
Q3: What are the main symptoms of BMS?
A: The hallmark symptom of BMS is a persistent burning sensation in the mouth. Other symptoms include dry mouth, a bitter or metallic taste, and a change in taste perception. The symptoms can vary in intensity throughout the day.
Q4: How is BMS diagnosed?
A: Diagnosing BMS involves ruling out other conditions that cause similar symptoms. Your doctor may perform a thorough oral examination, blood tests, allergy tests, and salivary flow tests. A detailed medical history is also crucial for diagnosis.
Q5: What treatment options are available for BMS?
A: Treatment for BMS focuses on relieving symptoms. Options may include pain relief medications, mouth rinses, saliva substitutes for dry mouth, and treatments for underlying conditions. Psychological support and stress management techniques can also be beneficial.
Q6: Can dietary changes help with BMS?
A: Yes, dietary changes can help manage BMS symptoms. Avoiding spicy, acidic, or very hot foods and drinks can reduce irritation. Additionally, drinking plenty of water, maintaining good oral hygiene, and avoiding tobacco and alcohol can also help.
Q7: Is BMS a sign of a more serious condition?
A: While BMS itself is not life-threatening, it can be a symptom of other underlying health issues, such as nutritional deficiencies or oral infections. It’s important to consult a healthcare provider for a proper diagnosis and to rule out other conditions.
Q8: How long does BMS last?
A: The duration of BMS varies. For some, it may be temporary, while for others, it can be a chronic condition. The severity and persistence of symptoms can fluctuate over time.
Q9: Are there any natural remedies for BMS?
A: Some natural remedies that might provide relief include alpha-lipoic acid supplements, vitamin B complex, and stress-reduction techniques like yoga and meditation. However, it’s important to discuss these with your healthcare provider before starting any new treatment.
Q10: Where can I find support for BMS?
A: Support groups, either online or in-person, can offer valuable advice and emotional support. Healthcare providers can also provide resources and referrals to specialists in managing BMS.
Conclusion
If you’re experiencing symptoms that align with BMS, it’s essential to consult healthcare professionals. They can provide personalized diagnosis and treatment plans, tailored to your specific needs. Remember, seeking professional help is not just a step towards symptom relief but also towards improving your overall quality of life.
Don’t let the discomfort of Burning Mouth Syndrome overshadow your days. Reach out for professional guidance and take that vital step towards better oral health and well-being.