Aspergillosis Treatment: Aspergillosis is a condition triggered by Aspergillus, a common mold (a type of fungus) that lives indoors and outdoors. Most people breathe in Aspergillus spores every day without getting sick.
However, people with weakened immune systems or lung diseases are at a higher risk of developing health problems due to Aspergillus. The types of health problems caused by Aspergillus include allergic reactions, lung infections, and infections in other organs.
What is Aspergillosis?
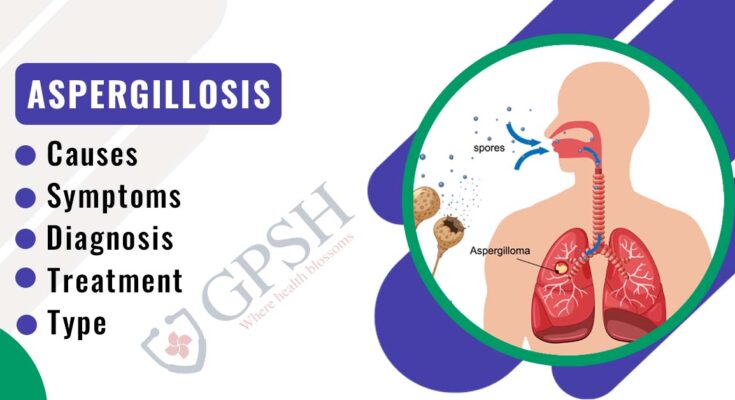
Aspergillosis is a medical condition caused by the Aspergillus fungus. This mold is commonly found in the environment, thriving in soil, decaying vegetation, and even household dust. While generally harmless to most people, it can pose significant health risks to individuals with weakened immune systems or lung diseases.
Detailed Description of Aspergillosis
Aspergillosis encompasses a range of illnesses, from mild to potentially life-threatening. It primarily affects the respiratory system, but can also impact other organs. There are several types, including:
- Allergic bronchopulmonary aspergillosis (ABPA): An allergic reaction causing inflammation in the lungs.
- Aspergilloma or “fungus ball”: A mass of fungus growing in the lungs or sinuses.
- Chronic pulmonary aspergillosis: A long-term condition affecting the lungs.
- Invasive aspergillosis: The most severe form, occurring when the infection spreads from the lungs to the bloodstream and other organs.
Causes and Risk Factors
Exposure to Aspergillus spores is the primary cause of aspergillosis. People with the following conditions are at increased risk:
- Asthma or cystic fibrosis.
- Weakened immune systems, due to conditions like HIV/AIDS, cancer treatment, or organ transplants.
- Chronic lung conditions or tuberculosis.
- Prolonged use of corticosteroids or other immunosuppressive medications.
It’s important to note that aspergillosis is not contagious and cannot be spread from person to person.
Statistics on Prevalence and Impact
The prevalence of aspergillosis varies globally, influenced by environmental factors and population health status.
- ABPA is estimated to affect about 2-15% of patients with asthma and up to 15% of patients with cystic fibrosis.
- Chronic pulmonary aspergillosis is less common, with estimates suggesting it affects 3-23 per 100,000 people annually.
- Invasive aspergillosis is a major concern in immunocompromised individuals, with a mortality rate of 30-95%, depending on the patient’s underlying condition and treatment efficacy.
Awareness and early diagnosis are crucial in managing aspergillosis, especially in high-risk groups. Regular monitoring and appropriate medical intervention can significantly reduce the health impacts of this condition.
Symptoms of Aspergillosis
Understanding these symptoms is crucial for early detection and effective treatment.
Common Symptoms of Aspergillosis
- Respiratory Issues: Persistent cough, wheezing, and shortness of breath are typical signs.
- Fever: A consistent fever that doesn’t respond well to typical fever-reducing medications can be a red flag.
- Fatigue and Weakness: General malaise and tiredness are often reported by patients.
- Weight Loss: Unexplained weight loss is a common occurrence in chronic cases.
- Chest Pain: Some patients experience chest discomfort or pain, which can be mistaken for other conditions.
Less Common Symptoms
- Coughing Up Blood: In severe cases, coughing up blood may occur, signaling advanced infection.
- Nosebleeds: Frequent and unexplained nosebleeds can be associated with certain forms of aspergillosis.
- Skin Lesions: Although rare, skin sores or lesions can develop, especially in disseminated aspergillosis.
- Vision Problems: In some instances, vision can be affected if the infection spreads to the eyes.
- Neurological Symptoms: Seizures or other neurological issues may arise in extreme cases where the infection impacts the brain.
Variations Based on Type of Aspergillosis
- Allergic Bronchopulmonary Aspergillosis (ABPA): This type primarily affects patients with asthma or cystic fibrosis, leading to worsening asthma symptoms and possible lung damage over time.
- Aspergilloma: Also known as a “fungus ball,” it typically doesn’t cause symptoms initially but may lead to chronic cough and hemoptysis (coughing up blood) as it progresses.
- Chronic Pulmonary Aspergillosis: This long-term condition often presents with weight loss, fatigue, cough, and sometimes hemoptysis.
- Invasive Aspergillosis: The most severe form, usually affects people with weakened immune systems. Symptoms can be widespread, affecting the lungs, brain, and other organs.
However, recognizing the symptoms of aspergillosis early is key to managing and treating the condition effectively. While some symptoms are common across different types, others are specific to the form of aspergillosis. If you experience any persistent or severe symptoms, consulting a healthcare professional is imperative for accurate diagnosis and appropriate treatment.
Types of Aspergillosis: Diagnosis and Treatment Implications
Understanding these types is crucial for effective healthcare management.
Allergic Bronchopulmonary Aspergillosis (ABPA):
This allergic reaction to the Aspergillus fungus primarily affects individuals with asthma or cystic fibrosis. Diagnosis involves a combination of clinical assessment, imaging, and specific IgE testing. Treatment typically includes corticosteroids and antifungal medications. Early and accurate diagnosis is vital to prevent complications such as bronchiectasis.
Chronic Pulmonary Aspergillosis (CPA):
CPA often develops in people with pre-existing lung conditions. It’s characterized by long-term respiratory symptoms and lung cavities. Diagnosis relies on a combination of chest imaging and serological tests. Antifungal therapy is the cornerstone of CPA treatment, often requiring prolonged administration to prevent recurrence.
Aspergilloma (Fungal Ball):
This form of aspergillosis involves a fungus ball developing in pre-existing lung cavities. Diagnosis is usually made using imaging techniques like CT scans, which reveal a characteristic appearance. Treatment may include surgical removal of the aspergilloma, especially in symptomatic patients, alongside antifungal therapy.
Invasive Aspergillosis (IA):
IA is a severe form that occurs mainly in immunocompromised individuals, such as transplant recipients or cancer patients. Prompt and accurate diagnosis, typically involving tissue biopsies and culture, is crucial due to its rapid progression and high mortality rate. Treatment involves aggressive antifungal therapy and, in some cases, surgical debridement of infected areas.
Cutaneous Aspergillosis:
This rare type occurs when Aspergillus infects the skin, often through wounds. Diagnosis involves skin lesion examination and fungal culture. Treatment typically includes topical and systemic antifungal agents.
Each type of Aspergillosis requires a tailored approach to diagnosis and treatment, emphasizing the importance of healthcare professionals being aware of these different forms. Accurate diagnosis and appropriate treatment strategies are essential for managing Aspergillosis effectively, improving patient outcomes, and reducing the risk of complications.
Diagnosing Aspergillosis: A Comprehensive Guide
Understanding the steps and tools involved in its diagnosis is crucial for both healthcare professionals and patients.
Steps in Diagnosing Aspergillosis
- Patient History and Symptoms Evaluation: The first step is assessing the patient’s medical history and symptoms. Chronic cough, fatigue, and weight loss are common indicators, particularly in those with weakened immune systems.
- Physical Examination: A thorough physical examination, focusing on the respiratory system, is essential. This may involve checking for any abnormal lung sounds or signs of allergic reactions.
- Laboratory Tests: Blood tests can help identify markers of infection and inflammation. Elevated levels of certain antibodies may suggest exposure to Aspergillus.
Different Diagnostic Tools and Tests
- Imaging Studies: Chest X-rays or CT scans are pivotal in visualizing lung abnormalities. These images can show characteristic signs of aspergillosis, like cavities or fibrosis in the lungs.
- Microbiological Testing: Samples from the lungs, such as sputum or tissue biopsies, are examined under a microscope or cultured to detect Aspergillus. These tests can confirm the presence and type of fungus.
- Antigen and Antibody Tests: These tests look for specific antigens or antibodies related to Aspergillus in the blood, providing further evidence of infection.
- Pulmonary Function Tests: These assess lung function and can be crucial in evaluating the impact of the infection on respiratory health.
Challenges in Diagnosing Aspergillosis
- Symptom Overlap: Symptoms of aspergillosis can mimic other respiratory diseases like tuberculosis or chronic obstructive pulmonary disease (COPD), making it difficult to diagnose accurately.
- Varied Presentations: Aspergillosis can present differently in each patient, especially in those with underlying health conditions, leading to diagnostic complexities.
- Limited Access to Advanced Testing: In some regions, access to specialized tests like antigen detection or high-resolution CT scans can be limited, delaying diagnosis.
- Interpreting Test Results: Distinguishing colonization from infection can be challenging, as Aspergillus is commonly found in the environment. This necessitates careful interpretation of test results by experienced clinicians.
However, diagnosing aspergillosis requires a multifaceted approach, combining clinical assessment with a range of diagnostic tools. Awareness of the challenges involved in diagnosis can lead to more accurate and timely identification of this condition, improving patient outcomes.
Treatment Options for Aspergillosis
This article provides an in-depth look at the treatment options for aspergillosis, focusing on antifungal medications, potential surgical interventions, and the importance of lifestyle changes and supportive care.
Antifungal Medications: Your First Line of Defense
Antifungal medications are the cornerstone of aspergillosis treatment. These drugs work by inhibiting the growth of the fungus, thereby controlling the infection. The most commonly used antifungals include:
- Voriconazole: Often the first choice, it’s known for its effectiveness against a wide range of Aspergillus species.
- Itraconazole: Used in chronic or allergic forms of aspergillosis, itraconazole is effective but may have more side effects.
- Amphotericin B: Used in severe cases, this medication is potent but can have significant side effects.
The effectiveness of these medications can vary based on the type and severity of the aspergillosis. It’s crucial to follow your healthcare provider’s guidance and report any side effects.
Surgical Options: When Medication Isn’t Enough
In some cases, especially when aspergillosis leads to complications like aspergilloma (fungal ball) or severe lung damage, surgery might be necessary. Surgical intervention aims to remove the infected tissue, thereby preventing further spread of the infection. This option is typically considered when medications are ineffective or when the disease has progressed significantly.
Lifestyle Changes and Supportive Care: Enhancing Treatment Efficacy
While medications and surgery are primary treatments, lifestyle changes and supportive care play a vital role in managing aspergillosis. These may include:
- Environmental Control: Minimizing exposure to Aspergillus spores, especially in high-risk environments.
- Nutritional Support: A balanced diet can help strengthen the immune system.
- Regular Monitoring: Keeping track of symptoms and lung function, especially in chronic cases, is essential.
However, the treatment of aspergillosis involves a multi-faceted approach including antifungal medications, possible surgical interventions, and supportive lifestyle changes. Always consult a healthcare provider for a tailored treatment plan.
Emerging Treatments and Research for Aspergillosis
Latest Advancements in Aspergillosis Treatment
Aspergillosis, a fungal infection caused by Aspergillus species, poses significant challenges in treatment, especially for those with weakened immune systems. However, the landscape of its management is evolving rapidly with recent advancements.
Innovative Antifungal Agents
New antifungal agents are at the forefront of these advancements. These drugs, with improved efficacy and fewer side effects, are revolutionizing the approach to Aspergillosis treatment. They target the fungus more effectively, reducing the duration of treatment and enhancing patient outcomes.
Advanced Diagnostic Methods
Early and accurate diagnosis is crucial in managing Aspergillosis. Emerging diagnostic methods, including molecular techniques and advanced imaging, are enabling quicker detection of the infection. This not only facilitates prompt treatment but also aids in monitoring the effectiveness of therapy, thereby improving the overall management of the disease.
Ongoing Research and Future Prospects
The future of Aspergillosis treatment is promising, thanks to ongoing research and development efforts.
Focus on Personalized Medicine
Personalized medicine is a key focus area. Researchers are exploring genetic factors that influence individual responses to antifungal treatments. This could lead to more tailored therapies, maximizing effectiveness and minimizing side effects for each patient.
Vaccine Development
There is also significant interest in developing a vaccine for Aspergillosis. While this is still in the early stages, a successful vaccine could prevent the infection in high-risk individuals, such as those with compromised immune systems.
Understanding Aspergillus Biology
A deeper understanding of Aspergillus biology and its interaction with the human immune system is another area of research. Insights gained here could lead to novel therapeutic strategies, possibly involving immune system modulation to combat the infection more effectively.
Collaboration and Global Efforts
Finally, global collaboration among researchers, healthcare professionals, and pharmaceutical companies is vital. Such partnerships are enhancing the pace of research and the dissemination of knowledge, potentially leading to breakthroughs in the prevention and treatment of Aspergillosis.
Living with Aspergillosis
Living with chronic Aspergillosis requires a comprehensive management strategy. This fungal infection, affecting the respiratory system, can have varying impacts on different individuals. The key to managing Aspergillosis effectively lies in a personalized treatment plan, often involving antifungal medications. Regular consultations with healthcare providers are essential to monitor the infection’s progression and adjust treatments accordingly.
Lifestyle and Dietary Recommendations for Aspergillosis Patients
Adjusting lifestyle and diet plays a crucial role in managing Aspergillosis. Here are some tips:
- Maintain a Clean Environment: Reducing exposure to mold spores is vital. Keep your living spaces well-ventilated and free from dampness.
- Balanced Diet: Focus on a nutritious diet that boosts your immune system. Include fruits, vegetables, lean proteins, and whole grains.
- Stay Hydrated: Adequate hydration is essential for maintaining healthy respiratory functions.
- Exercise Regularly: Engage in light to moderate exercises, as recommended by your doctor, to enhance lung capacity and overall health.
- Avoid Smoking: Smoking can exacerbate respiratory conditions, so it’s crucial to avoid it.
Support Systems and Resources for Aspergillosis
Coping with chronic Aspergillosis can be challenging, but you’re not alone. Here are some support avenues:
- Patient Support Groups: Joining Aspergillosis support groups can provide emotional support and valuable information from those who understand your experience.
- Educational Resources: Websites like the Aspergillosis Patients and Carers website offer extensive information about the condition.
- Mental Health Support: Chronic illnesses can affect your mental health. Don’t hesitate to seek professional help if you’re struggling emotionally.
- Online Forums and Communities: Platforms like Reddit and HealthUnlocked offer spaces to share experiences and advice with others affected by Aspergillosis.
Living with Aspergillosis involves adapting to various lifestyle changes and understanding the importance of ongoing medical care. By following a tailored treatment plan, making smart lifestyle choices, and utilizing available support systems, individuals with Aspergillosis can lead fulfilling lives. Remember, seeking regular medical advice and connecting with a support network are key steps in managing this chronic condition effectively.
Prevention of Aspergillosis
Fortunately, there are effective strategies to reduce the risk of this infection. Emphasizing the importance of environmental controls is crucial in preventing the spread of Aspergillosis.
Tips for Reducing the Risk of Aspergillosis
- Maintain Clean Air Environments: Use air purifiers and maintain HVAC systems to filter out fungal spores from indoor air. This is especially important in areas prone to dampness or where mold growth is common.
- Avoid Exposure to Dust and Soil: Aspergillus spores are commonly found in soil and dust. Wearing masks and taking precautions when gardening, doing yard work, or during construction activities can help minimize inhalation of these spores.
- Control Humidity and Dampness: Aspergillus thrives in moist environments. Keeping indoor humidity levels below 50% and promptly addressing water leaks or damp areas can significantly reduce the risk.
- Regular Cleaning: Regularly clean and disinfect areas prone to mold growth, such as bathrooms and kitchens, using mold-inhibiting cleaners.
- Food Safety: Aspergillus can contaminate certain foods, particularly grains, nuts, and spices. Store food properly and avoid consuming items that show signs of mold.
Importance of Environmental Controls
Environmental controls play a pivotal role in preventing Aspergillosis. This includes:
- Implementing Air Quality Standards: Hospitals and healthcare facilities should adhere to strict air quality standards to protect vulnerable patients.
- Building Maintenance: Regular inspection and maintenance of buildings can prevent mold growth and accumulation of dust, which harbor Aspergillus spores.
- Education and Awareness: Raising awareness about the sources and risks of Aspergillosis can empower individuals to take proactive steps in their environments, whether at home or work.
By adhering to these guidelines and prioritizing environmental controls, the risk of Aspergillosis can be significantly reduced, safeguarding the health of individuals, especially those with existing health concerns.
Conclusion
It’s crucial to remember that while this information serves as a guide, it cannot replace the expertise of healthcare professionals. If you suspect you or someone you know may be suffering from Aspergillosis, it’s imperative to seek professional medical advice immediately. A qualified healthcare provider can offer a personalized and accurate diagnosis, followed by a tailored treatment plan.
In conclusion, understanding Aspergillosis is the first step towards effective treatment. With the right knowledge and prompt medical attention, managing and overcoming Aspergillosis becomes more achievable. Remember, when it comes to Aspergillosis treatment, early diagnosis and professional guidance are key to a successful recovery.