Blastocystis Hominis Symptoms: Blastocystis hominis is a microscopic organism that can be found in the intestines. Though often considered a parasite, its role as a pathogen remains a subject of debate among medical experts.
In recent years, the prevalence of Blastocystis hominis has attracted attention due to its potential connection to various gastrointestinal symptoms.
What is Blastocystis Hominis?
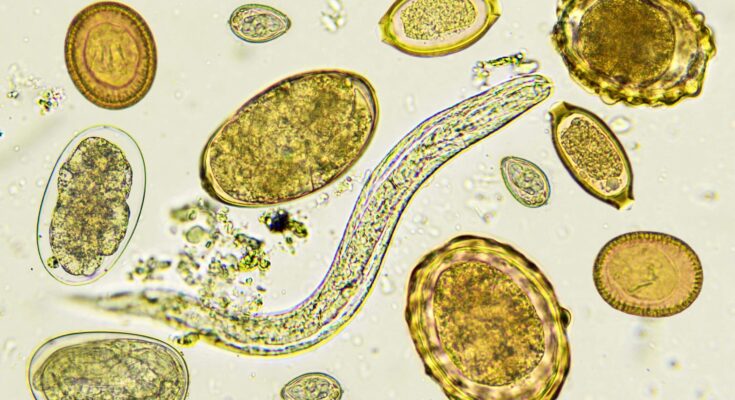
Blastocystis hominis is a microscopic organism classified as a protozoan parasite. It resides primarily in the intestines of humans and a variety of animals. Unlike typical parasites, Blastocystis hominis exhibits a high degree of genetic diversity, leading to variations in its appearance and potential impact on the host. While it is often found in the stool of individuals with and without gastrointestinal symptoms, the role of Blastocystis hominis in causing disease is still a subject of ongoing research and debate.
The organism is characterized by its ability to survive in different forms, including cysts and vacuolar forms. This adaptability allows it to endure various environmental conditions. Notably, Blastocystis hominis can be transmitted through the fecal-oral route, often due to poor hygiene or contaminated water and food sources.
Brief History and Prevalence
The discovery of Blastocystis hominis dates back to the early 20th century, but its significance and classification have evolved over time. Initially, it was not considered a significant pathogen. However, with increasing global travel and attention to waterborne diseases, Blastocystis hominis has gained more recognition in the medical community.
Its prevalence is notable worldwide, with higher occurrence rates in developing countries due to factors like inadequate sanitation and water treatment facilities. The prevalence of Blastocystis hominis varies, but studies suggest it is one of the most common intestinal parasites globally. It’s found in a broad spectrum of the population, including both symptomatic and asymptomatic individuals, making its study both challenging and essential for understanding intestinal health and disease.
Symptoms of Blastocystis Hominis
Blastocystis hominis, a microscopic parasite found in the intestines, can manifest in a range of symptoms, varying in both intensity and duration. Understanding these symptoms is crucial for early detection and effective treatment.
Common Symptoms
The presence of Blastocystis hominis often leads to gastrointestinal discomfort. Key symptoms include:
- Abdominal Pain and Cramps: A frequent and notable symptom, abdominal pain can range from mild discomfort to severe cramps.
- Bloating and Gas: These symptoms are commonly associated with the presence of the parasite, leading to discomfort and abdominal distension.
- Diarrhea: This can vary from mild to severe, often watery, and sometimes alternating with constipation.
- Nausea and Loss of Appetite: Many individuals experience a general feeling of sickness and a decrease in appetite.
- Fatigue: A less specific but still relevant symptom, fatigue can be both physical and mental.
Variations in Symptom Severity and Duration
The symptoms of Blastocystis hominis can vary greatly among individuals:
- Mild Cases: Some people may experience only slight discomfort or no symptoms at all, making the infection hard to detect without a medical examination.
- Severe Cases: In more acute cases, symptoms can be intense and debilitating, requiring immediate medical attention.
- Chronic Infections: In certain individuals, Blastocystis hominis can lead to long-term health issues, with symptoms persisting for weeks or even months.
- Asymptomatic Carriers: Interestingly, some individuals may carry the parasite without showing any symptoms, yet they can still spread the infection to others.
The symptoms of Blastocystis hominis are diverse and can impact individuals differently. Awareness of these symptoms is essential for timely diagnosis and treatment. If you experience any of the above symptoms persistently, it is advisable to consult a healthcare provider for proper diagnosis and treatment.
Causes and Risk Factors of Blastocystis hominis Infection
Blastocystis hominis, a microscopic organism found in stools of infected individuals, is primarily transmitted through the fecal-oral route. This typically occurs when individuals consume food or water contaminated with the parasite. The transmission can also happen through direct contact with contaminated surfaces or hands. Notably, Blastocystis hominis is prevalent in areas with inadequate sanitation and is often found in both developed and developing countries.
Risk Factors for Infection
The risk of acquiring a Blastocystis hominis infection increases under certain conditions. Key risk factors include:
- Poor Hygiene Practices: Inadequate handwashing, especially after using the toilet or handling contaminated materials, significantly raises the risk of infection.
- Consuming Contaminated Food or Water: Eating or drinking contaminated products is a common transmission route, particularly in areas without proper food and water sanitation.
- International Travel: Travelers to regions where the parasite is common, such as some developing countries, are at a higher risk.
- Exposure in Institutions: Outbreaks can occur in institutions like daycare centers or nursing homes due to close contact and potentially shared facilities.
- Weak Immune System: Individuals with compromised immunity, such as those with HIV/AIDS, cancer, or other conditions, may be more susceptible to infection.
Populations Most at Risk
Certain populations are more vulnerable to Blastocystis hominis infections:
- Children: Young children, especially those in daycare centers, are at a higher risk due to their close contact with others and less developed hygiene practices.
- Travelers: People traveling to areas with known prevalence of the parasite, especially those who might consume local water or food, are at an increased risk.
- Residents of Areas with Poor Sanitation: Individuals living in areas lacking proper waste disposal and water treatment facilities are continually exposed to the risk of infection.
- Immunocompromised Individuals: People with weakened immune systems are more likely to contract the infection and may experience more severe symptoms.
Understanding these risk factors and populations at risk is crucial for prevention and management of Blastocystis hominis infections. Awareness and adherence to good hygiene practices, safe food and water consumption, and cautious behavior in high-risk areas can significantly reduce the risk of infection.
Diagnosing Blastocystis Hominis
Blastocystis hominis, a microscopic organism frequently found in the intestines, can be challenging to diagnose. Accurate detection is crucial for effective treatment and understanding its impact on health.
Methods Used for Diagnosis
Stool Tests: The most common method for diagnosing Blastocystis hominis is through stool tests. These tests involve analyzing stool samples for the presence of the organism.
- Direct Microscopic Examination: This involves a direct look at the stool sample under a microscope. It’s a quick method but may miss low levels of the parasite.
- Culture Method: In this method, the stool sample is cultured in specific media to encourage the growth of Blastocystis hominis, making it easier to detect.
- Molecular Methods (PCR): Polymerase Chain Reaction (PCR) tests are more sensitive and can detect even minute quantities of Blastocystis DNA in a stool sample.
Serological Tests: These tests check for antibodies against Blastocystis in the blood. However, they are not commonly used due to their limited availability and the fact that antibody presence does not necessarily indicate an active infection.
Challenges in Diagnosing Based on Symptoms Alone
Non-Specific Symptoms: Symptoms of Blastocystis hominis infection, such as abdominal discomfort, bloating, and diarrhea, are common to many gastrointestinal disorders. This non-specificity makes diagnosis based solely on symptoms unreliable.
Asymptomatic Carriers: Many individuals with Blastocystis hominis do not show any symptoms, further complicating the diagnostic process.
Co-Infections: The presence of other intestinal parasites or bacteria can mask or mimic the symptoms of Blastocystis, leading to misdiagnosis.
Variability in Strains: Different strains of Blastocystis hominis may cause different symptoms, adding another layer of complexity to the diagnosis.
Diagnosing Blastocystis hominis requires a combination of clinical evaluation and laboratory tests. Stool analysis remains the cornerstone of diagnosis, but the non-specific nature of symptoms and the potential for co-infections necessitate a careful and comprehensive approach. Understanding these challenges is key to ensuring accurate diagnosis and effective management of Blastocystis hominis infections.
Complications and Co-infections for Blastocystis hominis
Understanding the potential complications and its relation to other gastrointestinal conditions is crucial for both patients and healthcare providers.
Potential Complications from Untreated Infections
Untreated Blastocystis hominis infections can lead to a range of complications, significantly impacting a person’s health. These complications include:
- Chronic Gastrointestinal Issues: Persistent diarrhea, abdominal pain, and bloating are common symptoms that can escalate into chronic conditions if left untreated.
- Malabsorption Syndrome: This condition occurs when your intestines cannot absorb nutrients properly, leading to malnutrition and weight loss.
- Irritable Bowel Syndrome (IBS): There is growing evidence linking Blastocystis hominis with IBS, a disorder characterized by a combination of abdominal pain and altered bowel habits.
- Compromised Immune System: Chronic infection can weaken the immune system, making the body more susceptible to other infections and diseases.
- Increased Risk of Colitis: Inflammation of the colon, known as colitis, can be exacerbated by ongoing Blastocystis hominis infections.
Relation to Other Gastrointestinal Conditions
Blastocystis hominis doesn’t exist in isolation and often interacts with other gastrointestinal conditions. Understanding these relationships is vital for effective treatment:
- Co-infections: This parasite often coexists with other intestinal parasites and bacteria, complicating diagnosis and treatment.
- Exacerbation of Existing Conditions: Individuals with pre-existing gastrointestinal disorders, such as Crohn’s disease or ulcerative colitis, may experience worsened symptoms due to Blastocystis hominis.
- Interference with Gut Flora: The presence of this parasite can disrupt the normal balance of gut flora, leading to dysbiosis and associated gastrointestinal discomfort.
- Influence on Gut Inflammation: Blastocystis hominis can contribute to increased gut inflammation, affecting overall gut health and potentially triggering other gastrointestinal issues.
However, Blastocystis hominis is not a condition to be taken lightly. Its potential to cause severe complications and its interaction with other gastrointestinal conditions necessitates prompt and effective medical attention. Understanding the risks and interrelations of this parasite can lead to better management and treatment outcomes for those affected.
Treatment Options for Blastocystis hominis
The treatment of Blastocystis hominis involves a range of strategies aimed at alleviating symptoms and eradicating the organism.
Treatment Methods
1. Antiparasitic Medications: The most common treatment involves antiparasitic medications. These include:
- Metronidazole (Flagyl): Frequently the first line of treatment.
- Tinidazole: Similar to metronidazole, used for those who do not respond to the first-line treatment.
- Nitazoxanide: Effective in some cases, especially in children.
- Paromomycin: An alternative for those who cannot tolerate other antiparasitics.
2. Probiotics: Probiotics are suggested to improve gut health and balance the intestinal flora, potentially helping in reducing the symptoms.
3. Dietary Changes: Some patients benefit from dietary changes, such as reducing sugar and increasing fiber intake, to manage symptoms.
Effectiveness and Limitations
- Varied Response to Medication: Not all patients respond to the same medication, and multiple treatments may be necessary.
- Recurrence: There is a risk of recurrence, even after successful treatment.
- Symptomatic Treatment: In many cases, treatment focuses on symptom management rather than eradication of the organism, as Blastocystis hominis is often considered a commensal organism.
- Diagnostic Challenges: The presence of Blastocystis hominis does not always mean it is the cause of symptoms, making treatment decisions complex.
- Lack of Consensus: There is no universal agreement on the treatment approach, reflecting the ongoing research and debate in the medical community.
The treatment of Blastocystis hominis involves a combination of antiparasitic medications, probiotics, and dietary changes. The effectiveness varies among individuals, and the approach is often tailored to the patient’s specific symptoms and response to treatment. Continual research and clinical trials are essential to develop more effective and targeted treatments for this condition.
Prevention Strategies for Blastocystis hominis Infection
Preventing its spread is crucial for maintaining gastrointestinal health. This guide focuses on effective strategies to minimize the risk of Blastocystis hominis infection, highlighting the paramount importance of hygiene and sanitation.
Key Prevention Tips:
- Regular Handwashing: Frequent and thorough handwashing is the cornerstone of preventing Blastocystis hominis infection. Wash hands with soap and water, especially after using the bathroom, changing diapers, and before preparing or eating food.
- Safe Water Consumption: Drinking contaminated water is a common way to contract this parasite. Always consume water from safe, treated sources. When traveling or in areas with questionable water quality, opt for bottled or boiled water.
- Proper Food Handling: Ensure that all food, particularly fruits and vegetables, is washed thoroughly. In regions where Blastocystis hominis is prevalent, avoid eating raw vegetables and fruits that cannot be peeled.
- Travel Precautions: When traveling to areas with lower sanitation standards, be extra vigilant about water and food consumption. Avoid ice in drinks and eat foods that are cooked and served hot.
- Sanitary Living Conditions: Maintaining cleanliness in living spaces, particularly in kitchens and bathrooms, can significantly reduce the risk of parasite transmission.
- Education and Awareness: Educating yourself and your community about the ways Blastocystis hominis is spread can foster better hygiene practices and reduce the risk of infection.
The Role of Hygiene and Sanitation:
Good hygiene and proper sanitation are essential in the battle against Blastocystis hominis. They not only protect individuals but also help in safeguarding entire communities from the spread of this parasite. Implementing these prevention strategies can lead to a significant decrease in the incidence of infections.
By adopting these practical measures, you can effectively minimize the risk of Blastocystis hominis infection and promote a healthier, more hygienic living environment.
FAQs about Blastocystis Hominis: Symptoms and Causes
What is Blastocystis Hominis?
Blastocystis hominis is a microscopic parasite found in the intestines. It’s a common cause of digestive distress in many individuals globally.
Can Blastocystis Hominis Cause Symptoms?
Yes, Blastocystis hominis can cause symptoms in some people. Common symptoms include diarrhea, abdominal pain, bloating, and gas. However, it’s worth noting that not everyone with this parasite will experience symptoms.
How Do You Get Infected with Blastocystis Hominis?
The primary route of infection is fecal-oral transmission. This can happen through consuming contaminated food or water, or through direct contact with infected individuals or animals.
Who is at Risk for Blastocystis Hominis Infection?
Anyone can get infected, but it’s more common in areas with poor sanitation. Travelers to developing countries, people with compromised immune systems, and those in close contact with animals are at higher risk.
Can Blastocystis Hominis Lead to Serious Health Issues?
In most cases, Blastocystis hominis doesn’t lead to serious health issues. However, in people with weakened immune systems, it can cause more severe symptoms and complications.
How is Blastocystis Hominis Diagnosed?
It’s typically diagnosed through stool tests. Your doctor may request a stool sample to identify the presence of the parasite.
What Treatments are Available for Blastocystis Hominis?
Treatment often includes antiparasitic medications. However, treatment may not always be necessary, especially in asymptomatic cases. Always consult a healthcare provider for appropriate advice.
Can Dietary Changes Help with Blastocystis Hominis Symptoms?
Some people find that dietary changes, like increasing fiber intake or avoiding certain foods, can help manage symptoms. However, this varies from person to person.
Is it Possible to Prevent Blastocystis Hominis Infection?
Yes, practicing good hygiene, such as washing hands regularly and ensuring safe food and water consumption, can reduce the risk of infection.
Can Blastocystis Hominis Go Away on Its Own?
In some individuals, the infection may resolve without treatment. However, if symptoms persist or worsen, it’s important to seek medical advice.
Conclusion
We strongly encourage anyone experiencing symptoms possibly linked to Blastocystis hominis to consult with a healthcare professional. Self-diagnosis and treatment can often lead to mismanagement of the condition and possibly exacerbate the situation. A medical expert can provide accurate diagnosis and appropriate treatment plans, tailored to individual needs and health profiles.
Remember, while information online, including our comprehensive coverage of Blastocystis hominis, can be informative and enlightening, it should never replace professional medical advice. Health concerns should always be addressed by consulting with trained medical practitioners who can offer the most relevant and safe treatment options.
In closing, awareness and understanding of Blastocystis hominis are vital. However, the key to effectively managing its potential impact lies in seeking and following professional medical guidance. Stay informed, but more importantly, stay in touch with healthcare providers to ensure the best care for your health and wellbeing.