Orchitis Symptoms: Orchitis is an inflammatory condition of the testicles that can affect males of all ages but is most commonly observed in adults.
It is characterized by swelling, pain, and a potential decrease in fertility if not addressed promptly.
Understanding the symptoms and causes of orchitis is crucial for timely diagnosis and treatment.
What is Orchitis?
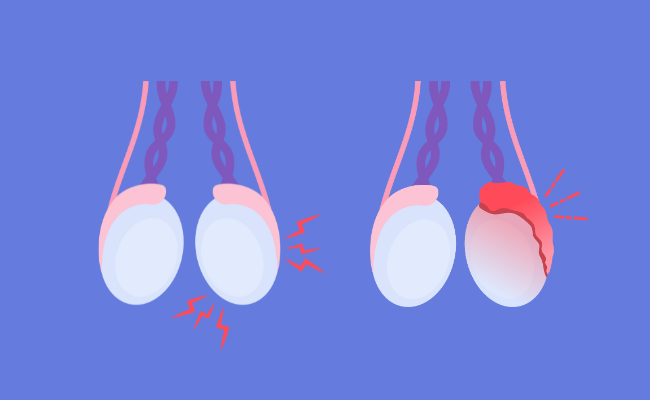
Orchitis is a medical condition characterized by the inflammation of one or both testicles in males. This inflammation can result from various causes, including infections, injuries, or underlying health conditions, and often leads to symptoms such as pain, swelling, and tenderness in the affected area. Understanding orchitis is crucial for prompt diagnosis and effective treatment.
Anatomy Involved in Orchitis
The primary anatomical structures involved in orchitis are the testicles. The testicles are oval-shaped organs contained within the scrotum, which is the skin-covered sac that hangs behind the penis. Each testicle is attached to the body by the spermatic cord, which houses blood vessels, nerves, and the vas deferens. These structures are vital for the transport of sperm and the regulation of blood flow and temperature within the testes. Orchitis typically affects these components, leading to the symptoms associated with the condition.
Types of Orchitis
Orchitis can be classified into several types based on its origin and nature:
- Viral Orchitis: Often associated with the mumps virus, this type is the most common form of orchitis. It typically develops a few days after the onset of mumps, particularly in adolescent and adult males.
- Bacterial Orchitis: This type can occur as a complication of epididymitis, where the infection spreads from the epididymis (a tube at the back of the testicles that stores and carries sperm) to the testicles. It can also be caused by sexually transmitted infections (STIs) such as gonorrhea or chlamydia.
- Granulomatous Orchitis: A less common type, granulomatous orchitis is characterized by chronic inflammation and is usually non-infectious. It may be associated with autoimmune diseases and can mimic testicular cancer in its presentation.
- Reactive Orchitis: This type can occur as a reaction to systemic infections or inflammation in other parts of the body. Unlike other forms, it is not due to a direct infection of the testicles but rather a secondary inflammatory response.
However, each type of orchitis has distinct causes, manifestations, and treatments, making it essential for individuals experiencing symptoms to seek medical evaluation to determine the specific type and appropriate management strategy.
Common Causes and Risk Factors of Orchitis
Understanding the causes and recognizing the risk factors can help in preventing the onset of this condition or managing its symptoms effectively.
Causes of Orchitis
Orchitis can be triggered by several factors, primarily involving infections and physical health conditions:
- Bacterial Infections: These are commonly associated with epididymitis, an inflammation of the tube at the back of the testicle that stores and carries sperm. When bacteria from a urinary tract or sexually transmitted infection (STI) spread to the testicles, it can lead to bacterial orchitis.
- Viral Infections: The mumps virus is a leading cause of viral orchitis, particularly affecting men who have not been vaccinated against mumps. Approximately one-third of post-pubertal males who contract mumps develop orchitis.
- Sexually Transmitted Infections (STIs): Infections such as gonorrhea and chlamydia can also cause orchitis as a complication of untreated STIs.
- Urinary Tract Infections: Though less common, UTIs can lead to orchitis if the infection spreads from the bladder or urethra to the testicles.
- Injury or Trauma: Physical injury to the groin area can cause inflammation of the testicles, which may lead to orchitis.
Risk Factors of Orchitis
Certain conditions and behaviors can increase the likelihood of developing orchitis:
- Age: Men between the ages of 15 and 35 are typically at higher risk, as this is the age group more likely to contract STIs.
- Unprotected Sexual Activity: Engaging in sexual activities without the use of condoms increases the risk of STIs, which can lead to orchitis.
- Personal History of STIs or Urinary Tract Infections: Individuals who have previously had STIs or UTIs are at increased risk of developing orchitis.
- Anatomical Issues: Conditions such as congenital urinary tract abnormalities can predispose individuals to infections that may lead to orchitis.
- Not Being Vaccinated Against Mumps: Individuals who have not received the mumps vaccine are more susceptible to mumps, which is a significant cause of viral orchitis.
However, engaging in safe sexual practices, maintaining good personal hygiene, and getting vaccinated can significantly reduce the risk of developing this painful condition.
Symptoms of Orchitis
Understanding the symptoms is crucial for timely diagnosis and treatment. Here, we explore the common symptoms of orchitis, differentiate between acute and chronic forms, and highlight signs that warrant immediate medical attention.
List of Symptoms
The primary symptoms of orchitis can include:
- Swelling of one or both testicles: This is often the most noticeable sign.
- Pain and tenderness in the testicles: The pain can range from mild to severe and may increase with movement.
- Heaviness in the scrotum: A sensation of weight or fullness in the scrotal area.
- Fever: Elevated body temperature is common, especially if the orchitis is caused by an infection.
- Nausea and vomiting: These symptoms may accompany the condition in severe cases.
- Frequent urination: An increased urge to urinate, sometimes accompanied by a burning sensation.
- Discharge from the penis: This can occur if the orchitis is associated with a bacterial infection.
How Symptoms Can Vary Between Acute and Chronic Orchitis
The symptoms of orchitis may vary depending on whether the condition is acute or chronic:
- Acute Orchitis: Symptoms appear suddenly and are typically more severe. They include intense pain, pronounced swelling, and marked tenderness in the testicles. Fever and general malaise are also more pronounced in acute cases.
- Chronic Orchitis: This form develops more slowly and symptoms are generally less severe but persistent. Chronic orchitis might manifest as a dull ache or mild discomfort in the testicles, along with occasional swelling.
Signs That Indicate You Should Seek Medical Attention
It is essential to seek medical care if you experience any of the following:
- Severe or sudden testicular pain: This could indicate a testicular torsion, a serious condition that requires immediate medical intervention.
- High fever: A fever above 38°C (100.4°F) accompanying testicular pain can be a sign of a severe infection.
- Persistent symptoms: If symptoms of discomfort, swelling, or pain persist beyond a few days, it’s important to consult a healthcare provider.
- Visible discharge or blood in urine: These are signs of a possible infection or other underlying conditions that need professional evaluation.
If you suspect you have symptoms of orchitis, consult a healthcare professional for a thorough evaluation and appropriate management.
Diagnosis of Orchitis
Diagnosing this condition accurately is crucial for effective treatment and management. The diagnostic process involves a thorough medical history, a physical examination, and specific tests and procedures.
Medical History and Physical Examination
When diagnosing orchitis, healthcare providers begin by gathering a detailed medical history and performing a physical examination:
- Medical History: The patient’s medical history includes questions about symptoms, such as pain, swelling, and fever, and their duration. Doctors also inquire about any recent infections, especially urinary tract infections or sexually transmitted infections (STIs), and a history of mumps.
- Physical Examination: The physical examination focuses on the groin area. Doctors check for swelling, tenderness, and redness of the testicles. They also assess the prostate gland and check for any discharge from the penis, which might suggest an associated infection.
Tests and Procedures
Following the initial evaluation, several tests and procedures can help confirm the diagnosis of orchitis:
- Urinalysis: This test checks for signs of infection, blood, or white blood cells in the urine.
- Blood Tests: Blood tests can detect elevated white blood cells, which indicate infection, or mumps antibodies, particularly if mumps is suspected as the cause of orchitis.
- Ultrasound: An ultrasound of the scrotum is performed to assess the structure of the testicles, rule out other conditions like torsion (twisting of the testis), and confirm inflammation.
- STD Testing: If a sexually transmitted infection is suspected, tests for gonorrhea, chlamydia, and other infections may be necessary.
- Nuclear Scan of the Testicles: This test involves injecting a small amount of radioactive material into the bloodstream. Images are then taken to observe the blood flow to the testicles, helping to differentiate between orchitis and testicular torsion.
By conducting these comprehensive evaluations, healthcare providers can accurately diagnose orchitis, leading to targeted treatment that can alleviate symptoms and prevent complications.
Complications Associated with Orchitis
Orchitis, an inflammation of one or both testicles, commonly arises from bacterial or viral infections, including mumps. If not promptly or adequately treated, orchitis can lead to several complications that may impact overall health significantly.
Potential Complications of Orchitis
- Testicular Atrophy: The affected testicle may shrink in size and lose function due to damage from prolonged inflammation.
- Scrotal Abscess: Infection may progress, leading to the formation of an abscess that could require surgical intervention.
- Chronic Epididymitis: Orchitis can lead to persistent inflammation of the epididymis, causing ongoing pain and discomfort.
- Impaired Fertility: Severe or recurrent orchitis may reduce sperm production and quality, potentially leading to difficulties in achieving conception.
- Recurrent Infections: Once affected, the testicles may become more susceptible to future infections.
- Hydrocele Formation: Fluid can accumulate around the affected testicle, leading to swelling and discomfort.
Impact of Complications on Overall Health
The complications associated with orchitis can have profound effects on a person’s health and quality of life:
- Physical Discomfort and Pain: Chronic pain and discomfort can persist long after the initial infection has resolved, affecting daily activities and mental health.
- Emotional and Psychological Stress: Concerns about fertility and chronic pain can lead to significant stress, anxiety, and depression.
- Sexual Health Problems: Issues such as decreased libido, erectile dysfunction, and discomfort during intercourse can arise, affecting relationships and self-esteem.
- Reproductive Health Concerns: Impaired fertility can impact family planning, causing distress and necessitating potentially expensive fertility treatments.
If you suspect you have orchitis, consulting with a healthcare professional promptly is advisable to prevent the onset of these complications.
Preventing Orchitis
Here, we explore effective strategies for preventing orchitis and underscore the significance of early intervention.
Recommendations for Prevention
- Vaccination: Ensure vaccinations, especially against mumps, are up to date. The MMR vaccine (measles, mumps, and rubella) is particularly crucial in preventing mumps-related orchitis.
- Maintain Good Hygiene: Regular bathing and proper hygiene can reduce the risk of bacterial infections that might lead to orchitis.
- Safe Sexual Practices: Using condoms during sexual activity helps prevent sexually transmitted infections (STIs) that could cause orchitis.
- Regular Check-Ups: Frequent medical check-ups can help catch and treat infections early before they escalate to orchitis.
- Prompt Treatment of Infections: Immediate medical attention and treatment of any urinary or reproductive tract infections can prevent their spread to the testicles.
Importance of Early Treatment in Preventing Complications
Early treatment of orchitis is crucial for several reasons:
- Prevents Severe Pain and Discomfort: Early diagnosis and management can significantly reduce the severity of symptoms.
- Avoids Testicular Damage: Timely treatment prevents potential damage to testicular tissue, which can affect fertility.
- Reduces Risk of Abscess Formation: Early intervention can prevent the development of abscesses in the testicles, which require surgical treatment.
- Decreases Likelihood of Chronic Symptoms: Proper and prompt treatment reduces the risk of developing chronic, lingering pain or discomfort in the testicles.
- Limits Spread of Infection: Early treatment helps contain the infection, preventing it from spreading to other parts of the reproductive system.
However, understanding and implementing these preventative strategies can significantly reduce the risk of orchitis and its complications. Keeping informed about symptoms and treatment options remains key to managing this condition effectively.
Treatment Options for Orchitis
Effective management of orchitis is crucial to alleviate symptoms and prevent complications. This article explores various treatment options, including medical interventions, home remedies, and surgical considerations.
Medical Treatments for Orchitis
- Antibiotics: If the orchitis is bacterial, antibiotics are the primary treatment. The specific type of antibiotic prescribed depends on the underlying bacteria. It’s crucial to complete the full course of antibiotics even if symptoms improve to ensure the infection is fully eradicated.
- Anti-inflammatory Medications: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or aspirin, can help reduce swelling and pain associated with orchitis.
- Antiviral Medication: In cases where orchitis is caused by viral infections such as mumps, antiviral medications may be prescribed, although often the treatment focuses on relief of symptoms.
- Supportive Undergarments: Wearing snug, supportive undergarments can help alleviate discomfort by supporting the scrotum and reducing swelling.
Home Remedies and Self-Care Measures
- Rest: Adequate rest is essential. Limiting physical activity can help reduce irritation and swelling in the testicles.
- Cold Compresses: Applying ice packs wrapped in a cloth to the affected area for short periods (15-20 minutes) several times a day can help reduce swelling and pain.
- Elevation: Elevating the scrotum while lying down can help reduce swelling and discomfort.
- Hydration: Staying well-hydrated is important, especially if the orchitis is associated with systemic infections like mumps.
- Avoiding Irritants: Avoid activities or clothing that may exacerbate the pain, such as tight clothing or vigorous exercise.
When to Consider Surgery
Surgery is rarely required for orchitis but may be considered in specific circumstances:
- Abscess Formation: If an abscess develops in the testicle, surgical drainage may be necessary to remove the pus and alleviate pressure.
- Chronic Epididymitis: Sometimes, orchitis can lead to chronic epididymitis, where the inflammation persists or recurs frequently. In such cases, surgical intervention may be required to remove the affected part of the epididymis.
- Testicular Atrophy or Damage: If the testicles have sustained significant damage or atrophy as a result of severe or recurrent orchitis, surgical evaluation and intervention might be considered to address complications or residual effects.
It is vital to consult with a healthcare professional for a proper diagnosis and appropriate treatment plan tailored to the specific cause and severity of orchitis. Early and effective treatment can significantly improve outcomes and comfort.
FAQs about Orchitis Symptoms
What is orchitis?
Orchitis refers to the inflammation of one or both testicles, typically caused by bacterial or viral infections. It is often associated with mumps or other infections that impact the reproductive system.
What are the common symptoms of orchitis?
The most frequent symptoms of orchitis include swelling of one or both testicles, pain ranging from mild to severe, tenderness, fever, nausea, and a feeling of heaviness in the affected testicle. Some may also experience general fatigue or flu-like symptoms.
How quickly do orchitis symptoms appear?
Symptoms of orchitis can develop suddenly, usually within a few days of infection. Viral causes like mumps may take longer to manifest symptoms, typically appearing 4 to 6 days after the onset of mumps.
Can orchitis symptoms be mistaken for something else?
Yes, symptoms of orchitis can be similar to other conditions like epididymitis (inflammation of the tube at the back of the testicle that stores and carries sperm), testicular torsion (a sudden twisting of the testicles that causes severe pain and swelling), and hernias. Accurate diagnosis by a healthcare provider is crucial.
Are there any long-term effects of orchitis?
If not treated promptly, orchitis can lead to reduced fertility, chronic pain, and atrophy (shrinking) of the affected testicle. Early treatment is essential to prevent long-term complications.
How is orchitis treated?
Treatment for orchitis depends on the underlying cause. Bacterial infections are treated with antibiotics, while viral infections are generally managed with rest, ice packs, elevation of the scrotum, and over-the-counter pain relief. In all cases, it’s important to follow the guidance of a healthcare professional.
When should someone seek medical attention for orchitis?
If you experience any symptoms of orchitis, such as testicular pain or swelling, fever, or nausea, seek medical attention promptly. Early diagnosis and treatment are key to managing symptoms and preventing complications.
Conclusion
In summary, recognizing the symptoms of orchitis is crucial for timely and effective treatment. This condition, marked by inflammation and discomfort in the testicles, can lead to serious complications if left unchecked. It is essential for individuals to be aware of the initial signs, such as swelling, pain, fever, and nausea, to prevent further health issues.
We strongly encourage anyone experiencing these symptoms to consult a healthcare provider immediately. Early medical intervention can significantly improve the outcome and prevent long-term consequences. Remember, prioritizing your health is paramount, and seeking professional advice is a key step in ensuring your well-being.
References
For further reading and to validate the information provided on orchitis symptoms, consider the following reputable sources. These links lead to comprehensive articles and research papers that offer in-depth insights into the symptoms, causes, and treatment options for orchitis:
- Centers for Disease Control and Prevention (CDC) – This page provides detailed information on the causes, symptoms, and treatment of orchitis, particularly related to mumps and other infections. CDC Orchitis Information
- Mayo Clinic – The Mayo Clinic offers a robust overview of orchitis, including diagnostic methods and management strategies, helping patients understand how to seek appropriate care. Mayo Clinic on Orchitis
- MedlinePlus – A resource by the U.S. National Library of Medicine, MedlinePlus presents trustworthy information on the symptoms and treatments for orchitis, backed by medical research. MedlinePlus Orchitis Resource
- WebMD – WebMD provides an article that covers the essential aspects of orchitis, including symptom recognition and when to consult a healthcare provider. WebMD on Orchitis
These sources are instrumental in offering accurate and medically reviewed information that can aid individuals in understanding orchitis better.