Aortic Valve Stenosis Treatment: Aortic valve stenosis (AVS) is a critical heart condition characterized by the narrowing of the aortic valve, impacting blood flow from the heart to the rest of the body.
This article offers a comprehensive guide to understanding, diagnosing, and treating AVS, providing vital information for patients and healthcare professionals alike.
Understanding Aortic Valve Stenosis
What is Aortic Valve Stenosis
Aortic valve stenosis is a condition where the aortic valve, which controls blood flow from the heart to the aorta, becomes narrowed. This narrowing restricts blood flow, forcing the heart to work harder to pump blood through the smaller opening. Over time, this added strain can lead to serious health issues, including heart failure.
Causes and Risk Factors
The primary causes of aortic valve stenosis include:
- Age-Related Changes: As people age, calcium deposits or scarring can cause the valve to stiffen and narrow.
- Congenital Heart Defects: Some individuals are born with an aortic valve that has only one or two leaflets, instead of the normal three, predisposing them to stenosis.
- Rheumatic Fever: A history of rheumatic fever can lead to valve damage later in life.
Risk factors enhancing the likelihood of developing aortic valve stenosis include:
- Advanced age
- High cholesterol
- Hypertension (high blood pressure)
- Smoking
- History of heart diseases in the family
Prevalence and Demographics Affected
Aortic valve stenosis primarily affects older adults, with a higher prevalence in those over 65 years of age. It’s estimated that approximately 1-2% of people aged 65 and above have this condition. The prevalence increases with age, and men are slightly more likely to develop it than women. Awareness of this condition is crucial, as it often progresses without noticeable symptoms until the valve becomes severely narrowed.
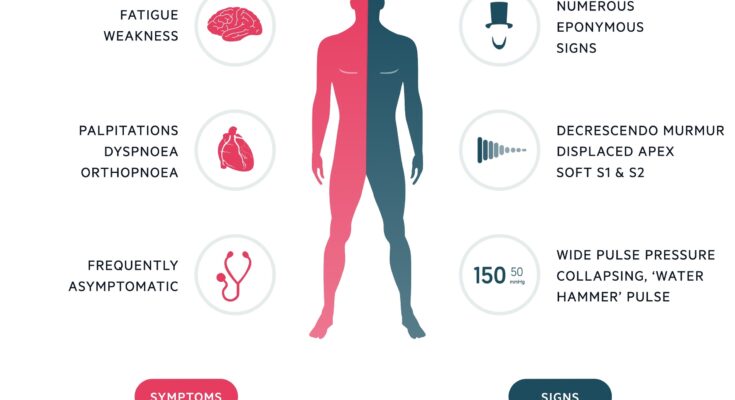
Symptoms and Early Detection of Aortic Valve Stenosis
Aortic valve stenosis, a critical heart condition, often manifests through various symptoms that should not be overlooked. Common signs include:
- Shortness of Breath: Experiencing difficulty in breathing, especially during physical activities or when lying down, is a prevalent symptom.
- Chest Pain or Pressure: This can feel like a tightness or heavy sensation in the chest area.
- Fatigue: Feeling unusually tired, even after minimal exertion, is another common sign.
- Heart Palpitations: Sensing rapid, fluttering, or pounding heartbeats.
- Fainting or Dizziness: Episodes of lightheadedness or fainting spells, particularly during or after physical activity.
- Reduced Physical Activity: Noticing a decrease in your ability to engage in physical activities that you previously could handle.
The Importance of Early Detection
Detecting aortic valve stenosis early is crucial for several reasons:
- Prevention of Heart Damage: Early detection can help prevent long-term damage to the heart and complications like heart failure.
- Better Treatment Outcomes: When diagnosed early, the treatment options are more effective and less invasive.
- Improved Quality of Life: Early management of the condition can lead to a significant improvement in the quality of life and reduce symptoms.
- Reduced Risk of Emergency Situations: Recognizing and treating the condition early reduces the risk of emergency interventions, which can be riskier.
When to Seek Medical Attention
It’s imperative to consult a healthcare professional if you notice any of the symptoms mentioned above, especially if they persist or worsen over time. Early medical intervention is key in managing aortic valve stenosis effectively. Pay particular attention to:
- Persistent or worsening symptoms.
- Symptoms that occur or worsen with physical activity.
- Any new symptoms related to your heart or breathing.
Remember, aortic valve stenosis can progress slowly and doesn’t always show symptoms until the condition is advanced. Regular check-ups and discussing any concerns with your doctor are vital steps in early detection and effective management of this condition.
Diagnostic Procedures for Aortic Valve Stenosis
Accurate diagnosis is crucial for effective treatment. Various diagnostic tests play a pivotal role in identifying and assessing the severity of this condition.
Echocardiogram: The Cornerstone of Diagnosis
The echocardiogram is a key diagnostic tool for aortic valve stenosis. It uses sound waves to create detailed images of the heart, enabling doctors to evaluate the condition of the aortic valve and measure the blood flow through the heart. This test is non-invasive, highly informative, and widely regarded as the most effective way to diagnose and monitor aortic valve stenosis.
Complementary Diagnostic Tests
While the echocardiogram is central to the diagnosis, other tests are also important:
- Electrocardiogram (EKG): This test records the electrical activity of the heart and can indicate abnormalities caused by aortic valve stenosis.
- Chest X-ray: Useful for visualizing the size and shape of the heart, a chest X-ray can show changes in the heart associated with advanced aortic valve stenosis.
- Cardiac MRI: This imaging test provides detailed pictures of the heart’s structure and function, offering additional insights, especially in complex cases.
Each of these tests contributes to a comprehensive understanding of the patient’s condition, guiding the treatment approach for aortic valve stenosis.
Treatment Options for Aortic Valve Stenosis
Treatment approaches are tailored to each patient’s specific condition, with a focus on improving heart function and alleviating symptoms.
Medications: A Supportive Role
Medications play a supportive role in managing aortic valve stenosis. They are primarily used to relieve symptoms and improve quality of life, rather than directly addressing the valve narrowing. Common medications include beta-blockers, diuretics, and blood thinners. However, their effectiveness is limited in reversing the condition, making further intervention often necessary.
Surgical Interventions: Repair and Replacement
Surgical options are a mainstay in treating severe aortic valve stenosis. There are two primary types:
- Valve Repair: In some cases, the existing valve can be repaired, preserving the patient’s native valve structure.
- Valve Replacement: More commonly, the damaged valve is replaced with a prosthetic valve. This can be done using a mechanical valve, which requires lifelong blood-thinning medication, or a biological valve, which may need to be replaced after several years.
Minimally Invasive Alternatives: TAVR
Transcatheter Aortic Valve Replacement (TAVR) has emerged as a groundbreaking, minimally invasive procedure. Ideal for patients at high risk for traditional surgery, TAVR involves placing a new valve via a catheter, usually through a small incision in the leg. This method significantly reduces recovery time and has been shown to be an effective alternative to conventional surgery.
However, the treatment of aortic valve stenosis encompasses a range of options, from medications to advanced surgical procedures. The choice of treatment depends on the severity of the condition and the patient’s overall health, with a goal to improve life quality and heart functionality. Regular monitoring and consultation with a healthcare professional are crucial in managing this condition effectively.
Post-Surgery Care and Rehabilitation for Aortic Valve Stenosis
Recovering from Aortic Valve Surgery: After undergoing surgery for aortic valve stenosis, it’s crucial to focus on recovery and rehabilitation. This phase typically involves:
- Rest and Gradual Activity: Initially, rest is key. Gradually, patients are encouraged to engage in light activities, enhancing their recovery process.
- Pain Management: Effective pain management, often through prescribed medications, is essential for a comfortable recovery.
- Wound Care: Proper care of surgical incisions prevents infections and promotes healing.
- Physical Therapy: Tailored physical therapy programs help in regaining strength and mobility.
Monitoring for Complications: Post-operative care includes vigilant monitoring for any signs of complications such as infection, abnormal heart rhythms, or heart failure symptoms.
Long-term Management and Follow-up
Regular Follow-up Appointments: Regular check-ups with a cardiologist are crucial. These appointments typically involve:
- Echocardiograms: To monitor the functioning of the replaced or repaired valve.
- Blood Pressure and Cholesterol Checks: Managing these can prevent further heart problems.
Medication Adherence: Patients may need lifelong medications like anticoagulants. Adhering to prescribed medication regimens is vital for long-term health.
Lifestyle Changes and Ongoing Monitoring
Healthy Lifestyle: Adopting a heart-healthy lifestyle can significantly impact the long-term success of aortic valve stenosis treatment. This includes:
- Balanced Diet: A diet low in saturated fats, cholesterol, and sodium, rich in fruits and vegetables.
- Regular Exercise: Engaging in regular, moderate exercise as recommended by healthcare providers.
- Smoking Cessation: Quitting smoking is crucial, as it significantly reduces heart disease risks.
Ongoing Monitoring: Continuous self-monitoring for symptoms like shortness of breath, chest pain, or fatigue is important. Any new or worsening symptoms should be reported to a healthcare provider immediately.
Advancements in Aortic Valve Stenosis Treatment
Recent Advancements in Treatment Methods
The landscape of Aortic Valve Stenosis (AVS) treatment has undergone significant transformations in recent years, driven by innovative approaches and technological advancements. These developments have revolutionized patient outcomes, offering less invasive procedures and improved quality of life. Here are some key advancements:
- Transcatheter Aortic Valve Replacement (TAVR): This minimally invasive surgical procedure has become a game-changer for patients ineligible for traditional surgery. TAVR allows for the replacement of the aortic valve through a small incision, reducing recovery time and associated risks.
- Advances in Imaging Techniques: Enhanced imaging technologies like 3D echocardiography have improved the accuracy of AVS diagnosis and treatment planning, enabling more precise interventions.
- Bioprosthetic Valve Developments: The evolution of bioprosthetic valves, which are designed to mimic natural heart valve function, has extended the durability and effectiveness of valve replacements.
- Pharmacological Improvements: There’s growing interest in medication that can complement surgical treatments of AVS, aiming to improve patient outcomes and delay disease progression.
Future Trends and Research in AVS Treatment
Looking ahead, the field of AVS treatment is ripe with potential for groundbreaking discoveries and improvements:
- Regenerative Medicine: Research into tissue engineering and regenerative medicine holds the promise of developing biologically-engineered valves that could grow with the patient, potentially eliminating the need for multiple surgeries.
- Customizable Valve Solutions: Advances in personalized medicine could lead to custom-made valves tailored to individual patient anatomy and needs, enhancing treatment effectiveness.
- AI and Machine Learning: The integration of AI and machine learning in diagnostics and treatment planning could lead to more accurate predictions of disease progression and tailor-made treatment regimens.
- Minimally Invasive Techniques: Ongoing research aims to further minimize the invasiveness of AVS treatments, reducing recovery times and improving patient comfort.
However, the future of AVS treatment is bright, with ongoing research and advancements poised to further revolutionize this field, offering hope and improved care to patients worldwide.
Patient Stories and Case Studies: Transforming Lives with Aortic Valve Stenosis Treatment
Understanding Aortic Valve Stenosis Through Real-Life Experiences
Aortic valve stenosis, a condition characterized by the narrowing of the aortic valve, significantly impacts patients’ lives. Understanding this through real-life patient stories and case studies not only brings to light the challenges faced but also highlights the profound impact of effective treatments.
Journey to Better Health: Patient Narratives
Each patient’s journey with aortic valve stenosis is unique. These narratives provide an intimate glimpse into their daily struggles and triumphs. From initial symptoms to diagnosis and treatment, their stories offer invaluable insights for others navigating similar paths.
Life-Altering Treatments: A New Lease on Life
The advancements in treating aortic valve stenosis have been life-altering for many. Patients share how medical interventions, ranging from medication to surgical procedures, have significantly improved their quality of life. These accounts serve as a testament to the progress in cardiac healthcare.
Empowering Patients and Caregivers
These stories are not just about medical outcomes; they are powerful tools for patient empowerment. They provide hope, foster a sense of community, and offer practical advice for patients and caregivers alike.
The Ripple Effect of Improved Quality of Life
The benefits of successful treatment extend beyond physical health. Patients recount how overcoming aortic valve stenosis has positively affected their mental well-being, relationships, and overall life satisfaction.
FAQs: Understanding Aortic Valve Stenosis and Its Treatment
In this section, we address frequently asked questions (FAQs) about aortic valve stenosis, a significant heart condition, and its treatment options. The information is presented in an easy-to-understand format to help readers gain a clearer understanding of this medical issue.
What is Aortic Valve Stenosis?
Aortic valve stenosis is a condition where the aortic valve, which controls blood flow from the heart to the aorta, becomes narrowed. This narrowing impedes blood flow and can lead to various health complications.
What Causes Aortic Valve Stenosis?
This condition can be caused by several factors, including congenital heart defects, calcium buildup on the valve, and rheumatic fever. Age-related changes can also lead to aortic valve stenosis in older adults.
What are the Symptoms of Aortic Valve Stenosis?
Symptoms often include shortness of breath, chest pain, fatigue, heart palpitations, and in severe cases, fainting. However, some individuals may not experience symptoms until the condition becomes advanced.
How is Aortic Valve Stenosis Diagnosed?
Doctors typically use echocardiograms, electrocardiograms (ECG), chest X-rays, and cardiac catheterization to diagnose aortic valve stenosis. These tests help evaluate the valve’s condition and the heart’s overall health.
What Treatment Options are Available?
Treatment options depend on the severity of the condition. They can range from medication management to surgical interventions like valve repair or replacement. In less severe cases, regular monitoring and lifestyle changes may be sufficient.
Can Lifestyle Changes Help with Aortic Valve Stenosis?
Yes, lifestyle changes such as maintaining a healthy weight, regular exercise, and a balanced diet can help manage symptoms and slow the progression of the disease. However, they cannot reverse the condition.
Is Surgery Always Necessary for Aortic Valve Stenosis?
Not always. Surgery is typically recommended for severe cases or when symptoms significantly impact quality of life. Less severe cases may be managed with medication and lifestyle adjustments.
What are the Risks of Aortic Valve Surgery?
Like any surgery, risks include bleeding, infection, and reactions to anesthesia. Specific to heart valve surgery, there are risks of valve dysfunction and irregular heart rhythms.
How Long is the Recovery After Valve Surgery?
Recovery time varies, but most patients spend a few days in the hospital post-surgery and may need several weeks to months for complete recovery. Cardiac rehabilitation is often recommended to aid in recovery.
Can Aortic Valve Stenosis be Prevented?
While congenital causes cannot be prevented, reducing risk factors for heart disease, like high blood pressure and cholesterol, can help prevent aortic valve stenosis caused by age-related degeneration or other heart conditions.
Conclusion
We encourage our readers to always be attentive to their health. If you notice any symptoms or changes in your body that cause concern, do not hesitate to consult a healthcare professional. Early intervention can be a pivotal factor in managing and overcoming health issues. Remember, prioritizing your health is not just a personal benefit; it also contributes positively to your family and community by fostering a culture of health awareness and proactive care.
In summary, the journey towards a healthier life begins with awareness and action. Take charge of your health by being vigilant about symptoms and seeking medical advice when necessary. Early diagnosis and effective treatment are your allies in maintaining a healthy, fulfilling life.