Pancreatitis Symptoms: Pancreatitis is a medical condition characterized by inflammation of the pancreas. The pancreas is a vital organ located in the abdomen and plays a crucial role in digestion and metabolism.
It produces enzymes that aid in the digestion of food and hormones like insulin, which regulates blood sugar levels.
When this organ becomes inflamed, it can cause a range of symptoms and potentially severe health complications.
What is Pancreatitis?
Pancreatitis is a medical condition characterized by inflammation of the pancreas, a vital organ situated behind the stomach. The pancreas plays a crucial role in digestion and hormone production, particularly insulin, which regulates blood sugar levels. When the pancreas becomes inflamed, its functioning can be severely impaired, leading to a range of symptoms and complications.
Types of Pancreatitis
Pancreatitis manifests in two primary forms:
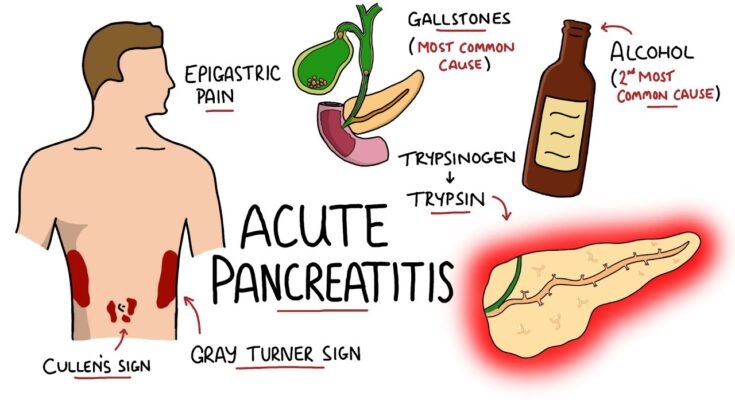
- Acute Pancreatitis: This type appears suddenly and can range from mild discomfort to life-threatening illness. It often resolves with appropriate treatment, but severe cases may cause significant damage to the pancreas.
- Chronic Pancreatitis: Unlike the acute form, chronic pancreatitis develops over many years. It leads to permanent damage and a gradual loss of pancreatic function. This form is often associated with long-term alcohol abuse, genetic disorders, or repeated episodes of acute pancreatitis.
Relevance of Pancreatitis in General Health
Pancreatitis is not just a disease of the pancreas; it can affect the entire body and contributes to various health complications. Understanding and managing pancreatitis is crucial for maintaining overall health due to the following reasons:
- Digestive Health: The pancreas produces enzymes essential for breaking down fats, proteins, and carbohydrates. Pancreatitis can lead to malnutrition and weight loss due to the reduced ability to digest and absorb nutrients.
- Diabetes: Chronic pancreatitis can impair the pancreas’s ability to produce insulin, leading to diabetes, a significant health concern globally.
- Systemic Inflammation: Severe cases of pancreatitis can trigger systemic inflammation, affecting other organs and potentially leading to multi-organ failure.
However, recognizing the signs of pancreatitis and seeking prompt medical attention can prevent the progression of the disease and reduce the risk of developing these serious health issues.
Symptoms of Pancreatitis
Pancreatitis, a condition characterized by inflammation of the pancreas, can manifest through various symptoms, which vary depending on whether the condition is acute or chronic. Recognizing these symptoms early can lead to prompt treatment and better outcomes.
Early Signs of Pancreatitis
Early detection of pancreatitis is crucial. Here are the initial signs that might indicate the onset of this condition:
- Mild to Severe Upper Abdominal Pain: This pain may radiate to the back and typically worsens after eating, especially foods high in fat.
- Abdominal Tenderness: The abdomen may be tender to the touch.
- Fever: A mild fever can accompany the early stages of pancreatitis.
- Nausea and Vomiting: These symptoms are frequently associated with the onset of pancreatitis, especially after large meals.
- Rapid Pulse: The heart rate may increase as the body reacts to the pain and inflammation.
Common Symptoms of Acute Pancreatitis
Acute pancreatitis occurs suddenly and can last for days. The common symptoms include:
- Severe Upper Abdominal Pain: This is often the most noticeable symptom.
- Swollen and Tender Abdomen: Swelling occurs due to inflammation.
- Nausea and Vomiting: Persistent and potentially severe, making it difficult to keep food down.
- Fever and Chills: These may indicate a more severe inflammation or infection.
- Increased Heart Rate: Often accompanies severe pain and dehydration.
Symptoms of Chronic Pancreatitis
Chronic pancreatitis develops over time and can lead to permanent damage if untreated. Symptoms include:
- Persistent Upper Abdominal Pain: Can be disabling and affect daily activities.
- Weight Loss and Malnutrition: Due to the pancreas not producing enough enzymes to break down food.
- Oily, Smelly Stools (Steatorrhea): Occurs if the body does not properly digest fats.
- Diabetes: As the insulin-producing cells are damaged over time.
When to See a Doctor
It’s important to consult a healthcare professional if you experience any of the above symptoms, especially severe abdominal pain. Seek immediate medical attention if:
- Pain is Severe and Unrelenting: This could indicate acute pancreatitis or other serious conditions.
- Jaundice: Yellowing of the skin or eyes could be a sign of a blocked bile duct.
- Changes in Mental State or Sudden Confusion: These could indicate a severe complication affecting your body’s chemistry or infection.
However, always prioritize professional medical advice when dealing with severe or persistent symptoms.
Causes and Risk Factors of Pancreatitis
Below, we explore the general causes of pancreatitis, along with specific risk factors for acute and chronic forms of the disease, and also delve into some less common causes.
General Causes of Pancreatitis
Pancreatitis can result from various factors, with the most prevalent causes including:
- Gallstones: These are the leading cause of acute pancreatitis. Gallstones can block the pancreatic duct, leading to inflammation.
- Alcohol consumption: Heavy alcohol use is a significant cause of both acute and chronic pancreatitis.
- Medications: Certain medications, such as some diuretics, antibiotics, and chemotherapy agents, can induce pancreatitis.
- High triglyceride levels: Elevated levels of triglycerides in the blood can lead to pancreatitis.
- Abdominal surgery or trauma: Procedures or injuries affecting the abdomen may cause pancreatitis.
- Infections: Various viral, bacterial, and fungal infections can contribute to the development of pancreatitis.
Risk Factors for Acute Pancreatitis
Acute pancreatitis occurs suddenly and usually resolves in a few days with treatment. Risk factors for developing acute pancreatitis include:
- Biliary tract disease: This is the most common cause, primarily due to gallstones.
- Alcohol misuse: Acute episodes can be triggered by excessive alcohol intake.
- Genetic predisposition: Certain genetic mutations can increase susceptibility to pancreatitis.
- Metabolic disorders: Conditions such as hypercalcemia and hyperlipidemia can precipitate acute pancreatitis.
Risk Factors for Chronic Pancreatitis
Chronic pancreatitis is a long-lasting condition that can deteriorate over time, leading to permanent damage. Risk factors for chronic pancreatitis include:
- Ongoing alcohol consumption: Chronic and excessive use is a major contributor.
- Smoking: Tobacco use significantly increases the risk of chronic pancreatitis.
- Hereditary factors: Genetic conditions like cystic fibrosis can predispose individuals to chronic pancreatitis.
- Chronic and recurrent acute pancreatitis: Repeated episodes of acute pancreatitis may evolve into chronic pancreatitis.
Less Common Causes of Pancreatitis
While the most frequent causes of pancreatitis are well-recognized, there are also less common causes that can trigger the condition:
- Autoimmune diseases: Conditions where the body’s immune system attacks its own tissues, including the pancreas.
- Pancreatic cancer: In rare cases, cancer in the pancreas can cause inflammation.
- Scorpion stings: Some species of scorpion can inject toxins that provoke pancreatitis.
- Hyperparathyroidism: Overactivity of the parathyroid glands can lead to high calcium levels, which may induce pancreatitis.
However, regular medical check-ups and lifestyle adjustments, such as moderating alcohol intake, managing diet, and avoiding smoking, can help mitigate the risk of developing this painful and potentially severe condition.
Diagnosing Pancreatitis
Accurate diagnosis is crucial for effective treatment and management. The process typically involves a combination of medical history review, physical examination, and various medical tests.
Medical History and Physical Examination
The initial steps in diagnosing pancreatitis involve a thorough medical history and physical examination. These help to identify any risk factors and symptoms consistent with the condition.
- Medical History: Doctors will ask about the patient’s past health issues, alcohol consumption, family history of pancreatitis, and any recent medications that could influence pancreatic health.
- Physical Examination: This might reveal abdominal tenderness or swelling. Physicians look for signs like jaundice (yellowing of the skin and eyes) which can indicate complications related to pancreatitis.
Imaging and Laboratory Tests
To confirm a diagnosis of pancreatitis and assess its severity, several imaging and laboratory tests are commonly employed:
- Blood Tests: Elevated levels of pancreatic enzymes, such as amylase and lipase, are indicative of pancreatitis. Blood tests can also detect signs of infection, kidney function, and other organ complications.
- Abdominal Ultrasound: This non-invasive test uses sound waves to create images of the pancreas and surrounding organs, helping to identify inflammation, blockages, or other abnormalities.
- Computed Tomography (CT) Scan: A CT scan provides a more detailed look at the pancreas, detecting inflammation, bleeding, and damage to the pancreas.
- Magnetic Resonance Imaging (MRI): MRI scans can be particularly useful in viewing bile ducts and pancreatic ducts for any obstructions or abnormalities.
- Endoscopic Ultrasound (EUS): This procedure involves an endoscope equipped with an ultrasound device. It’s inserted through the mouth and into the stomach to get close images of the pancreas, which is helpful in assessing chronic pancreatitis or investigating pancreatic cysts.
- Endoscopic Retrograde Cholangiopancreatography (ERCP): This technique uses an endoscope and X-rays to look at the pancreatic and bile ducts. It is useful for identifying stones, tumors, or narrowings that might be causing pancreatitis.
By combining findings from the patient’s medical history, physical examination, and these diagnostic tests, healthcare providers can accurately diagnose pancreatitis and tailor an appropriate treatment plan.
Complications of Pancreatitis
The nature of these complications varies depending on whether the pancreatitis is acute or chronic. Understanding these potential issues is crucial for tailoring effective treatment strategies.
Potential Complications from Acute Pancreatitis
Acute pancreatitis can result in a number of immediate, severe complications:
- Pseudocysts: Accumulations of fluid and debris in cyst-like pockets in the pancreas. These can cause persistent abdominal pain and can potentially rupture, leading to infections.
- Infection: The inflamed pancreas is more susceptible to infection, which can exacerbate the condition and lead to more severe health issues.
- Kidney Failure: Acute pancreatitis can impact kidney function, leading to acute renal failure if not managed promptly.
- Breathing Problems: The inflammation can affect the lungs, leading to breathing difficulties and, in severe cases, respiratory failure.
- Hypovolemic Shock: This is a critical condition that occurs when acute pancreatitis leads to severe fluid loss, lowering blood volume and potentially causing organ failure.
These complications necessitate immediate medical attention and often intensive care, highlighting the importance of prompt diagnosis and management.
Long-term Effects of Chronic Pancreatitis
Chronic pancreatitis, characterized by persistent inflammation of the pancreas, can lead to long-term complications such as:
- Permanent Pancreatic Damage: Over time, chronic inflammation can lead to irreversible damage and scarring of the pancreas.
- Diabetes: The pancreas plays a crucial role in insulin production. Damage from chronic pancreatitis can lead to insulin deficiency and type 1 diabetes.
- Pancreatic Cancer: Long-standing inflammation is linked with an increased risk of developing pancreatic cancer.
- Malnutrition: Chronic pancreatitis can impair the pancreas’ ability to produce enzymes necessary for digestion, leading to malabsorption and malnutrition.
- Chronic Pain: Ongoing inflammation and damage can cause persistent, debilitating abdominal pain.
These effects require long-term management strategies to mitigate symptoms and preserve as much pancreatic function as possible.
Influence of Complications on Treatment Strategies
The complications associated with pancreatitis significantly influence the approach to treatment:
- Severity and Extent of Inflammation: Treatment strategies are heavily dependent on the severity and specific nature of the complications. For instance, infections may require antibiotics, whereas pseudocysts might need surgical drainage.
- Prevention of Further Damage: In cases of chronic pancreatitis, treatment focuses on preventing further damage to the pancreas, managing pain, and supporting nutritional needs.
- Individualized Treatment Plans: Due to the variability in how pancreatitis affects individuals, treatment plans are highly personalized. They may involve a combination of medication, surgery, lifestyle changes, and nutritional management.
Overall, the approach to treating pancreatitis must be comprehensive, integrating immediate care with long-term management to minimize complications and improve quality of life.
Treatment Options for Pancreatitis
Here, we explore the various treatment strategies ranging from immediate medical interventions to long-term management and lifestyle adjustments.
Immediate Treatments for Managing Symptoms
- Pain Management: Pancreatitis often causes severe abdominal pain. Doctors may prescribe medications like acetaminophen, ibuprofen, or more potent pain relievers to manage this discomfort. In some cases, hospitalization is required for intravenous pain relief.
- Hydration: Dehydration is common in pancreatitis patients. Immediate treatment includes fluid replacement, either orally or through IV fluids, to maintain electrolyte balance and hydration.
- Fasting: To rest the pancreas and reduce its workload, patients may be advised to stop eating for a few days. Nutrition is then provided intravenously or via a feeding tube to bypass the pancreas.
- Treating Underlying Issues: Immediate treatment also focuses on addressing the root causes such as gallstones or high triglyceride levels, which might involve procedures like ERCP (Endoscopic Retrograde Cholangiopancreatography) to remove bile duct obstructions.
Long-term Treatment Strategies
- Enzyme Replacement Therapy: Chronic pancreatitis may impair the pancreas’ ability to produce digestive enzymes. Supplemental enzymes can help improve digestion and nutrient absorption, reducing diarrhea and weight loss.
- Diabetes Management: The pancreas plays a crucial role in insulin production. Damage from chronic pancreatitis may lead to diabetes, necessitating insulin therapy and regular blood sugar monitoring.
- Regular Medical Checkups: Regular follow-ups with a healthcare provider are essential to monitor the health of the pancreas, manage symptoms, and adjust treatments as needed.
- Surgery: In severe cases, surgical intervention might be necessary to remove damaged tissue, drain cysts, or relieve ductal obstructions.
Lifestyle Changes and Home Remedies
- Diet Adjustments: Adopting a low-fat, high-nutrient diet can significantly reduce symptoms. Small, frequent meals may also help manage pain and improve nutrient absorption.
- Avoid Alcohol: Alcohol can exacerbate pancreatitis symptoms and contribute to additional flare-ups. Abstaining from alcohol is crucial in both acute and chronic cases.
- Quit Smoking: Smoking is a significant risk factor for pancreatitis. Quitting smoking can reduce the risk of flare-ups and improve overall pancreatic health.
- Stress Management: Techniques like meditation, yoga, and regular exercise can help manage stress, which might otherwise exacerbate symptoms of pancreatitis.
By combining immediate medical treatments, adopting long-term management strategies, and making key lifestyle adjustments, individuals suffering from pancreatitis can lead more comfortable and healthier lives.
Prevention of Pancreatitis
Fortunately, adopting certain lifestyle changes can significantly reduce the risk of developing this condition. Here are essential tips focusing on dietary choices and the impact of alcohol consumption and smoking.
Tips to Reduce the Risk of Developing Pancreatitis
- Maintain a Balanced Diet: Emphasizing a diet rich in fruits, vegetables, whole grains, and lean proteins can help manage weight and reduce the strain on the pancreas.
- Stay Hydrated: Drinking plenty of fluids, especially water, helps keep your digestive system running smoothly and can mitigate the risk factors associated with pancreatitis.
- Limit Fatty Foods: High-fat diets can strain the pancreas, so it’s crucial to limit foods that are rich in saturated and trans fats to prevent flare-ups.
- Moderate Meal Sizes: Overeating, especially high-fat meals, can trigger pancreatitis attacks. Eating smaller, more frequent meals can help ease the workload on the pancreas.
Importance of Dietary Choices
Diet plays a pivotal role in preventing pancreatitis. Foods low in animal fats and simple sugars and high in antioxidants (like berries, leafy greens, and nuts) can protect the pancreas. Additionally, including ingredients rich in omega-3 fatty acids, such as fish and flaxseeds, can help reduce inflammation throughout the body, including the pancreas.
Role of Alcohol Consumption and Smoking in Pancreatitis
- Alcohol Consumption: Alcohol is a significant risk factor for both acute and chronic pancreatitis. Reducing alcohol intake or avoiding it altogether can drastically lower the risk of developing pancreatitis.
- Smoking: Tobacco use is strongly linked with an increased risk of developing pancreatitis. Quitting smoking not only reduces this risk but also improves overall health.
However, consulting with a healthcare provider for personalized advice tailored to your health needs is also recommended.
FAQs about Pancreatitis Symptoms
What are the most common symptoms of pancreatitis?
The most common symptoms of pancreatitis include severe upper abdominal pain that may radiate to the back, nausea, vomiting, fever, and a rapid pulse. The abdominal pain often increases after eating and can be very intense.
How quickly do symptoms of pancreatitis appear?
Symptoms of acute pancreatitis can appear suddenly and are often severe, requiring immediate medical attention. In chronic pancreatitis, symptoms may develop more gradually and persist or recur over time.
Can pancreatitis symptoms vary in intensity?
Yes, the intensity of pancreatitis symptoms can vary. In acute cases, the pain and symptoms are severe and sudden. In chronic pancreatitis, the pain may be less severe but more constant, with periods of worsening.
Are there any less common symptoms of pancreatitis?
Less common symptoms of pancreatitis can include indigestion, hiccups, clay-colored stools, and unexplained weight loss. Some people may also experience jaundice, which is a yellowing of the skin and eyes.
When should someone seek medical help for pancreatitis symptoms?
It is crucial to seek immediate medical attention if you experience severe abdominal pain, especially if accompanied by vomiting, fever, or jaundice. Early diagnosis and treatment are important to prevent complications.
Can pancreatitis be asymptomatic?
Yes, in some cases, especially in chronic pancreatitis or early stages, the disease may be asymptomatic or have very mild symptoms that can be overlooked.
How are pancreatitis symptoms diagnosed?
Diagnosis typically involves a combination of medical history evaluation, physical examinations, blood tests to check enzyme levels, and imaging tests like ultrasound, CT scan, or MRI to assess the pancreas’s condition.
Conclusion
In summary, recognizing the symptoms and understanding the causes of pancreatitis is crucial for timely and effective management of this condition. Symptoms such as severe abdominal pain, nausea, fever, and vomiting should not be ignored. Identifying whether the pancreatitis is acute or chronic is key in determining the appropriate course of treatment. It’s important to remember that factors like heavy alcohol consumption, gallstones, and certain medications can significantly contribute to the development of pancreatitis.
We strongly encourage anyone experiencing these symptoms to seek professional medical advice. Early intervention by healthcare professionals can prevent complications, improve outcomes, and ensure the well-being of individuals affected by this condition. Prioritizing your health by consulting with a doctor can lead to better management strategies and a healthier future. Remember, your health is invaluable, and timely medical attention is paramount.
References
For further reading and to validate the information provided on pancreatitis symptoms, consider exploring the following reputable sources:
- Mayo Clinic – This comprehensive guide offers detailed insights into the causes, symptoms, and treatments of pancreatitis. Read more about pancreatitis on Mayo Clinic.
- WebMD – WebMD provides a wealth of information on the signs and symptoms of pancreatitis, including diagnostic methods and lifestyle recommendations. Explore pancreatitis symptoms at WebMD.
- National Pancreas Foundation – An excellent resource for patient-focused information on pancreatitis, including educational materials and support resources. Visit the National Pancreas Foundation.
- MedlinePlus – A service of the U.S. National Library of Medicine, MedlinePlus offers reliable health information about pancreatitis, including an overview of treatment options and preventive measures. Learn more about pancreatitis on MedlinePlus.
- Healthline – Healthline provides easy-to-understand information on the symptoms, causes, and treatment options for pancreatitis, complemented by advice on living with the condition. Check out Healthline’s coverage on pancreatitis.
These sources are highly respected in the medical community and provide reliable, up-to-date information that can help readers understand and manage pancreatitis effectively.