Patent Ductus Arteriosus Symptoms: Patent Ductus Arteriosus (PDA) is a heart condition that affects the flow of blood between two major arteries connected to the heart: the aorta and the pulmonary artery.
This condition is typically diagnosed shortly after birth and can have significant implications if not addressed timely.
In this comprehensive guide, we explore the symptoms and causes of PDA, providing essential information for caregivers and healthcare providers.
Understanding Patent Ductus Arteriosus (PDA)
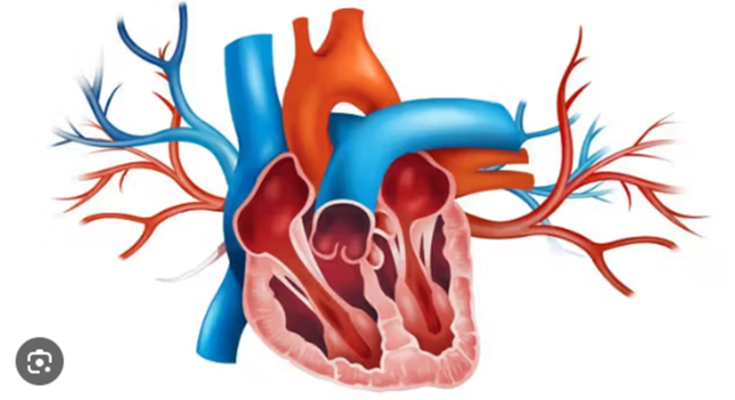
Patent Ductus Arteriosus (PDA) is a congenital heart defect that occurs when the ductus arteriosus, a blood vessel in a baby’s heart, fails to close naturally after birth. This vessel is vital during fetal development as it allows blood to bypass the lungs which are not yet in use. After birth, the ductus arteriosus is supposed to close as the newborn’s lungs take over oxygenation of the blood. When it remains open, or patent, it can lead to significant health issues, affecting the heart and circulation.
How PDA Affects the Heart and Circulation
- Increased Blood Flow to the Lungs: PDA results in abnormal blood flow between the aorta and the pulmonary artery. This causes more blood than usual to flow into the lungs. This excessive blood flow can overwork the lungs and make breathing difficult.
- Heart Overload: The heart has to work harder to pump the additional volume of blood being recirculated. Over time, this increased workload can lead to heart enlargement and even heart failure.
- Decreased Oxygenation Efficiency: As more blood circulates through the lungs, the efficiency of oxygen exchange can be reduced. This might lead to lower oxygen levels in the blood, affecting the overall oxygen supply to the body’s tissues.
- Pulmonary Hypertension: Continued high blood flow to the lungs can lead to increased pressure in the pulmonary arteries (pulmonary hypertension). This serious condition can damage the pulmonary arteries and strain the heart further.
Statistics and Demographics Affected by PDA
- Prevalence: PDA is a relatively common congenital heart defect, accounting for about 5-10% of all congenital heart diseases.
- Age and Detection: PDA is typically identified shortly after birth during neonatal screenings or upon observing symptoms like rapid breathing or poor feeding. However, in some cases, it may not be detected until later in childhood or even adulthood, especially if symptoms are mild.
- Gender Disparity: There is a noticeable gender disparity in the incidence of PDA, with the condition being more prevalent in females. Studies indicate that females are about twice as likely to be affected as males.
- Impact of Prematurity: Premature infants are particularly susceptible to PDA. Statistics show that the prevalence of PDA is significantly higher in premature babies, especially those born before 28 weeks of gestation. In some very premature infants, the incidence can be as high as 60%.
If detected early, treatments such as medications, catheter-based procedures, or surgery can be effective in closing the ductus arteriosus and minimizing the risk of long-term complications.
Symptoms of Patent Ductus Arteriosus (PDA)
Here, we will explore the common symptoms associated with PDA in infants, as well as those observed in older children and adults if the condition is not treated early. Additionally, we’ll provide tips for parents and caregivers on how to detect subtle symptoms.
Common Symptoms in Infants
In infants, the symptoms of PDA can vary from mild to severe, depending on the size of the ductus arteriosus and how much extra blood flows to the lungs. Common symptoms include:
- Frequent Respiratory Infections: Infants with PDA may experience more respiratory infections than usual due to increased fluid in the lungs.
- Rapid Breathing or Breathlessness: The extra blood flow can cause the baby to breathe rapidly or struggle for breath, especially during feeding or crying.
- Poor Feeding and Growth: Difficulty in feeding and inadequate weight gain are often observed in infants with PDA, as they may tire easily during feeding.
- Sweating Around the Head: Excessive sweating, particularly around the head during feeding or crying, can also be a sign of PDA.
- Pulsating Heartbeat: Parents might notice a stronger or more pronounced heartbeat in their infants.
Symptoms in Older Children and Adults
If PDA is not diagnosed and treated during infancy, it can persist into childhood and adulthood, leading to more severe symptoms, such as:
- Shortness of Breath: Older children and adults may experience shortness of breath, especially during exercise.
- Fatigue: There is often a noticeable increase in fatigue or tiredness, stemming from the heart’s increased workload.
- Heart Murmurs: An unusual heart sound, known as a murmur, is commonly detected by doctors during physical examinations.
- Enlarged Heart: Over time, the heart may enlarge as it works harder to pump blood.
- High Blood Pressure in the Lungs (Pulmonary Hypertension): PDA can lead to increased pressure in the lung arteries, a serious condition that might require advanced treatment.
Detecting Subtle Symptoms: Tips for Parents and Caregivers
Detecting PDA in its early stages can be challenging, especially if the symptoms are subtle. Here are some tips for parents and caregivers to help identify potential warning signs:
- Monitor Feeding Patterns: Pay attention to how your infant feeds. Difficulty in feeding, frequent breaks, sweating during feeding, or rapid fatigue are important signs.
- Observe Breathing: Note any instances of rapid or labored breathing, especially when your child is at rest or during normal activities.
- Watch for Signs of Inadequate Growth: Regularly check your child’s growth metrics. A lag in weight gain or growth compared to peers can be a crucial indicator of PDA.
- Listen to Heart Sounds: While it’s not always possible without medical training, becoming familiar with the sound of your child’s heartbeat can help you notice any unusual changes or sounds.
- Seek Regular Medical Check-Ups: Regular check-ups with a pediatrician can help catch PDA early. Mention any abnormal symptoms or behaviors you have observed.
If you notice any of these symptoms, consult with a healthcare professional for a thorough evaluation and appropriate management.
Complications Arising from Untreated Patent Ductus Arteriosus (PDA)
This condition is common in newborns, especially premature infants, but if left untreated, it can lead to a host of serious health complications both in early childhood and later in life.
Potential Complications in Infants and Young Children
- Heart Failure – The heart needs to work harder to pump blood, leading to heart failure. This can manifest as difficulty breathing, rapid heartbeat, and fatigue.
- Pulmonary Hypertension – Increased blood flow to the lungs can cause high blood pressure in the lung arteries, known as pulmonary hypertension, which can damage the lungs over time.
- Infective Endocarditis – PDA increases the risk of infection in the heart lining and valves, a condition known as infective endocarditis, which can be life-threatening if not treated promptly.
- Growth Problems – Children with untreated PDA may experience growth problems due to insufficient blood flow and oxygen delivery to the body’s tissues.
- Respiratory Issues – Frequent respiratory infections and chronic breathing difficulties can occur due to the increased workload on the lungs.
Long-term Health Implications if PDA Remains Untreated
- Cardiac Arrhythmias – Individuals with untreated PDA are at higher risk of developing irregular heart rhythms, which can complicate into more severe heart issues.
- Eisenmenger Syndrome – This is a severe form of pulmonary hypertension where the blood flow reverses from the lungs into the body, leading to cyanosis (bluish tint to the skin) and worsening heart failure.
- Congestive Heart Failure – Chronic overload of blood flow can lead to congestive heart failure, where the heart is unable to pump blood effectively, resulting in fluid buildup in the lungs, liver, and other body areas.
- Decreased Quality of Life – Ongoing health problems may lead to limitations in physical activity and overall reduced quality of life.
- Increased Risk of Premature Death – The cumulative effect of these complications can significantly shorten life expectancy if PDA is not properly managed.
Treating PDA early, typically through surgical or catheter-based interventions, can prevent these complications and lead to a healthier, more active life for those affected. Awareness and early diagnosis are crucial in managing this condition effectively.
Diagnosis of Patent Ductus Arteriosus
Timely diagnosis and intervention are crucial to prevent complications. Here’s an overview of the diagnostic methods and the importance of early detection.
Diagnostic Methods for Detecting PDA
- Echocardiogram: This is the most common and effective method for diagnosing PDA. It uses sound waves to create images of the heart, allowing doctors to see the blood flow through the heart and measure the size of the ductus arteriosus.
- Chest X-ray: This imaging technique can show whether there are changes in the heart size or problems in the lungs that might be due to PDA.
- Electrocardiogram (ECG): While an ECG primarily checks for heart rhythm irregularities, it can sometimes indicate enlarged chambers of the heart, suggesting PDA.
- Cardiac Catheterization: This invasive procedure involves inserting a thin tube into a blood vessel that leads to the heart. It provides detailed and accurate measurements of the pressure inside the heart and the oxygen levels in different parts of the heart, confirming the presence of a PDA.
- Pulse Oximetry: This non-invasive test measures the oxygen saturation in the blood. A lower than normal reading might suggest that there is a PDA, as oxygenated blood is mixing with deoxygenated blood.
Importance of Early Diagnosis and Interventions
Early diagnosis and intervention for PDA are essential for several reasons:
- Prevention of Complications: Untreated PDA can lead to complications such as infective endocarditis, pulmonary hypertension, and heart failure. Early treatment can prevent these severe health issues.
- Improved Outcomes: Early detection allows for timely medical or surgical treatment, which can improve the overall health outcomes and quality of life for affected infants.
- Minimization of Long-term Effects: Early and effective treatment of PDA can minimize the long-term effects on the heart and lungs, reducing the risk of chronic respiratory problems and cardiovascular issues in adulthood.
- Resource Management: Identifying PDA early can help in better allocation of healthcare resources, ensuring that interventions are provided when they are most effective and less invasive.
However, early intervention not only saves lives but also reduces the long-term healthcare costs associated with managing complications from untreated cases.
Treatment Options for Patent Ductus Arteriosus
Here we explore various treatment options for PDA, ranging from nonsurgical methods to surgical interventions and long-term management strategies.
Nonsurgical Methods
For many cases of PDA, especially in premature infants, nonsurgical approaches are preferred. These methods include:
- Medications: The use of nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or indomethacin is common. These medications help close the ductus arteriosus by reducing prostaglandin levels, which keep the ductus open.
- Monitoring: In some cases, especially where the PDA is small and not causing significant symptoms, careful monitoring may be all that’s required. Regular check-ups will help assess if the ductus is closing on its own.
- Catheter-Based Procedures: This minimally invasive procedure involves inserting a catheter through a large blood vessel, typically in the leg, and guiding it to the heart to place a closure device in the ductus arteriosus. This method is preferred for its quick recovery times and minimal risk compared to surgery.
Surgical Options and Advancements
Surgical treatment might be necessary if the PDA is large or causing significant health issues, or if other treatments have failed. Surgical options include:
- Ligation: A traditional method where the ductus arteriosus is tied off to prevent blood flow. This procedure requires open chest surgery.
- Video-Assisted Thoracoscopic Surgery (VATS): A less invasive form of surgery that uses small incisions and a camera to guide the surgeon. VATS leads to shorter recovery times and less pain than traditional open surgery.
- Robotic Surgery: The latest advancement in surgical technology, robotic surgery allows for even greater precision and control, potentially reducing risks and improving outcomes in PDA closure.
Long-term Management and Follow-up Care
Managing PDA over the long term, especially after surgical treatment, involves:
- Regular Cardiology Check-ups: Continuous monitoring by a cardiologist to assess heart function and ensure the PDA has not recurred.
- Medication: Some patients may require medications to help manage blood pressure, heart rate, or other associated conditions.
- Lifestyle Adjustments: Recommendations may include physical activity adjustments, dietary changes, and other health-focused lifestyle modifications to support overall cardiovascular health.
- Education and Support: Patients and families benefit from education about the condition and ongoing support from healthcare teams to manage any long-term effects of PDA.
However, with advancements in medical technology and a better understanding of the condition, patients with PDA can lead healthy, active lives.
FAQs about Patent Ductus Arteriosus Symptoms
What is Patent Ductus Arteriosus (PDA)?
Patent Ductus Arteriosus (PDA) is a heart condition that occurs when the ductus arteriosus, a blood vessel in babies’ hearts that bypasses the lungs by directing blood away from the lungs and back to the body, fails to close after birth. This is common in newborns but can lead to complications if it remains open.
What are the common symptoms of PDA in infants?
The most common symptoms of PDA in infants include rapid breathing, difficulty breathing, a continuous heart murmur, poor feeding habits, and slow weight gain. Infants with a significant PDA may show signs of tiredness and increased respiratory infections.
How is PDA detected in children?
PDA is often detected during a physical examination through the presence of a heart murmur. An echocardiogram, which uses sound waves to produce images of the heart, can confirm the diagnosis by showing how blood flows through the heart and the open ductus arteriosus.
Can older children and adults have PDA?
Yes, while PDA is most commonly identified and treated in infancy, some cases may go unnoticed until later in childhood or even adulthood. In adults, it’s often detected when investigating other heart-related symptoms or during routine medical examinations.
What complications can arise from untreated PDA?
If left untreated, PDA can lead to larger volumes of blood flowing through the heart, causing the heart to enlarge and work harder. Over time, this can lead to heart failure, increased pressure in the pulmonary arteries (pulmonary hypertension), and other serious health issues.
When should you seek medical advice for PDA?
If your child shows any signs of PDA, such as difficulty breathing, frequent respiratory infections, or unexplained poor growth, it’s important to seek medical advice. Early detection and treatment can prevent complications and improve outcomes.
Conclusion
In summary, Patent Ductus Arteriosus (PDA) is a congenital heart defect characterized by the persistence of the ductus arteriosus, a blood vessel that should close soon after birth. Common symptoms of PDA include rapid breathing, difficulty breathing, and fatigue, especially during feeding in infants. Causes are predominantly linked to genetic factors and conditions like prematurity.
If you suspect that you or your child may be exhibiting symptoms of PDA, it is crucial to seek professional medical advice. Early diagnosis and treatment can significantly improve the quality of life and prevent further complications associated with this condition. Do not hesitate to consult with a healthcare provider to ensure the best possible outcome for heart health.
References
For further reading and validation of the information provided on the symptoms of Patent Ductus Arteriosus (PDA), the following reputable sources are recommended. These links offer comprehensive insights and detailed explanations to enhance your understanding of PDA:
- Mayo Clinic – This renowned medical resource provides an in-depth overview of Patent Ductus Arteriosus, including symptoms, causes, and treatment options. Learn more about PDA at the Mayo Clinic.
- American Heart Association – A leading authority in heart-related ailments, the AHA offers valuable information on the diagnosis and management of PDA. Visit the American Heart Association to read more.
- National Institutes of Health – Through its various articles and research papers, the NIH provides scientific details and research findings related to PDA. Explore NIH resources on PDA.
These resources are essential for anyone seeking to understand the complexities of Patent Ductus Arteriosus and its impact on health. By consulting these reputable sources, you can ensure that the information you read is accurate and trustworthy.