Paraganglioma Treatment: Paraganglioma is a rare type of tumor that arises from neuroendocrine cells which are associated with the nervous system and the adrenal glands.
These tumors can occur anywhere in the body but are most commonly found near the carotid artery in the neck, along the spine, and inside the abdomen or chest.
Although paragangliomas can be benign, they have the potential to become malignant, making early diagnosis and effective treatment crucial.
Understanding Paraganglioma
Paragangliomas are rare neuroendocrine tumors that originate from the paraganglia, a group of cells that are part of the body’s autonomic nervous system. These tumors can develop in various parts of the body, including the head, neck, chest, and abdomen. Understanding the types, symptoms, and demographics affected by paragangliomas can help in early diagnosis and management.
Types of Paragangliomas
Paragangliomas are classified based on their location and whether they produce excess hormones:
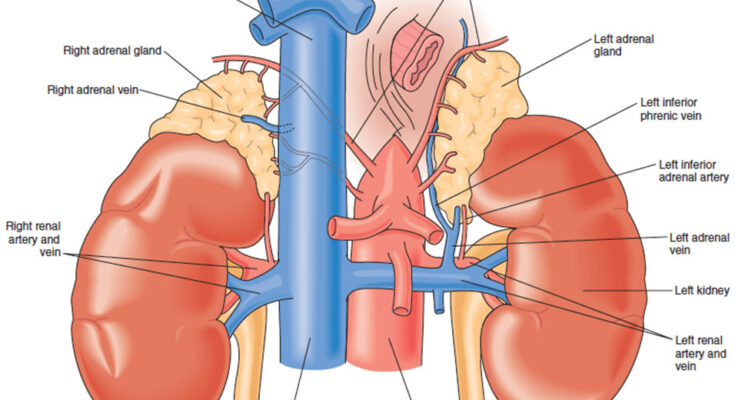
- Pheochromocytomas: These are the most common type of functional paragangliomas and arise from the adrenal glands, producing excess catecholamines.
- Head and Neck Paragangliomas: Often non-functional, these tumors develop in the paraganglia located in the head and neck region, including the carotid body, jugular bulb, and along the vagus nerve.
- Thoracic Paragangliomas: These occur in the chest area, usually along the spine or near the heart.
- Abdominal Paragangliomas: Located in the abdominal region, these can be either functional or non-functional.
Common Symptoms and Signs of Paraganglioma
The symptoms of paragangliomas vary depending on whether the tumor is functional (hormone-producing) or non-functional:
- Hypertension: Persistent or episodic high blood pressure is a common sign, especially in functional tumors.
- Heart Palpitations and Tachycardia: Rapid heartbeat can occur due to excess hormone production.
- Headaches: Often severe, these are typically linked to hormone fluctuations.
- Sweating: Excessive sweating is a frequent symptom of catecholamine-secreting tumors.
- Anxiety or Panic Attacks: These emotional responses can be triggered by hormone secretion.
- Localized Symptoms: Depending on the tumor’s location, symptoms might include a palpable mass, pain, or difficulty swallowing (particularly in head and neck paragangliomas).
Statistics on Incidence and Demographics Affected
Paragangliomas are considered very rare, with an estimated incidence of about 2 to 8 cases per million people each year. They can occur at any age but are most commonly diagnosed in adults between the ages of 30 and 50. There is no significant gender predilection, meaning both males and females are equally likely to develop these tumors. Certain genetic factors and inherited syndromes, such as Multiple Endocrine Neoplasia (MEN) types 2A and 2B, Von Hippel-Lindau disease, and Neurofibromatosis type 1, significantly increase the risk of developing paragangliomas.
Diagnosing Paraganglioma
Here’s a detailed guide on diagnosing paraganglioma, focusing on initial suspicions, key diagnostic tests, and the importance of differential diagnosis.
Initial Steps in Suspecting Paraganglioma
- Recognizing Symptoms: Common symptoms that may raise suspicion for paraganglioma include hypertension, headaches, palpitations, sweating, and anxiety. These symptoms are often episodic, corresponding with sporadic releases of catecholamines by the tumor.
- Medical History and Physical Examination: A thorough medical history and physical exam are crucial. Particular attention should be paid to past medical and family history of similar symptoms or diagnosed neuroendocrine tumors.
- Assessment of Risk Factors: Understanding any genetic predispositions or environmental exposures that could increase the likelihood of developing paraganglioma is an important initial step.
Key Diagnostic Tests
1. Biochemical Testing: The measurement of catecholamines and metanephrines in plasma and urine is a critical test. These substances are produced in excess when paragangliomas are present.
2. Imaging Tests:
- Computed Tomography (CT) and Magnetic Resonance Imaging (MRI): These imaging modalities are effective in visualizing the size, shape, and location of paragangliomas.
- 18F-fluorodeoxyglucose positron emission tomography (FDG-PET): This is used to detect paragangliomas that may not be visible on CT or MRI scans.
- Metaiodobenzylguanidine (MIBG) Scintigraphy: Particularly useful in detecting extra-adrenal paragangliomas.
3. Genetic Testing: Given the hereditary nature of some types of paragangliomas, genetic counseling and testing for mutations in specific genes like SDHB, SDHD, and SDHC are recommended.
Importance of Differential Diagnosis
- Rule Out Other Conditions: Symptoms of paraganglioma can mimic those of more common disorders like panic attacks, thyroid problems, or other forms of tumors. Accurate differential diagnosis is crucial.
- Avoid Mismanagement: Proper diagnosis ensures that the patient receives the appropriate treatment and management, avoiding the consequences of unnecessary or incorrect treatments.
- Genetic Implications: Understanding whether the paraganglioma is sporadic or hereditary influences both treatment options and surveillance strategies for patients and potentially affected family members.
However, accurate diagnosis of paraganglioma not only aids in effective treatment planning but also plays a critical role in patient counseling and management of the condition.
Treatment Options for Paraganglioma
Below, we explore the most effective treatment strategies for paraganglioma, including surgical approaches, radiation therapy, medication treatments, and emerging therapies.
Surgical Approaches for Tumor Removal
Surgery is often the first-line treatment for paraganglioma, especially if the tumor is localized and operable. The goal of surgical intervention is to completely remove the tumor while minimizing damage to surrounding tissues. The types of surgical procedures used depend on the tumor’s location:
- Adrenalectomy: Removal of one or both adrenal glands is performed if the tumor is located within these glands.
- Endoscopic Surgery: For tumors located in less accessible areas, such as the head, neck, or thorax, minimally invasive endoscopic techniques may be used.
- Laparoscopic Surgery: This is a minimally invasive procedure often employed for tumors in the abdomen, allowing for shorter recovery times and less postoperative pain.
Radiation Therapy
Radiation therapy is another cornerstone in the treatment of paraganglioma, particularly for patients who cannot undergo surgery or have metastatic disease. It involves using high-energy particles or waves, such as X-rays or gamma rays, to destroy cancer cells. The two main types of radiation therapy used in paraganglioma treatment are:
- External Beam Radiation Therapy (EBRT): Targets the tumor from outside the body and is typically used for tumors that are difficult to remove surgically.
- Stereotactic Radiosurgery: A precise form of radiation therapy that delivers concentrated radiation doses at high levels to the tumor while minimizing exposure to surrounding healthy tissues.
Medication Treatments
Medication treatments focus on controlling symptoms and limiting tumor growth, especially in cases where surgery and radiation are not viable options. Common medications include:
- Alpha-blockers and Beta-blockers: Used primarily to manage symptoms caused by excessive hormone production by the tumor.
- Chemotherapy: Although not always effective for paragangliomas, chemotherapy may be recommended for aggressive cases or when the tumor has spread.
Emerging Therapies and Clinical Trials
Research into new treatments for paraganglioma is ongoing. Emerging therapies and participation in clinical trials can provide access to cutting-edge treatments not yet widely available. Some promising areas include:
- Targeted Therapy: Drugs designed to target specific genetic changes seen in some paragangliomas.
- Immunotherapy: Treatments that help the immune system recognize and destroy cancer cells more effectively.
- Peptide Receptor Radionuclide Therapy (PRRT): A molecular therapy that delivers radioactive substances directly to tumor cells, which is particularly useful for tumors that express specific receptors.
However, consulting with a team of specialists who are experienced in treating paraganglioma is crucial to determine the most appropriate treatment strategy based on individual circumstances.
Challenges in Paraganglioma Treatment
Below, we explore the key complexities involved in the treatment of malignant paragangliomas, the management of hormonal imbalances caused by the tumors, and considerations for long-term surveillance and follow-up care.
Complexities in Treating Malignant Paragangliomas
Malignant paragangliomas are particularly challenging to treat due to their aggressive nature and tendency to metastasize. Surgical removal, the primary treatment option, is complicated by the tumor’s proximity to vital structures such as blood vessels and nerves, increasing the risk of perioperative complications. Additionally, these tumors often show resistance to conventional chemotherapy and radiation, limiting treatment options and effectiveness.
Managing Hormonal Imbalances Caused by the Tumor
Paragangliomas can secrete excess hormones, leading to significant hormonal imbalances in patients. Managing these imbalances is critical, as they can cause severe symptoms such as high blood pressure, palpitations, and panic attacks. Treatment typically involves medications to control hormone levels and symptoms, coupled with careful monitoring to adjust therapy as needed.
Long-term Surveillance and Follow-Up Care Considerations
Due to the high risk of recurrence and metastasis, long-term surveillance is essential in managing malignant paragangliomas. Regular follow-up visits and imaging tests are required to monitor for new tumor growth or spread. This ongoing surveillance helps in early detection of recurrences, which is crucial for timely intervention and improving the prognosis.
Each of these challenges underscores the need for a tailored and vigilant approach to treatment and management, ensuring the best possible outcomes for patients with malignant paragangliomas.
Living with Paraganglioma
Living with paraganglioma, a rare tumor of the nerve tissue, can be challenging but manageable with the right lifestyle adjustments and support systems. Understanding how to adapt your daily life and where to find support can significantly improve your quality of life and outcomes.
Lifestyle Adjustments and Ongoing Care
- Regular Monitoring: Schedule frequent check-ups with your healthcare provider to monitor the tumor’s behavior and manage any symptoms.
- Diet and Nutrition: Adopt a balanced diet rich in fruits, vegetables, and whole grains to help manage overall health. Consult with a nutritionist who can tailor dietary recommendations to your specific needs.
- Exercise: Engage in regular, moderate exercise to improve overall health and stamina. Exercise can also aid in managing stress and emotional well-being.
- Stress Management: Techniques such as meditation, yoga, and deep breathing can help manage the stress that often accompanies a chronic condition.
- Medication Compliance: Adhere to any prescribed medication regimens to manage symptoms effectively and prevent complications.
Support Systems and Resources for Patients
- Patient Support Groups: Join support groups where you can connect with others who understand the challenges of living with paraganglioma. These groups provide emotional support and practical advice.
- Counseling Services: Professional counselors or therapists who specialize in chronic illness can help you navigate the emotional and psychological impacts of the disease.
- Educational Resources: Utilize resources from reputable organizations like the National Cancer Institute or local hospitals for up-to-date information and educational materials about paraganglioma.
- Family and Friends: Lean on your social network for support. Family and friends can offer practical help and emotional support.
Patient Stories and Outcomes
- Survivor Testimonials: Many patients find comfort and inspiration in hearing stories from others who have faced similar challenges. Websites and support groups often feature stories highlighting personal journeys and successful management strategies.
- Outcome Statistics: Familiarize yourself with the latest research and statistics on paraganglioma outcomes. Understanding the potential prognosis and advancements in treatment can provide hope and direction.
- Advocacy and Awareness: Engage in advocacy groups and activities to help raise awareness about paraganglioma. Participating in these efforts can provide a sense of purpose and contribute to broader community support and understanding.
However, with the right strategies and supports, individuals with paraganglioma can lead fulfilling lives despite the challenges posed by the condition.
FAQs about Paraganglioma Treatment
What is Paraganglioma?
Paraganglioma is a rare type of tumor that arises from the paraganglia, a collection of nerve cells dispersed throughout the body. These tumors can develop in various parts of the body, including the head, neck, and abdomen.
What are the Symptoms of Paraganglioma?
Common symptoms include high blood pressure, headaches, sweating, rapid heartbeat, and palpitations. Some patients may also experience abdominal pain, weight loss, or anxiety.
How is Paraganglioma Diagnosed?
Diagnosis typically involves a combination of imaging studies such as MRI or CT scans, and biochemical tests to measure hormone levels in the blood or urine. A biopsy may also be performed to confirm the diagnosis.
What are the Treatment Options for Paraganglioma?
Treatment options vary depending on the tumor’s location, size, and whether it has spread. Common treatments include surgery to remove the tumor, radiation therapy, and medications to manage symptoms and reduce tumor size. In some cases, targeted therapies and chemotherapy may be recommended.
Is Surgery Always Necessary?
Surgery is often the preferred treatment to remove the tumor completely. However, for some patients, especially those with inoperable or metastatic tumors, other treatments like radiation or medication might be more appropriate.
What is the Prognosis for Paraganglioma Patients?
The prognosis depends on several factors, including the tumor’s location, size, and whether it has spread. Early detection and treatment significantly improve the chances of a favorable outcome. Regular follow-ups are crucial to monitor for recurrence or metastasis.
Can Paraganglioma Recur After Treatment?
Yes, paraganglioma can recur after treatment. Regular follow-up appointments and imaging tests are essential to detect any recurrence early and manage it promptly.
Are There Any Lifestyle Changes Recommended for Paraganglioma Patients?
Maintaining a healthy lifestyle can help manage symptoms and improve overall well-being. This includes a balanced diet, regular exercise, avoiding stress, and adhering to prescribed medications and follow-up schedules.
Where Can I Find More Information and Support?
Patients and caregivers can find more information and support from medical professionals, support groups, and organizations specializing in rare tumors and cancer care. Online resources and local health services are also valuable sources of support.
Conclusion
Recognizing symptoms and seeking a prompt diagnosis is crucial in the management of paraganglioma. Early detection can significantly improve outcomes and open the door to a wider range of treatment options.
The landscape of paraganglioma treatment is continuously evolving, with new research and therapies offering hope and improved quality of life for patients. It’s vital for patients and their families to stay informed and proactive.
Regular consultations with healthcare professionals, keeping up with the latest research, and joining support networks can empower them to make well-informed decisions about their care.
References
For additional information and to validate the details discussed in our article on Paraganglioma Treatment, the following sources are highly recommended. These resources provide comprehensive insights and further reading opportunities:
- National Cancer Institute (NCI) – Offers an extensive overview of paraganglioma, including treatment options, management strategies, and ongoing research. Visit their site for authoritative content: National Cancer Institute – Paraganglioma.
- Mayo Clinic – A leading healthcare organization that provides detailed patient-friendly information on the diagnosis and treatment of paraganglioma. Their resources are well-regarded for both accuracy and depth: Mayo Clinic – Paraganglioma.
- PubMed Central (PMC) – An invaluable database of free-to-access medical journal articles. For research articles and clinical studies on paraganglioma treatment, check out: PubMed Central.
- The Endocrine Society – Offers guidelines and the latest research findings on the management of endocrine diseases, including paraganglioma. Explore their professional articles for a deeper understanding: The Endocrine Society – Paraganglioma.
These sources are excellent for patients, medical professionals, and researchers seeking in-depth knowledge about paraganglioma and its treatment options.