Bell’s Palsy Treatment: Bell’s Palsy is a neurological condition characterized by sudden, temporary weakness or paralysis on one side of the face.
This condition can affect anyone, regardless of age or gender, and its onset is often rapid and unexpected.
Understanding the diagnosis and treatment options for Bell’s Palsy is crucial for patients and healthcare providers alike.
What is Bell’s Palsy?
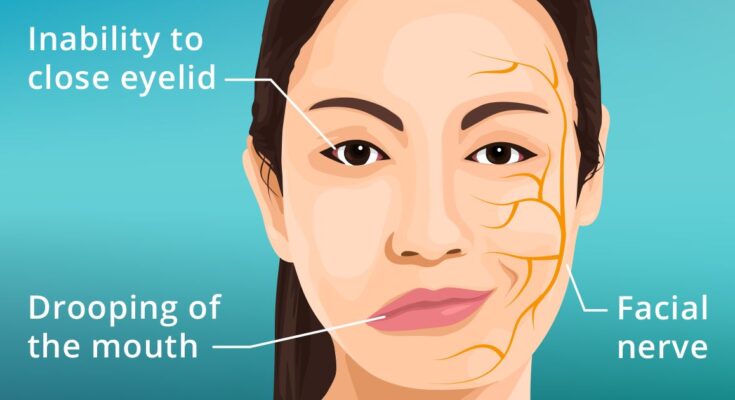
Bell’s Palsy is a medical condition characterized by sudden, temporary weakness or paralysis of the facial muscles. This often results in one side of the face appearing to droop or become stiff. Typically, Bell’s Palsy affects only one side of the face, and the exact cause is not always clear, though it’s often linked to viral infections.
Definition and Basic Understanding of Bell’s Palsy
Bell’s Palsy is defined as a form of temporary facial paralysis or weakness on one side of the face. This condition can occur when the nerve that controls facial muscles becomes inflamed, swollen, or compressed. The onset of Bell’s Palsy is often rapid, and its symptoms can vary from mild facial weakness to complete paralysis of one side of the face.
Statistics on Prevalence and Demographics Affected
Bell’s Palsy is a relatively common condition, affecting about 40,000 Americans each year. It can occur at any age, but it is more prevalent in people between 15 and 60 years old. The condition affects men and women equally and can occur in all ethnic groups. Pregnant women and individuals with respiratory illnesses, diabetes, or a family history of Bell’s Palsy are at a slightly higher risk.
This neurological disorder, while alarming, is usually temporary. Most people with Bell’s Palsy recover fully with or without treatment, often within three to six months. However, a small percentage of individuals may experience lasting effects or recurrence.
Understanding Bell’s Palsy is crucial, not only for those who are directly affected by it but also for the broader community to foster empathy and awareness about this temporary but impactful condition.
Causes and Risk Factors of Bell’s Palsy
Understanding the causes and risk factors is essential for those seeking to prevent or manage this condition. This article explores the potential causes of Bell’s Palsy, discusses risk factors, and offers insights into preventive measures.
Potential Causes of Bell’s Palsy
Bell’s Palsy remains somewhat of a medical mystery, with its exact cause not fully understood. However, researchers believe it is most likely due to:
1. Viral Infections: The condition is often linked to viral infections such as herpes simplex (which causes cold sores), varicella-zoster (responsible for chickenpox and shingles), Epstein-Barr (associated with mononucleosis), and others. These viruses can cause inflammation and swelling of the nerve controlling facial muscles.
2. Immune System Response: In some cases, Bell’s Palsy may result from an abnormal reaction of the body’s immune system. This autoimmune response can damage the facial nerve.
3. Nerve Compression: Inflammation or swelling in the area surrounding the facial nerve can lead to its compression, disrupting the nerve’s function and leading to the symptoms of Bell’s Palsy.
Risk Factors
Certain factors may increase the likelihood of developing Bell’s Palsy. These include:
1. Age: While it can occur at any age, Bell’s Palsy is more common among people aged 15 to 60.
2. Pregnancy: Pregnant women, especially those in the third trimester, or those who have just given birth, are at a higher risk.
3. Diabetes: Individuals with diabetes are more susceptible to developing Bell’s Palsy.
4. Respiratory Illnesses: Recent upper respiratory infections, such as the cold or flu, can elevate the risk.
5. Family History: There may be a genetic predisposition to Bell’s Palsy in some families.
Preventive Measures
While there is no guaranteed way to prevent Bell’s Palsy, the following steps might reduce risk:
1. Maintaining Overall Health: A strong immune system can fend off the infections that might trigger Bell’s Palsy. Regular exercise, a balanced diet, and adequate sleep contribute to overall health.
2. Managing Chronic Conditions: Effective management of conditions like diabetes can lower the risk.
3. Protecting Against Viral Infections: Basic hygiene practices, such as regular hand washing and avoiding close contact with people who have viral infections, can be helpful.
However, while the exact causes of Bell’s Palsy are not entirely clear, understanding the potential triggers and risk factors can help in its prevention and management. If you suspect you have symptoms of Bell’s Palsy, it is crucial to consult a healthcare professional promptly for a proper diagnosis and treatment plan.
Symptoms and Early Signs of Bell’s Palsy
Understanding its symptoms and recognizing early signs are crucial for timely treatment and recovery. This article provides a comprehensive list of symptoms associated with Bell’s Palsy, along with guidance on recognizing early signs and knowing when to seek medical help.
Comprehensive List of Symptoms
1. Rapid Onset of Weakness or Paralysis on One Side of the Face: This can happen within hours to days, making it difficult to smile, close the eye, or raise the eyebrow on the affected side.
2. Drooping of the Mouth: This might make it hard to eat or drink without spilling.
3. Decreased Ability to Close the Eye on the Affected Side: This can lead to eye dryness and irritation.
4. Altered Taste: A reduction in taste sensation on the front two-thirds of the tongue.
5. Increased Sensitivity to Sound on One Side: Sounds may seem unusually loud in one ear (hyperacusis).
6. Pain Around the Jaw or Behind the Ear: This can occur on the affected side and may precede the weakness.
7. Change in Tear and Saliva Production: Either reduced or increased.
8. Headache: This symptom is not as common but can occur.
Recognizing Early Signs
Early recognition of Bell’s Palsy is essential for prompt treatment. If you notice any of the following, consult a healthcare professional:
1. Sudden weakness or paralysis on one side of the face.
2. Difficulty with facial expressions, like smiling or closing the eye.
3. Unexplained drooping of the mouth or eyelid.
4. Changes in taste, sound sensitivity, or pain in the facial region.
When to Seek Medical Help
Immediate medical attention is recommended if:
- You experience any of the symptoms mentioned above.
- Symptoms rapidly worsen.
- You have difficulty speaking, drinking, eating, or your eye does not close properly.
- You have a high fever, rash, or severe headache accompanying the facial weakness.
Bell’s Palsy can be alarming, but early diagnosis and treatment can significantly improve the prognosis. If you suspect you or someone you know might be showing signs of Bell’s Palsy, don’t hesitate to seek medical advice.
Diagnosing Bell’s Palsy
Accurate diagnosis is critical for effective treatment. Here’s an overview of the process involved in diagnosing Bell’s Palsy, including the tests and examinations typically used.
The Diagnostic Process for Bell’s Palsy
Initial Evaluation: The diagnosis of Bell’s Palsy starts with a thorough medical history and physical examination. Doctors will ask about the onset of symptoms, their duration, and any associated factors like recent illnesses or injuries.
Physical Examination: A detailed examination of the face is crucial. Doctors look for the degree of muscle weakness, check for other facial nerve abnormalities, and assess the ability to move the forehead, close the eyes, smile, and frown.
Neurological Tests: To rule out other conditions, a neurological examination is conducted. This involves testing reflexes, muscle strength, and sensation in various parts of the body.
Tests and Examinations Specific to Bell’s Palsy
Electromyography (EMG): This test measures the electrical activity of muscles. An EMG can confirm the presence of nerve damage and determine the severity and extent of the involvement.
Imaging Tests: Sometimes, imaging tests like MRI or CT scans are used to view the facial nerve and surrounding structures. These tests help rule out other possible causes of facial paralysis, such as a tumor or stroke.
Blood Tests: While not always necessary, blood tests can help identify underlying conditions that might contribute to facial paralysis, such as diabetes or a viral infection.
Differentiating Bell’s Palsy from Other Neurological Disorders
Bell’s Palsy can be confused with other neurological disorders. Here’s how it is differentiated:
Sudden Onset: Unlike other conditions, Bell’s Palsy typically has a rapid onset of symptoms.
Facial Drooping: The hallmark of Bell’s Palsy is the one-sided facial droop that usually does not affect other parts of the body.
Absence of Other Neurological Symptoms: In Bell’s Palsy, other neurological symptoms like severe headache, arm or leg weakness, or difficulty speaking are generally absent.
Recovery Pattern: Bell’s Palsy often shows signs of improvement within weeks, which is different from more severe neurological conditions.
Ruling Out Other Causes: Tests such as MRI and blood tests help exclude conditions like stroke, Lyme disease, or brain tumors.
However, diagnosing Bell’s Palsy involves a combination of medical history, physical and neurological examinations, and specific tests. It’s crucial to differentiate it from other neurological disorders for appropriate treatment and management. Always consult a healthcare professional if you suspect Bell’s Palsy or experience sudden facial weakness.
Bell’s Palsy Treatment Options
This comprehensive guide delves into the various treatment options available, offering insights into their effectiveness and suitability.
Medications for Bell’s Palsy
One of the primary treatments for Bell’s Palsy involves medication. Commonly prescribed drugs include:
- Corticosteroids: Prednisone is often used to reduce inflammation and swelling. Its effectiveness in improving recovery rates is notable, but it’s important to be aware of potential side effects like insomnia and mood swings.
- Antiviral Medications: While the role of viruses in Bell’s Palsy is still under study, antiviral medications like Acyclovir may be prescribed alongside corticosteroids. The effectiveness of antivirals in Bell’s Palsy treatment is still a subject of research.
Physical Therapy and Exercises for Facial Muscles
Physical therapy plays a crucial role in Bell’s Palsy recovery. Key components include:
- Facial Exercises: Gentle exercises can help in regaining control over facial muscles, enhancing recovery.
- Massage and Acupuncture: These therapies might aid in muscle relaxation and improve facial nerve function.
Alternative Therapies for Bell’s Palsy
Alternative therapies have gained popularity, though their effectiveness varies:
- Acupuncture: Some patients find relief through acupuncture, though scientific backing is limited.
- Vitamin Therapy: B12, B6, and zinc supplements are sometimes recommended, but their direct impact on Bell’s Palsy recovery is not well-established.
It’s essential to consult with healthcare professionals before starting any treatment for Bell’s Palsy. They can provide personalized advice based on individual health profiles and the severity of the condition.
Home Care and Lifestyle Adjustments for Bell’s Palsy
This guide offers practical tips for managing Bell’s Palsy at home, focusing on dietary considerations and lifestyle changes to aid in recovery.
1. Nurturing a Balanced Diet
Hydration: Staying hydrated is crucial. Drink plenty of water and avoid excessive caffeine and alcohol, as they can lead to dehydration.
Nutrient-Rich Foods: Incorporate foods rich in B vitamins, Vitamin D, and Omega-3 fatty acids, which are essential for nerve health. These nutrients can be found in leafy greens, nuts, seeds, fish, and eggs.
Soft Foods: If chewing is difficult, opt for soft foods like smoothies, soups, and mashed vegetables to ensure adequate nutrition without causing strain.
2. Facial Care and Exercise
Gentle Massage: Gently massaging the affected areas of the face can improve blood flow and reduce discomfort.
Facial Exercises: Engage in facial exercises to maintain muscle tone. These should be done gently and without strain.
3. Protecting the Eye
Eye Care: If blinking is difficult, protect your eye from drying out. Use lubricating eye drops during the day and eye ointment at night. Wearing a protective eyepatch, especially while sleeping, can also be beneficial.
4. Managing Stress
Relaxation Techniques: Stress can exacerbate symptoms. Practice relaxation techniques like meditation, deep breathing, or gentle yoga.
5. Adequate Rest
Sleep and Rest: Ensure you get enough sleep and rest, as it is vital for recovery. Use extra pillows to keep your head elevated and prevent fluid accumulation in the facial area.
6. Avoiding Exposure to Cold
Stay Warm: Exposure to cold air can worsen symptoms. Keep your face protected from cold winds and consider using a scarf or face mask.
7. Consult Healthcare Professionals
Regular Check-Ups: Regularly consult with your healthcare provider to monitor your condition and adjust care as needed.
Recovering from Bell’s Palsy involves a combination of medical treatment and home care strategies. By adopting these dietary and lifestyle changes, you can support your body’s healing process and improve your overall well-being. Remember, each person’s recovery journey is unique, so it’s essential to listen to your body and consult with healthcare professionals.
The Prognosis of Bell’s Palsy: Understanding Recovery and Managing Complications
Understanding the prognosis and recovery timeline can provide reassurance and guidance for patients and their caregivers.
Typical Recovery Timelines
- Short-Term Recovery: The majority of Bell’s Palsy patients start noticing improvement within the first two weeks after symptoms begin. Most individuals experience significant recovery within three to six months.
- Long-Term Outlook: While the recovery time can vary, approximately 85% of Bell’s Palsy patients recover completely. The timeline may extend beyond six months, particularly in severe cases.
Factors Influencing Recovery
Several factors impact the recovery timeline:
- Age: Younger patients generally recover faster than older adults.
- Severity of Paralysis: Mild cases tend to resolve quicker than severe paralysis.
- Overall Health: Underlying health conditions can influence the speed and extent of recovery.
- Prompt Treatment: Early intervention with medications like corticosteroids can improve outcomes.
Potential Complications
While most individuals recover fully, some may experience complications:
- Persistent Muscle Weakness: In a small percentage of cases, some muscle weakness may remain.
- Facial Muscle Contracture: Rarely, the muscles may become permanently tightened.
- Eye Complications: Due to difficulty closing the eye, dryness or corneal damage can occur.
Mitigating Complications
Follow these steps to reduce risks:
- Protect the Eye: Use eye drops or ointments and wear a protective patch, especially at night.
- Physical Therapy: Facial exercises can help restore muscle strength and function.
- Regular Medical Follow-Up: Monitoring progress with a healthcare provider can identify and address complications early.
While Bell’s Palsy can be distressing, the prognosis is generally positive. Understanding the typical recovery timeline, factors influencing recovery, and potential complications helps in managing the condition effectively. Remember, early medical intervention and consistent care are key to a swift and complete recovery.
Advancements in Bell’s Palsy Treatment
Recent Research and Advancements in Treatment
Bell’s Palsy, a condition that causes sudden weakness in the muscles on one side of the face, has seen significant advancements in treatment options due to recent research. The past few years have been pivotal in understanding the pathology of this condition, leading to more effective and faster treatments. Here are some key highlights:
1. Improved Medication Regimens: The role of antiviral medications and corticosteroids in the treatment of Bell’s Palsy has been further clarified. Recent studies suggest that an early initiation of these drugs can significantly improve recovery rates.
2. Physical Therapy Innovations: Physical therapy remains a cornerstone in the management of Bell’s Palsy. Innovations such as targeted facial exercises and neuromuscular retraining techniques have shown promising results in enhancing facial function recovery.
3. Electrical Stimulation Therapies: The use of electrical stimulation therapies, like transcutaneous electrical nerve stimulation (TENS), has gained traction. These therapies aim to prevent muscle atrophy and promote nerve recovery.
4. Surgical Advances: For severe cases, surgical options have advanced. Procedures like decompression surgery and nerve grafting are being refined to improve outcomes for patients with severe or long-standing symptoms.
5. Holistic Approaches: There’s an increasing focus on holistic treatment approaches, including stress management and dietary modifications, which play a supportive role in recovery.
Future Outlook for Bell’s Palsy Treatment Methods
The future of Bell’s Palsy treatment is promising and geared towards personalized medicine. Ongoing research is focusing on:
1. Genetic Research: Understanding the genetic factors involved in Bell’s Palsy could lead to more tailored treatments and prevention strategies.
2. Advanced Imaging Techniques: The development of more sophisticated imaging techniques will aid in earlier and more accurate diagnosis, allowing for prompt treatment initiation.
3. Neuroprotective Drugs: Research into neuroprotective drugs holds promise for protecting nerve cells from damage and accelerating recovery.
4. Regenerative Medicine: Stem cell therapy and other regenerative medicine techniques are under investigation, potentially offering new ways to repair nerve damage.
5. AI and Machine Learning: The integration of AI and machine learning in diagnostic processes can lead to more precise treatments and better predictions of recovery outcomes.
However, the advancements in Bell’s Palsy treatment not only offer hope for more effective and faster recovery but also pave the way for innovative approaches that could revolutionize the management of this condition. As research continues to evolve, patients can look forward to more personalized and efficient treatment options.
FAQs: Understanding Bell’s Palsy
What is Bell’s Palsy?
Bell’s Palsy is a medical condition characterized by sudden, temporary weakness or paralysis of the facial muscles, typically affecting one side of the face. It can cause a drooping appearance and impact facial expressions.
What Causes Bell’s Palsy?
The exact cause of Bell’s Palsy is unknown, but it is often associated with viral infections that lead to inflammation of the facial nerve. Factors like stress, pregnancy, and diabetes may increase the risk.
Is Bell’s Palsy Permanent?
In most cases, Bell’s Palsy is not permanent. The majority of patients experience significant improvement within weeks, and complete recovery is possible within six months. However, a small percentage may have lasting effects.
Can Bell’s Palsy be Prevented?
Currently, there is no known method to prevent Bell’s Palsy. Maintaining overall health and managing risk factors, like controlling diabetes, may reduce the risk.
How is Bell’s Palsy Treated?
Treatment for Bell’s Palsy may include medications like corticosteroids to reduce inflammation and antiviral drugs if a viral infection is suspected. Physical therapy can also help restore muscle strength.
Is Bell’s Palsy Contagious?
Bell’s Palsy is not contagious. It is a neurological condition affecting the facial nerve and is not caused by an infection that can be transmitted from person to person.
Can Children Get Bell’s Palsy?
Yes, children can develop Bell’s Palsy, although it is more common in adults. Children generally have a good prognosis and recover well with appropriate treatment.
Is Bell’s Palsy a Sign of Stroke?
While Bell’s Palsy symptoms may resemble a stroke, they are not the same. Bell’s Palsy specifically affects facial muscles, while a stroke can have more widespread effects on the body and may include other symptoms like severe headache, trouble walking, or weakness in the arms or legs.
Conclusion
It’s crucial to recognize that while information about Bell’s palsy is widely available, it cannot replace the expertise of healthcare professionals. If you suspect you or someone you know might be experiencing symptoms of Bell’s palsy, it’s essential to seek medical advice promptly. Early diagnosis and treatment can significantly impact the effectiveness of the treatment and speed of recovery.
Remember, your health is paramount. Consulting with a medical professional ensures you receive personalized advice and treatment tailored to your specific needs. They can provide guidance, support, and, if necessary, treatment plans to assist in a smoother and quicker recovery. Your journey towards health and wellness is a priority, and professional medical advice is a critical step in navigating conditions like Bell’s palsy.