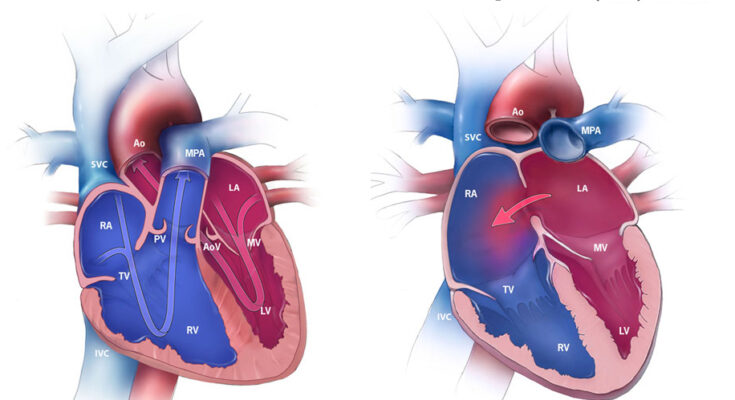
Atrial Septal Defect Treatment: Atrial Septal Defect (ASD) is a congenital heart defect characterized by a hole in the septum, the wall dividing the upper chambers of the heart.
This condition allows oxygen-rich blood from the left atrium to mix with oxygen-poor blood in the right atrium, causing an imbalance in blood flow.
What is Atrial Septal Defect (ASD)
Atrial Septal Defect (ASD) is a congenital heart condition characterized by a hole in the wall (septum) that separates the two upper chambers (atria) of the heart. This opening allows oxygen-rich blood from the left atrium to mix with oxygen-poor blood in the right atrium. Normally, the heart’s left and right sides have separate blood flow. The presence of an ASD disrupts this flow, causing various health challenges.
Common Causes and Risk Factors
The exact cause of ASD is often unclear, but it’s generally thought to result from a combination of genetic and environmental factors. Risk factors include:
- Genetic Conditions: Some chromosomal abnormalities, like Down syndrome, are linked to a higher risk of ASD.
- Family History: A family history of heart defects or ASD specifically increases the risk.
- Exposure During Pregnancy: Certain conditions during pregnancy, such as drug use, alcohol consumption, and certain medications, can increase the risk of a baby developing ASD.
Prevalence and Demographics Affected
ASD is one of the more common congenital heart defects. It affects people of all ages but is often diagnosed in childhood or early adulthood. The prevalence is slightly higher in females compared to males. While ASD can occur in any ethnic group, genetic predispositions in some populations may influence the incidence rate.
Symptoms and Early Detection of Atrial Septal Defect (ASD)
Recognizing the symptoms early is crucial for effective management. Common symptoms include:
- Shortness of Breath: Especially during exercise or physical activities.
- Fatigue: A general feeling of tiredness and lack of energy.
- Swelling of Legs, Feet, or Abdomen: Due to fluid retention.
- Heart Palpitations: Irregular heartbeats that are noticeable.
- Frequent Respiratory Infections: Especially in children.
- Difficulty in Breathing: Notable in infants during feeding.
The Importance of Early Detection
Detecting ASD early plays a vital role in preventing complications such as heart failure, pulmonary hypertension, and atrial fibrillation. Early detection allows for timely intervention, which can significantly improve the quality of life and reduce the risk of long-term heart problems.
Screening Procedures and Recommended Age for Screening
Screening for ASD is an essential step in early diagnosis and treatment. The recommended procedures include:
- Echocardiogram: A non-invasive test that uses sound waves to create a detailed image of the heart. It’s the most effective way to diagnose ASD.
- Chest X-Ray: To check the size and shape of the heart and lungs.
- Electrocardiogram (ECG or EKG): To measure the electrical activity of the heart and identify any irregularities.
Recommended Age for Screening:
- Infants and Young Children: Pediatricians often detect heart murmurs during routine check-ups, prompting further investigation.
- Adults: Screening is advised if symptoms like shortness of breath or palpitations are present, especially if there’s a family history of ASD.
By understanding the symptoms and importance of early detection, individuals can seek appropriate medical attention promptly. Regular check-ups and awareness are key in managing ASD effectively.
Diagnostic Procedures for Atrial Septal Defect (ASD)
Accurate diagnosis is crucial for effective management and treatment. This section outlines the essential diagnostic procedures for ASD, emphasizing the significance of various tests, the role of medical history and physical examination, and the interpretation of diagnostic results.
Detailed Explanation of Diagnostic Tests
- Echocardiogram: This is the primary diagnostic test for ASD. It uses sound waves to produce images of the heart, allowing doctors to see the hole in the septum and assess its size and impact on heart function.
- Electrocardiogram (ECG): An ECG records the electrical activity of the heart. It helps in identifying rhythm abnormalities that can be associated with ASD.
- Chest X-ray: This imaging test provides pictures of the heart and lungs, which can show changes in the heart’s shape and size due to ASD.
- Cardiac MRI: A more detailed imaging test, MRI provides high-resolution images of the heart’s structure and function.
- Cardiac Catheterization: In some cases, this invasive test is used to measure the pressure in the heart’s chambers and determine the blood flow pattern.
The Role of Medical History and Physical Examination
The medical history and physical examination are foundational components of ASD diagnosis. During the medical history, doctors inquire about symptoms, family history of heart diseases, and other health issues. In the physical examination, the doctor looks for signs like a heart murmur or other abnormal heart sounds that might indicate ASD.
Interpretation of Diagnostic Results
Interpreting the results of these tests requires expertise. The size and location of the ASD, its effect on heart function, and the presence of any associated heart conditions are crucial factors. The interpretation guides the treatment plan, which may range from monitoring to surgical intervention, depending on the severity of the condition.
Early and accurate diagnosis of ASD is vital for managing the condition effectively. These diagnostic procedures, combined with a thorough medical history and physical examination, provide a comprehensive approach to identifying and treating atrial septal defect.
Treatment Options for Atrial Septal Defect
The treatment for Atrial Septal Defect varies based on the size of the defect and the patient’s symptoms. Small ASDs may not require immediate treatment and can be monitored over time, while larger defects often necessitate more aggressive intervention.
Non-Surgical Treatments and Their Effectiveness
In some cases, especially when the ASD is small and not causing significant symptoms, non-surgical treatment options may be considered. These include:
- Medication: Medications don’t close the ASD but can help manage symptoms. They may include diuretics to decrease fluid buildup in the body or beta-blockers to control heart rate.
- Regular Monitoring: Regular check-ups and echocardiograms are vital to monitor the ASD’s progress and impact on the heart.
While these methods can manage symptoms, they do not close the ASD and might not be a permanent solution.
Surgical Interventions: Types and When They Are Necessary
When ASD poses a significant risk or leads to complications, surgical intervention becomes necessary. There are two main types:
- Catheter Procedures: Minimally invasive, catheter-based procedures involve inserting a thin tube through a vein into the heart and placing a device to close the ASD.
- Open-Heart Surgery: In cases where catheter procedures are not feasible, open-heart surgery is performed to stitch or patch the hole in the heart.
The choice between these methods depends on the ASD’s size, location, and the patient’s overall health.
Recent Advances in ASD Treatment
Recent advancements in ASD treatment focus on minimally invasive techniques and device improvements. Innovations in catheter-based procedures allow for quicker recovery times and reduced risks compared to traditional surgery. Research is also ongoing to develop better devices that can adapt to the heart’s movements and reduce long-term complications.
However, the treatment of Atrial Septal Defect has evolved significantly, offering patients various effective options. It’s essential for individuals with ASD to consult with a cardiologist to determine the most suitable treatment plan based on their unique condition.
Post-Treatment Care and Management of Atrial Septal Defect (ASD)
After undergoing surgery for Atrial Septal Defect (ASD), the focus of post-operative care is on recovery and prevention of complications. The key elements include:
- Rest and Gradual Activity Resumption: Patients are advised to take ample rest. Gradually, under medical guidance, they can resume daily activities.
- Pain Management: Pain relief is crucial. Medications prescribed by the healthcare provider should be taken as directed.
- Wound Care: Proper care of the surgical site to prevent infection is essential.
- Follow-up Appointments: Regular follow-up appointments are necessary to monitor the patient’s progress and address any concerns.
Long-Term Management and Lifestyle Adjustments
Long-term management of ASD involves lifestyle adjustments and medical oversight to ensure a healthy life post-surgery:
- Healthy Diet: A heart-healthy diet, low in saturated fats, cholesterol, and sodium, is recommended.
- Regular Exercise: Engaging in regular, moderate exercise, as advised by the healthcare provider, is beneficial.
- Avoiding Smoking: Smoking cessation is critical for cardiovascular health.
- Medication Adherence: If medications are prescribed, such as blood thinners, it’s important to take them as directed.
Monitoring and Regular Check-Ups
Regular monitoring is crucial for patients with ASD to prevent complications and manage the condition effectively:
- Echocardiograms: Routine echocardiograms may be recommended to monitor heart function.
- Cardiac Check-Ups: Regular visits to a cardiologist are essential to ensure the heart is functioning properly.
- Symptom Monitoring: Patients should be aware of any new or worsening symptoms and report them to their healthcare provider immediately.
However, effective post-treatment care and management of Atrial Septal Defect involve a combination of rest, lifestyle adjustments, medication adherence, and regular monitoring. These steps are vital to ensure a smooth recovery and maintain heart health in the long term.
Complications and Risks Associated with Untreated Atrial Septal Defect (ASD)
Understanding the potential complications and risks of delaying treatment is crucial for patients and healthcare providers.
Potential Complications of Untreated ASD
- Heart Failure: Over time, untreated ASD can cause the right side of the heart to enlarge and weaken, potentially leading to heart failure.
- Pulmonary Hypertension: Increased blood flow to the lungs due to the defect can result in high blood pressure in the lung arteries (pulmonary hypertension), a serious condition that can be irreversible.
- Arrhythmias: Individuals with untreated ASD are at an increased risk of developing abnormal heart rhythms (arrhythmias), particularly atrial fibrillation, which can lead to stroke or other heart-related complications.
- Stroke: The abnormal flow of blood through the heart can cause blood clots, which may travel to the brain, causing a stroke.
- Eisenmenger Syndrome: This is a rare, advanced form of pulmonary hypertension where the blood begins to flow in the reverse direction through the ASD, leading to serious complications.
Risks of Delaying Treatment
- Progression of Symptoms: Delaying treatment can lead to a progression of symptoms like fatigue, shortness of breath, and heart palpitations, affecting the quality of life.
- Increased Surgical Risks: As the condition worsens, the risks associated with potential surgery or other treatments may increase.
- Reduced Efficacy of Treatment: The effectiveness of treatments may diminish over time as the heart and lungs undergo more irreversible changes.
- Higher Long-Term Health Risks: Longer-term health risks, including chronic heart and lung conditions, are more likely if ASD is left untreated for an extended period.
However, prompt diagnosis and treatment of atrial septal defect are essential to prevent serious complications and improve long-term outcomes. Regular monitoring and early intervention can significantly reduce the risks associated with this heart condition.
Frequently Asked Questions
Q1: What is an Atrial Septal Defect (ASD)?
A1: An Atrial Septal Defect, commonly known as ASD, is a heart condition characterized by a hole in the wall (septum) that separates the two upper chambers (atria) of the heart. This hole can cause blood to flow abnormally between these chambers.
Q2: How common is ASD?
A2: ASD is a relatively common congenital heart defect. It is estimated that ASD occurs in about 1 in 1,500 live births, making it a notable condition in pediatric cardiology.
Q3: What are the symptoms of ASD?
A3: Symptoms of ASD can vary. In some cases, it may be asymptomatic, especially in children. When symptoms do occur, they can include shortness of breath, fatigue, swelling of legs, feet, or abdomen, heart palpitations, and frequent respiratory infections in children.
Q4: How is ASD diagnosed?
A4: ASD is typically diagnosed through a combination of physical examination, listening to the heart sounds, and imaging tests like echocardiograms, which use sound waves to create pictures of the heart.
Q5: What are the treatment options for ASD?
A5: Treatment for ASD depends on the size and location of the hole, as well as the patient’s age and symptoms. Options include monitoring for smaller defects, medications to manage symptoms, and surgical or catheter-based procedures to close the defect.
Q6: Is surgery always required for ASD?
A6: Not always. Small ASDs that don’t cause symptoms may only require regular monitoring. However, larger ASDs or those causing significant symptoms often require intervention, either through surgery or a less invasive catheter-based procedure.
Q7: What is the long-term outlook for someone with ASD?
A7: With proper treatment, the long-term outlook for individuals with ASD is generally very positive. Many lead normal, healthy lives post-treatment. Regular follow-up with a cardiologist is important.
Q8: Can ASD be prevented?
A8: Since ASD is a congenital condition, it cannot be prevented. However, good prenatal care and avoiding harmful substances during pregnancy can reduce the risk of congenital heart defects.
Q9: Are there any lifestyle changes recommended for someone with ASD?
A9: Individuals with ASD should consult with their healthcare provider about specific lifestyle changes. Generally, maintaining a heart-healthy lifestyle, including regular exercise and a balanced diet, is beneficial.
Q10: How does ASD affect children differently than adults?
A10: Children with ASD may experience different symptoms and complications compared to adults. Growth and developmental delays can occur, and close monitoring by a pediatric cardiologist is essential for managing their unique needs.
Conclusion
If you or someone you know exhibits symptoms like shortness of breath, fatigue, swelling of legs, or irregular heartbeats, it’s essential to consult a healthcare professional. Remember, early intervention can make a significant difference in managing ASD effectively. Healthcare providers can offer comprehensive evaluations and tailor treatments to individual needs, ensuring the best possible outcomes.
In conclusion, awareness and proactive management of Atrial Septal Defect are imperative for heart health. By understanding the importance of early detection and treatment, individuals can take essential steps towards maintaining a healthy heart. Always seek professional medical advice if you suspect ASD, as timely care can lead to better health and quality of life.