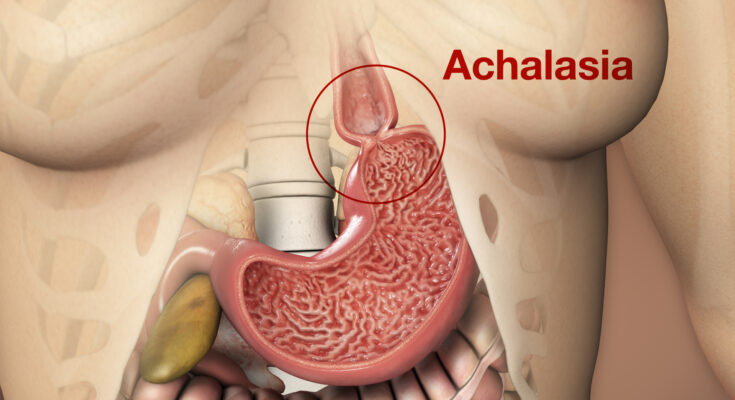
Achalasia Symptoms: Achalasia is a rare but serious esophageal disorder that affects the tube connecting your mouth and stomach, known as the esophagus.
It involves the inability of the esophagus to move food into the stomach and the lower esophageal sphincter, a valve, failing to open up properly.
What is Achalasia?
Definition and Brief Explanation:
Achalasia is a rare esophageal disorder affecting the tube that connects your throat to your stomach. It’s characterized by a failure of the lower esophageal sphincter (LES) to relax properly, hindering the normal movement of food and liquid into the stomach. This results in difficulties swallowing, regurgitation, and sometimes chest pain.
Differentiating Achalasia from Other Similar Conditions:
Achalasia might initially seem like other conditions given its symptoms, but there are distinct differences:
1. GERD (Gastroesophageal Reflux Disease): While both achalasia and GERD can cause regurgitation and chest pain, GERD is primarily caused by stomach acid flowing back into the esophagus, leading to heartburn and a sour taste in the mouth.
2. Esophageal Spasm: This condition involves painful, irregular contractions of the esophagus, whereas achalasia revolves around the inability of the LES to relax and coordinate contractions properly.
3. Esophageal Stricture: A narrowed esophagus due to scarring or inflammation can cause swallowing problems, but it lacks the characteristic LES dysfunction seen in achalasia.
By understanding these nuances, one can better differentiate achalasia from other esophageal conditions. Early diagnosis and treatment can help manage symptoms and improve quality of life.
Achalasia Symptoms
Recognizing these symptoms early on is crucial for timely treatment and better outcomes.
A. Early Symptoms
1. Difficulty Swallowing (Dysphagia): One of the first signs is a noticeable difficulty or discomfort when swallowing. It may feel as though food is getting stuck in the throat or chest.
2. Regurgitation of Undigested Food: This isn’t the typical acid reflux. Instead, individuals may find undigested food coming back up, sometimes hours after eating.
3. Chest Pain or Discomfort: This can often be mistaken for heart-related issues. The pain is usually more pronounced after eating.
4. Heartburn-like Symptoms: While it may feel like common heartburn, these symptoms are due to the esophagus’s inability to move food down effectively.
B. Advanced Symptoms
As achalasia progresses, the symptoms can become more severe and potentially lead to additional health risks.
1. Weight Loss: Due to swallowing difficulties, many people start to eat less and can experience unintentional weight loss.
2. Cough, Especially at Night or When Lying Down: The regurgitation can lead to coughing fits, especially when in a horizontal position.
3. Increased Risk of Aspiration: This is a concerning symptom where food or drink is inhaled into the lungs, leading to potential respiratory issues.
C. Complications from Ignored Symptoms
If left untreated or if symptoms are ignored, achalasia can result in significant complications:
1. Esophageal Damage or Sores (Ulcers): The constant irritation from undigested food and stasis can damage the esophageal lining, leading to painful ulcers.
2. Increased Risk of Esophageal Cancer: Over time, the chronic irritation and damage increase the risk of developing esophageal cancer.
If you or someone you know is experiencing these symptoms, it’s essential to consult a healthcare professional for proper diagnosis and treatment.
Causes of Achalasia
To understand the causes of achalasia, it’s essential to break them down into their primary factors.
A. Loss of Nerve Cells
The esophagus, a tube that connects your mouth to your stomach, relies on coordinated muscular activity to move food and liquid downward. This muscle movement is orchestrated by a network of nerve cells.
When there is a loss of these nerve cells, the esophagus cannot function correctly. The muscle movements become uncoordinated, and the lower esophageal sphincter (a muscular ring at the base of the esophagus) fails to relax properly. This leads to the typical symptoms of achalasia like difficulty swallowing.
B. Possible Triggers for Nerve Damage
While the exact cause of this nerve damage remains unclear, several potential triggers have been identified:
1. Viral infections: Some researchers believe certain viral infections may instigate the nerve damage.
2. Autoimmune response: In some cases, the body’s immune system might mistakenly target and damage the esophagus’s nerve cells.
3. Genetic predisposition or inheritance: Some people might be more susceptible to achalasia due to their genes, especially if they have a family history of the condition.
C. Risk Factors
Certain factors can increase the risk of developing achalasia, such as:
1. Age: While achalasia can affect people of all ages, it’s often diagnosed in middle-aged or older adults.
2. Family history: Individuals with a family history of achalasia might be at a higher risk.
3. Other associated medical conditions: Conditions like weight loss, cough (especially at night or when lying down), and an increased risk of aspiration (inhaling food or drink into the lungs) can also hint at the presence of achalasia.
D. Complications from Ignored Symptoms
Ignoring the symptoms of achalasia can lead to more severe complications, including:
1. Esophageal damage or sores (ulcers): Chronic retention of food in the esophagus can lead to the formation of ulcers.
2. Increased risk of esophageal cancer: Long-standing achalasia might increase the risk of esophageal cancer, though this risk is relatively low.
It’s crucial to consult a healthcare professional if you experience symptoms of achalasia. Early diagnosis and treatment can help manage the condition and prevent severe complications.
Differentiating Achalasia from Other Conditions
When it comes to digestive disorders, the symptoms can often be alarmingly similar. This overlap makes accurate diagnosis not just important, but essential. One such condition that often gets mistaken due to its symptomatology is achalasia.
Common Conditions with Similar Symptoms
One prime example of a condition that shares symptoms with achalasia is Gastroesophageal Reflux Disease (GERD). Both conditions can present with difficulty swallowing, chest pain, and regurgitation of food or liquids. However, while GERD is often a result of stomach acid flowing back into the esophagus, achalasia is caused by a failure of the esophageal muscles and the lower esophageal sphincter to work properly.
Importance of Correct Diagnosis for Effective Treatment
Misdiagnosis can lead to ineffective treatments and prolonged patient suffering. Treating GERD typically involves acid suppression medications, but these can be of little help to someone with achalasia. On the other hand, achalasia might require interventions such as dilation of the esophagus or even surgery. Therefore, it’s paramount to distinguish between these conditions to ensure that the patient receives the right care.
However, while the symptoms might appear similar on the surface, the underlying causes of digestive disorders like achalasia and GERD are distinct. A correct diagnosis is pivotal to determining the most effective treatment plan, emphasizing the need for thorough medical evaluation.
Frequently Asked Questions on Achalasia
What is Achalasia?
Achalasia is a rare disorder of the esophagus, where the muscles fail to function normally, leading to difficulties in swallowing and sometimes chest pain.
What causes Achalasia?
The exact cause remains unknown. However, it’s believed to be due to the loss of nerve cells in the esophagus, which can be due to factors like genetics, autoimmune responses, or infections.
What are the symptoms of Achalasia?
Common symptoms include difficulty swallowing, regurgitation of undigested food, chest pain, weight loss, and heartburn.
How is Achalasia diagnosed?
Doctors usually diagnose Achalasia through a combination of symptoms, barium swallow studies, endoscopy, and esophageal manometry.
How is Achalasia treated?
Treatment options can vary but may include medications, Botox injections, balloon dilation, or surgery like Heller myotomy.
Is Achalasia life-threatening?
While Achalasia is not directly life-threatening, untreated cases can lead to severe weight loss, malnutrition, and the risk of aspiration pneumonia.
Can you live a normal life with Achalasia?
With appropriate treatment and management, many individuals with Achalasia can lead a near-normal life, although dietary and lifestyle modifications might be needed.
Is Achalasia hereditary?
While the exact cause is still under research, there’s no concrete evidence suggesting that Achalasia is hereditary. However, there have been rare familial cases reported.
How common is Achalasia?
Achalasia is considered rare, affecting about 1 in every 100,000 people annually.
Can Achalasia be prevented?
Since the exact cause remains uncertain, there’s no known way to prevent Achalasia. However, early diagnosis and treatment can manage its symptoms effectively.
Conclusion
In wrapping up, it’s imperative to underscore the significance of detecting the symptoms of achalasia at the earliest stage. Early recognition can make all the difference in managing this condition effectively.
If you or someone you know is experiencing any of these symptoms, don’t hesitate—seek medical attention promptly. Knowledge is power, so we urge you to delve deeper into this topic or share this article with others.
By spreading awareness, you could make a positive impact in someone’s life. Let’s work together to shine a light on achalasia and support those affected by it.