Patent Ductus Arteriosus Treatment: Patent Ductus Arteriosus (PDA) is a congenital heart defect that occurs when the ductus arteriosus, a blood vessel connecting the aorta to the pulmonary artery, fails to close after birth.
This condition is significant because it allows blood to bypass the lungs, leading to various physiological complications.
Typically diagnosed in newborns, PDA can result in inadequate oxygenation of blood and heart failure if not treated promptly.
What is Patent Ductus Arteriosus?
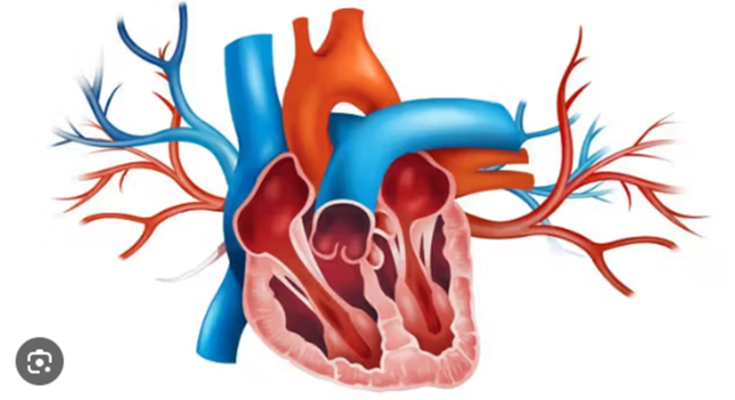
Patent Ductus Arteriosus (PDA) is a heart condition that occurs shortly after birth in some newborns. This condition involves the persistence of the ductus arteriosus, a blood vessel that normally closes soon after birth. In a healthy fetal heart, this vessel serves as a critical channel that bypasses the lungs, which are not yet in use. However, if the ductus arteriosus remains open, or “patent,” it can disrupt normal blood flow due to the differences in pressure between the heart’s chambers after birth.
How PDA Affects the Heart and Circulation
- Altered Blood Flow: The patent ductus arteriosus allows blood that should go from the left side of the heart into the body to flow back into the pulmonary circulation. This causes the heart to pump additional blood into the lungs, leading to congestion.
- Increased Heart Workload: The heart must work harder to pump the extra volume of blood. Over time, this increased workload can lead to heart enlargement and even heart failure if not treated.
- Reduced Oxygenation Efficiency: As more blood is shunted to the lungs, the efficiency of oxygen exchange can be compromised, which may reduce the oxygen available to the rest of the body.
Epidemiology: Incidence and Demographics
Patent Ductus Arteriosus is relatively common among newborns, especially in premature babies. The incidence of PDA can vary significantly but is notably higher in premature infants due to the lower likelihood of the ductus arteriosus closing spontaneously.
- Incidence: It is estimated that PDA occurs in about 1 in 2,000 full-term infants, but the rate increases to as high as 1 in 2 among very premature infants.
- Demographics: The condition is more frequently observed in female infants compared to males. Additionally, genetic factors, maternal health during pregnancy, and altitude can influence the prevalence of PDA.
However, understanding the impact of Patent Ductus Arteriosus on the heart and circulation is essential for timely intervention and management to prevent long-term complications in affected infants.
Signs and Symptoms of Patent Ductus Arteriosus
Understanding the signs and symptoms of PDA is crucial for early detection and management. Here, we explore how PDA presents in both infants and adults.
Common Symptoms in Infants and Children
In infants and young children, PDA can manifest through a variety of symptoms, which are primarily related to the heart working harder than it should. Common signs include:
- Murmuring Heart Sounds: A heart murmur, often described as a whooshing sound heard through a stethoscope, is one of the first indications of PDA.
- Rapid Breathing: Infants may exhibit faster breathing than normal, which can sometimes be accompanied by wheezing.
- Poor Feeding and Growth: Difficulty feeding or poor growth can be signs of PDA, as the heart condition may cause fatigue during feeding.
- Excessive Sweating: Infants with PDA might sweat more than usual, especially during feeding or physical activity.
- Pulmonary Congestion: Signs of congestion such as a persistent cough or respiratory infections can also be indicative of PDA.
Early diagnosis and treatment are vital to prevent complications such as heart failure and developmental issues. Pediatricians often detect these symptoms during routine check-ups.
How Symptoms Manifest Differently in Adults
While PDA is commonly identified and treated during infancy, some cases may go unnoticed until adulthood. In adults, the symptoms can be less obvious or different due to the body’s adaptation over time. Common manifestations in adults include:
- Fatigue and Breathlessness: Adults with undiagnosed PDA might experience unexplained tiredness or difficulty breathing, especially during exercise.
- Heart Palpitations: Irregular heartbeats or palpitations can be a symptom of PDA in adults, indicating altered blood flow in the heart.
- Endocarditis: Adults are at an increased risk of developing an infection of the heart lining known as endocarditis, which can exacerbate symptoms.
- Increased Risk of Heart Failure: Long-standing PDA can lead to heart failure due to the chronic overworking of the heart.
However, awareness and early intervention can greatly improve the outcome for individuals with PDA, highlighting the importance of regular health check-ups and attention to cardiovascular health.
Diagnosing Patent Ductus Arteriosus
Diagnosing this condition accurately is crucial as it influences the management and outcome of the patient. Here, we explore the various diagnostic methods and the challenges involved in diagnosing PDA.
Diagnostic Methods and Their Importance
- Echocardiogram: This is the most critical diagnostic tool for PDA. It uses sound waves to create images of the heart, allowing doctors to see the blood flow through the heart chambers and the ductus arteriosus. It helps in assessing the size of the PDA and its effect on heart function.
- Chest X-ray: X-rays can show whether there are changes in the size or shape of the heart and if there is increased lung fluid, both of which can suggest the presence of PDA.
- Electrocardiogram (ECG): While not specifically used to diagnose PDA, an ECG can show signs of heart enlargement or stress that might be related to PDA.
- Cardiac MRI: Magnetic resonance imaging provides a detailed image of the heart’s structure and blood flow. It is useful for assessing larger PDAs and planning surgical interventions.
- Cardiac Catheterization: This invasive procedure involves inserting a catheter into the heart to measure pressure and oxygen levels across different parts of the heart. It is generally reserved for complex cases or when other diagnostic methods are inconclusive.
Each of these methods plays a vital role not only in diagnosing PDA but also in determining the severity of the condition and guiding treatment decisions.
Challenges in Diagnosing PDA
- Symptom Variability: The symptoms of PDA can vary widely from none to severe, making it difficult to diagnose based on clinical symptoms alone. In premature infants, the symptoms can be subtle or masked by other prematurity-related conditions.
- Physical Examination Limitations: While a heart murmur is often present in cases of PDA, it might not be detectable in all patients, especially in those with a small PDA or in noisy clinical settings.
- Age-related Changes: The diagnostic approach may differ between newborns, older children, and adults, as the presentations and physiology change with age.
- Resource Availability: Advanced diagnostic tools like echocardiograms and MRIs may not be readily available in all healthcare settings, particularly in lower-resource environments.
- Interpretation Skills: Accurate diagnosis of PDA requires skilled interpretation of diagnostic tests, which may not be uniformly available across different regions or institutions.
However, understanding these diagnostic methods and recognizing the challenges involved are crucial steps in ensuring timely and accurate diagnosis of Patent Ductus Arteriosus, thereby improving the overall prognosis for affected individuals.
Treatment Options for Patent Ductus Arteriosus
Several effective treatments are available, ranging from non-surgical approaches to surgical interventions, and ongoing research continues to innovate in this field.
Non-Surgical Treatments
1. Medications: The first line of treatment for a PDA often involves medication that encourages the ductus arteriosus to close on its own. Commonly used drugs include:
- Indomethacin or Ibuprofen: These nonsteroidal anti-inflammatory drugs (NSAIDs) can help close the ductus arteriosus in premature infants.
- Paracetamol: A newer option that may be used when NSAIDs are contraindicated.
2. Catheter-Based Procedures: For some patients, particularly those who are at higher risk for surgery or have smaller PDAs, catheter-based procedures might be recommended. This involves inserting a catheter into a blood vessel and threading it to the heart to place a closure device. These devices effectively seal the PDA without the need for open surgery.
Surgical Treatments
1. Ligation: If medications do not close the PDA, or if the PDA is too large, surgical ligation might be necessary. This procedure involves opening the chest to access the heart and tying off the ductus arteriosus.
2. Video-Assisted Thoracoscopic Surgery (VATS): VATS is a minimally invasive surgery that uses small incisions and a camera to guide the procedure. This technique reduces recovery time and has fewer complications compared to traditional surgery.
Innovations in Treatment: Recent Advances and Research
The field of PDA treatment continues to evolve with significant advances in both techniques and technology:
1. Bioabsorbable Devices: Recent innovations include the development of devices that can be implanted to close the PDA, which then dissolve over time, reducing long-term risks associated with metal implants.
2. Gene Therapy: Researchers are exploring genetic approaches to treat or even prevent PDA before birth. Early-stage studies are promising, suggesting potential for future non-invasive treatments.
3. Customized Therapeutic Strategies: Advances in imaging and diagnostics allow for more personalized treatment plans, improving outcomes by tailoring interventions to the specific characteristics of each PDA.
However, ongoing research and innovation promise to further improve the efficacy and safety of these treatments, potentially transforming how this common congenital defect is managed in the future.
Prognosis and Management of Patent Ductus Arteriosus
Here we will discuss the expected outcomes post-treatment, the necessary long-term management and follow-up care, and potential complications to be vigilant for.
Expected Outcomes After Treatment
- Closure of the Ductus Arteriosus: The primary goal of treating PDA is to achieve the closure of the ductus arteriosus, which typically occurs naturally shortly after birth in healthy infants. Medical interventions either through medications like ibuprofen or indomethacin, or surgical procedures like catheter-based techniques or open surgery, are highly effective in closing the ductus in affected infants.
- Normalization of Hemodynamics: Successful treatment of PDA leads to the normalization of blood flow and pressure in the heart and the major blood vessels. This restores the normal circulatory pathway, which is crucial for the proper functioning of the heart and the overall health of the infant.
- Reduction in Symptoms and Improved Growth: Post-treatment, symptoms such as rapid breathing, poor feeding, and delayed growth should diminish. Infants often catch up with their peers in terms of growth and development within months following successful closure of the PDA.
Long-term Management and Follow-up Care
- Regular Cardiac Evaluations: Follow-up appointments with a pediatric cardiologist are crucial to monitor the heart’s function and to ensure that the closure remains effective. These evaluations might include physical exams, echocardiograms, and occasionally, electrocardiograms.
- Monitoring for Heart and Lung Health: Long-term management includes regular assessments of heart and lung function, especially if the PDA was closed later in infancy. This is to detect any potential lasting effects on the heart or pulmonary system.
- Developmental Assessments: Children who have had a PDA may require ongoing developmental assessments to ensure that their growth and cognitive functions are progressing normally.
Complications to Watch For
- Reopening of the Ductus Arteriosus: In some cases, the ductus arteriosus might partially or fully reopen, necessitating further treatment. Regular follow-up care helps in early detection and management of this complication.
- Residual Heart Problems: Some children may experience residual heart problems such as pulmonary hypertension or heart valve issues after a PDA closure, particularly if the closure occurred later in life or if complications arose during treatment.
- Infection Risks: Following surgical intervention, there is a small risk of infection or complications related to the procedure. Signs of infection include fever, redness or swelling at the incision site, and unusual pain or discomfort.
However, parents and caregivers should maintain ongoing communication with healthcare providers to ensure optimal care for their child.
Patient and Family Education on Patent Ductus Arteriosus (PDA)
Effective management and understanding of this condition are crucial for both patients and their families. Here’s how you can effectively educate yourself and manage PDA:
- Understanding PDA: Begin with a basic explanation of what PDA involves, including how it affects the heart’s function and the potential health implications.
- Symptom Recognition: Teach patients and families to recognize symptoms that may indicate complications or require medical attention, such as rapid breathing, poor feeding, and unusual tiredness.
- Routine Follow-ups: Stress the importance of regular follow-up appointments with pediatric cardiologists to monitor the condition and adjust treatments as needed.
- Medication Adherence: If medication is prescribed, discuss its importance, potential side effects, and the need for regular intake as directed by the healthcare provider.
- Lifestyle Adjustments: Provide guidance on any necessary lifestyle adjustments that might benefit the child’s health, such as nutritional considerations and activity levels.
- Emotional Support: Acknowledge the emotional impact of managing a chronic condition and suggest ways to seek emotional support through counseling or support groups.
Resources and Support for Families
Navigating PDA with your child can be challenging, but numerous resources and support systems are available to help:
- Educational Materials: Ask your healthcare provider for pamphlets, books, or recommended websites with reliable information about PDA.
- Support Groups: Connect with online or local support groups where experiences and advice can be shared with other families dealing with PDA.
- Specialist Referrals: Ensure you have contacts for specialists in pediatric cardiology for ongoing care and emergencies.
- Social Services: Explore social services that may offer practical support, such as transportation to medical appointments or home healthcare.
- Financial Aid: Investigate potential financial aid resources for families burdened by medical costs, such as grants from charitable foundations or government assistance programs.
- Counseling Services: Consider professional counseling or therapy to help manage the psychological and emotional strains of a chronic condition in the family.
However, educating yourself about PDA and utilizing available resources can significantly enhance your ability to manage the condition effectively while maintaining a supportive environment for your child’s development.
FAQs about Patent Ductus Arteriosus Treatment
What is Patent Ductus Arteriosus (PDA)?
Patent Ductus Arteriosus (PDA) is a heart condition that occurs when the ductus arteriosus, a blood vessel in the heart that is supposed to close shortly after birth, remains open. This can lead to increased blood flow to the lungs and may cause various health issues.
How is PDA diagnosed?
PDA is typically diagnosed through a combination of physical examinations, listening for heart murmurs via a stethoscope, and imaging tests such as echocardiography, which uses sound waves to create pictures of the heart and detect abnormal blood flow.
What are the common symptoms of PDA?
Symptoms of PDA can vary depending on the size of the ductus arteriosus and the age of the individual. Common symptoms include rapid breathing, difficulty in breathing, and frequent respiratory infections. In severe cases, it can lead to heart failure.
What treatment options are available for PDA?
Treatment for PDA depends on various factors including the age of the patient and the severity of the condition. Common treatments include:
- Medication: To help close the ductus arteriosus in premature infants.
- Catheter-based procedures: Minimally invasive procedures that close the PDA without open-heart surgery.
- Surgical closure: Recommended if other treatments are ineffective, especially in older children or adults.
Are there any risks associated with PDA treatment?
While treatments are generally safe and effective, there are potential risks such as infection, bleeding, or reactions to anesthesia. Catheter-based procedures might also carry risks of damaging the blood vessels or heart.
Can PDA close on its own without treatment?
In many infants, especially premature ones, the PDA may close on its own as the child grows. However, a persistent PDA that remains open beyond the first few weeks of life often requires medical intervention.
How can I prevent PDA?
Currently, there are no known preventative measures for PDA. It is a congenital condition, typically present at birth, and not influenced by environmental or lifestyle factors.
Conclusion
In summary, recognizing and effectively treating Patent Ductus Arteriosus (PDA) is crucial for the health and well-being of those affected, particularly in neonates and preterm infants. This congenital heart defect, if left untreated, can lead to significant health complications, including heart failure and pulmonary hypertension. Timely diagnosis and intervention are paramount in preventing these severe outcomes.
Moreover, there is a pressing need for ongoing research and innovation in the treatments available for PDA. With advances in medical technology and a deeper understanding of the condition, the potential for developing more efficient and less invasive treatment options grows. Encouraging continuous exploration in this field not only promises to improve the standard of care but also offers hope for better prognosis and quality of life for patients.
As we move forward, let us support and invest in medical research that seeks to uncover novel treatments and possibly a cure for Patent Ductus Arteriosus. Together, through sustained efforts and dedication, we can achieve significant strides in the management and treatment of this challenging condition.
References
For further reading and to validate the information provided regarding Patent Ductus Arteriosus (PDA) treatment, the following sources are highly reputable and offer detailed insights:
- American Heart Association (AHA) – Provides comprehensive information on the diagnosis and management of Patent Ductus Arteriosus. Visit their website for up-to-date research and treatment guidelines. Read more about PDA on AHA.
- Mayo Clinic – Offers an in-depth look at symptoms, causes, and treatment options for PDA, including both surgical and non-surgical approaches. This resource is invaluable for understanding the condition from a clinical perspective. Explore PDA treatment at Mayo Clinic.
- National Institutes of Health (NIH) – Features extensive research articles and clinical trial updates on PDA. It’s a great source for those looking to delve into the scientific and medical research aspects of the condition. Visit NIH for more on PDA research.
- Pediatrics & Neonatology Sources – Specializes in providing detailed pediatric care and neonatology insights, which are critical for understanding PDA in newborns. Their articles are peer-reviewed and highly informative. Learn more about neonatal PDA care.
These resources are fundamental for anyone looking to gain a comprehensive understanding of Patent Ductus Arteriosus, its implications, and the latest treatment modalities.