Optic Neuritis Treatment: Optic neuritis, a pivotal and alarming condition, often manifests as an inflammatory demyelination of the optic nerve, which can drastically impair vision.
This condition is frequently linked to multiple sclerosis (MS) but can arise from various other causes.
Understanding the comprehensive diagnosis and treatment approaches for optic neuritis is essential for timely intervention and optimal patient outcomes.
What is Optic Neuritis?
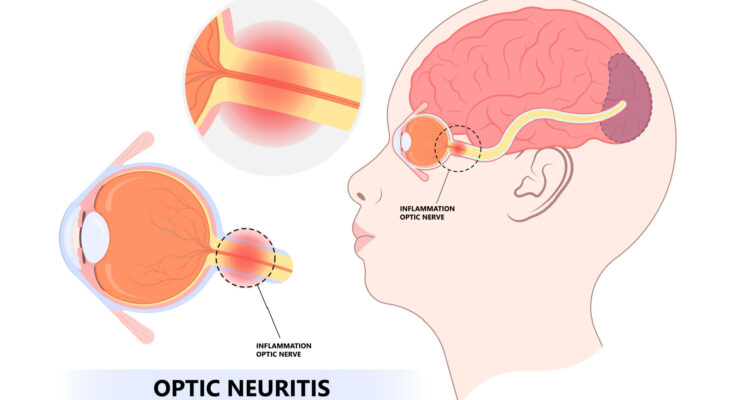
Optic neuritis is an inflammation of the optic nerve, the bundle of nerve fibers that transmits visual information from your eye to your brain. Commonly manifesting as pain in the eye and vision loss, optic neuritis can affect one or both eyes. The symptoms often come on suddenly and can vary in severity. This condition is frequently associated with autoimmune disorders, particularly multiple sclerosis (MS), where the body’s immune system mistakenly attacks the protective sheath (myelin) surrounding nerve fibers.
Statistics on Prevalence and Risk Factors
Optic neuritis is relatively uncommon, affecting approximately 5 out of 100,000 people each year. While it can occur at any age, it is most prevalent among adults aged 20 to 40 years. Women are at a higher risk compared to men, with a ratio of about 1.9:1.
Risk Factors:
- Autoimmune Diseases: Individuals with autoimmune conditions, especially multiple sclerosis, are at a significantly higher risk.
- Genetic Factors: Family history of autoimmune diseases can increase susceptibility.
- Environmental Influences: Some studies suggest that infections and certain vaccines may trigger the development of optic neuritis.
- Ethnicity: Caucasians are more likely to develop optic neuritis than other ethnic groups.
However, understanding these statistics and risk factors is crucial for early diagnosis and effective management of optic neuritis.
Symptoms of Optic Neuritis
Optic neuritis, an inflammation of the optic nerve, can manifest through various symptoms that may differ from person to person. Recognizing these symptoms early is crucial for effective treatment and management.
Common Signs and Symptoms of Optic Neuritis
- Vision Loss – One of the most alarming symptoms is sudden, usually partial, loss of vision. This typically affects one eye and can progress over hours or days.
- Pain – Movement of the affected eye often brings about pain, described as a sharp, aching sensation that can intensify with eye movement.
- Color Vision Changes – Colors may appear faded or less vivid than usual, a condition known as color desaturation.
- Visual Field Loss – Some individuals experience a reduction in their peripheral vision, which might feel like looking through a narrow tube.
- Flashing Lights – Brief, occasional flashes of light, often subtle, can occur in the vision of those affected.
Variability of Symptoms Between Individuals
The intensity and combination of symptoms can vary widely among individuals:
- Severity of Vision Loss – While some may experience mild blurriness, others might face severe vision impairment.
- Onset of Symptoms – The speed at which symptoms develop can vary; some experience rapid onset, while for others, it might progress more slowly.
- Recovery Times – The duration of the symptoms can differ significantly, with some recovering within weeks and others taking several months.
- Response to Treatment – Individuals may respond differently to similar treatments due to variations in underlying causes and overall health.
However, understanding these symptoms and their possible variations is crucial for those experiencing or diagnosing optic neuritis. Early consultation with a healthcare provider is advisable if any of these symptoms occur.
Causes of Optic Neuritis
Understanding the causes and their connection to other health conditions is crucial for both diagnosis and management.
Common Causes of Optic Neuritis
- Autoimmune Disorders: The most common link to optic neuritis is autoimmune disorders, where the immune system mistakenly attacks the body’s own tissues. Multiple sclerosis (MS) is the leading autoimmune disorder associated with optic neuritis. In MS, the immune system attacks the myelin sheath, the protective covering of the nerves, including those of the optic nerve.
- Infections: Certain viral and bacterial infections can lead to optic neuritis. Viruses such as measles, mumps, and herpes can trigger inflammation of the optic nerve. Bacterial infections, including Lyme disease and syphilis, can also be contributing factors.
- Other Health Conditions: Less commonly, conditions like sarcoidosis, which involves clusters of inflammatory cells in the body, and lupus, an autoimmune condition that causes widespread inflammation, can cause optic neuritis.
- Medications: Some drugs, particularly those that affect the immune system like interferon alpha and certain antibiotics, have been known to induce optic neuritis as a side effect.
- Vitamin Deficiencies: Severe deficiencies in essential nutrients like vitamin B12 can lead to damage of the optic nerve, potentially causing optic neuritis.
Connection to Autoimmune Disorders and Other Health Conditions
Optic neuritis is often considered a harbinger of autoimmune disorders, particularly multiple sclerosis. Approximately 50% of individuals who develop optic neuritis will eventually be diagnosed with multiple sclerosis. The inflammation in optic neuritis as related to MS is due to the immune system’s attack on the myelin sheath of the optic nerve.
Autoimmune factors aside, the relationship between optic neuritis and systemic infections or other inflammatory conditions emphasizes the importance of a comprehensive medical evaluation when this eye condition is diagnosed. Recognizing these links can lead to early identification and treatment of underlying systemic diseases, potentially improving outcomes for affected individuals.
However, optic neuritis is associated with a variety of causes, including autoimmune disorders, infections, other health conditions, certain medications, and nutritional deficiencies. Its connection to autoimmune diseases like MS underscores the need for thorough evaluation and management to address both the immediate symptoms and any underlying conditions.
Diagnosing Optic Neuritis
Accurate diagnosis is crucial for effective management and treatment. Here’s how medical professionals typically diagnose this condition:
List of Diagnostic Methods
- Clinical Evaluation: Initially, a detailed medical history is taken to understand any symptoms of vision loss, pain, or other related health issues.
- Ophthalmologic Examination: A comprehensive eye exam is conducted to assess visual acuity, color vision, pupil reactions, and the appearance of the optic disc.
- Visual Evoked Potentials (VEP): This test measures the electrical activity in the vision system when a visual stimulus is presented. A delay in response time can suggest optic neuritis.
- Magnetic Resonance Imaging (MRI): MRI scans are crucial in visualizing the optic nerve and brain to identify any lesions or abnormalities typical of optic neuritis, often associated with multiple sclerosis.
- Optical Coherence Tomography (OCT): This non-invasive imaging test provides high-resolution images of the retina, helping detect thinning of the retinal nerve fiber layer, a common feature in optic neuritis.
- Blood Tests: These may be conducted to rule out infectious or autoimmune conditions that can mimic or influence optic neuritis.
The Role of Ophthalmologic Examination
The ophthalmologic examination is vital in the diagnosis of optic neuritis for several reasons:
- Visual Function Assessment: It helps in evaluating how well the patient can see, which includes checking for visual acuity and color vision.
- Fundoscopic Exam: The optic nerve can be directly visualized to assess for swelling or other abnormalities.
- Pupillary Light Reflex: This test is important to check for an afferent pupillary defect, also known as a Marcus Gunn pupil, which is a classic sign of optic neuritis.
Importance of Differential Diagnosis
Differential diagnosis is essential in the evaluation of optic neuritis to distinguish it from other conditions that can present with similar symptoms, such as:
- Ischemic Optic Neuropathy: Typically affects older patients and presents with different fundoscopic findings.
- Neuromyelitis Optica: A distinct disease that affects the optic nerves and spinal cord but requires different treatment approaches.
- Infectious Causes: Such as syphilis or Lyme disease, which require specific types of treatment.
- Other Inflammatory Diseases: Conditions like sarcoidosis or lupus can also affect the optic nerve and need to be ruled out.
By conducting a thorough differential diagnosis, healthcare providers can ensure appropriate treatment and avoid potential complications associated with incorrect diagnosis and management.
Treatment Options for Optic Neuritis
Treatment is vital for managing symptoms and aiding recovery. Here, we explore the standard and emerging therapies for optic neuritis.
Standard Treatment Methods for Optic Neuritis
- Corticosteroids: The primary treatment for optic neuritis is corticosteroids. These drugs help reduce inflammation and accelerate the recovery of vision. High-dose intravenous methylprednisolone is often administered for three days, which may be followed by oral prednisone.
- Observation: In cases where symptoms are mild, doctors might recommend observation without immediate intervention. This approach relies on the body’s ability to heal naturally, as many patients experience spontaneous recovery.
Use of Steroids and Other Medications
- Intravenous Methylprednisolone: This potent steroid is used to decrease nerve inflammation quickly and is typically the first line of treatment to prevent further damage to the optic nerve.
- Oral Prednisone: Following IV steroids, an oral regimen may be prescribed to taper off the treatment gently, reducing potential side effects and helping manage inflammation.
- Pain Relievers: Over-the-counter pain medications, such as ibuprofen or acetaminophen, can be used to manage discomfort associated with optic neuritis.
Emerging Treatments and Therapies
- Immunomodulatory Therapies: For patients with recurrent episodes of optic neuritis, especially those linked to conditions like multiple sclerosis, immunomodulatory drugs such as interferons or monoclonal antibodies may be used to modify the immune system’s activity.
- Plasma Exchange (Plasmapheresis): In severe cases where steroids do not lead to recovery, plasma exchange might be considered. This procedure involves removing and replacing the blood plasma, potentially helping those who do not respond to steroid treatment.
- Biologics and Targeted Therapies: Research is ongoing into biologic agents that target specific pathways involved in inflammation and demyelination. These treatments hold promise for more personalized and effective management of optic neuritis.
- Neuroprotective Agents: Studies are investigating drugs that could protect nerve cells from damage during an episode of optic neuritis. This area of research aims to preserve vision and prevent long-term disability.
However, understanding the available treatments for optic neuritis is crucial for those experiencing this challenging condition. Always consult a healthcare professional for a diagnosis and personalized treatment plan.
Recovery and Management of Optic Neuritis
Recovering from optic neuritis can vary from person to person, but there are common experiences many patients share during this phase:
- Visual Improvement: Most patients start to notice an improvement in their vision within a few weeks after the onset of symptoms, although full recovery can take up to 12 months.
- Fluctuating Symptoms: It’s common for symptoms to fluctuate during the recovery period. Patients may experience periods where their vision improves, followed by moments where it seems to worsen slightly.
- Ongoing Assessments: Regular follow-ups with a healthcare provider are crucial. These visits help monitor the recovery of optic nerve function and adjust treatments as needed.
- Medication Effects: If steroids or other medications are prescribed to reduce nerve inflammation, patients might experience side effects such as mood swings, increased appetite, and changes in blood sugar levels.
Long-term Management Strategies
Managing optic neuritis over the long term involves several strategies to maintain eye health and prevent further issues:
- Regular Eye Examinations: Annual or biannual eye exams are essential to assess the health of the optic nerve and to check for any changes in vision.
- Monitoring for Multiple Sclerosis (MS): Since optic neuritis can be associated with MS, regular neurological evaluations might be recommended to monitor for symptoms of MS.
- Medication Adherence: For some patients, continuing medication to manage inflammation or to treat an underlying condition like MS is crucial. Consistent medication adherence is key to managing the condition effectively.
- Neuroprotective Measures: Research into neuroprotective treatments is ongoing. Patients should stay informed about new treatments that could help protect the optic nerve from further damage.
Lifestyle Adjustments and Supportive Care
Lifestyle adjustments and supportive care play a significant role in managing optic neuritis:
- Optimize Visual Environment: Enhancing the lighting in your living and work spaces can help reduce eye strain. Using high-contrast settings on screens and reading materials can also aid in visual clarity.
- Diet and Nutrition: Consuming a diet rich in antioxidants can help support nerve health. Foods high in omega-3 fatty acids, such as fish, flaxseeds, and walnuts, are recommended.
- Regular Exercise: Engaging in regular exercise can improve overall physical health and may help reduce the risk of MS in people with optic neuritis.
- Stress Management: Techniques such as meditation, yoga, and deep breathing can help manage stress, which may exacerbate symptoms.
- Support Groups: Connecting with others who are facing similar health challenges can provide emotional support and practical advice for dealing with optic neuritis.
However, regular communication with healthcare providers ensures that any changes in condition are addressed promptly, optimizing the outlook for recovery.
Complications and Risks Associated with Optic Neuritis
Potential Complications of Optic Neuritis
Optic neuritis, an inflammation of the optic nerve, can lead to several complications, primarily affecting vision. Key potential complications include:
- Permanent Vision Loss: While many recover substantial vision, a small percentage of individuals may experience permanent reduction in visual acuity.
- Color Vision Deficits: Damage to the optic nerve can lead to impaired color perception, often affecting the ability to distinguish between colors, especially reds and greens.
- Visual Field Defects: Individuals may experience partial vision loss in specific areas of their visual field, such as peripheral or central vision loss.
- Pain with Eye Movement: Persistent discomfort or pain when moving the eyes can continue even after other symptoms have subsided.
- Optic Atrophy: Long-term inflammation can lead to optic nerve damage, resulting in optic atrophy, which is characterized by the degeneration of nerve fibers.
Risk of Recurrence and Long-Term Effects on Vision
The risk of recurrence in optic neuritis varies, and several factors influence long-term visual outcomes:
- Recurrence: Approximately 35% of patients experience a recurrence of optic neuritis in either eye. The risk of recurrence can be higher in individuals with specific underlying health conditions, such as multiple sclerosis (MS).
- Development of Multiple Sclerosis: Up to 50% of individuals who experience an initial episode of optic neuritis may develop multiple sclerosis over subsequent years. MS-related optic neuritis tends to have a higher recurrence rate and more significant visual impairment.
- Chronic Visual Impairment: Although many patients regain much of their vision, about 10% may continue to have moderate to severe visual impairment. The extent of visual recovery typically stabilizes within 12 months after the initial episode.
- Contrast Sensitivity and Visual Quality: Even after apparent recovery, some individuals might struggle with reduced contrast sensitivity and visual quality, impacting daily activities like driving at night or distinguishing objects in low-contrast situations.
However, regular monitoring and consultation with healthcare professionals specializing in neurology and ophthalmology are recommended to mitigate these risks effectively.
The Future of Optic Neuritis Treatment
Optic neuritis, a demyelinating inflammation of the optic nerve often associated with multiple sclerosis (MS), presents significant challenges and opportunities in the field of neurology. As research progresses, the future of treating this condition looks promising with several innovative approaches on the horizon.
Research Trends and Potential Breakthroughs in Treatment
Recent years have seen a surge in the exploration of targeted therapies and personalized medicine for optic neuritis. Here are some key research trends and potential breakthroughs:
- Neuroprotective Agents: Researchers are investigating drugs that can protect nerve cells from damage. These agents aim to preserve vision and slow the progression of optic neuritis.
- Biologic Therapies: The development of biologics, which target specific pathways involved in immune responses, offers hope for more precise and effective treatments. These therapies could potentially reduce the autoimmune attacks on the optic nerve.
- Stem Cell Therapy: This innovative approach involves using stem cells to repair or replace damaged tissues in the optic nerve. Early studies suggest that stem cell therapy might restore some degree of vision in patients with severe optic neuritis.
- Advanced Imaging Techniques: Enhanced imaging technologies, such as optical coherence tomography (OCT), are becoming crucial in diagnosing and monitoring optic neuritis. These technologies allow for more precise assessments of nerve damage and treatment efficacy.
- Gene Therapy: Exploratory research into gene therapy shows potential for correcting genetic defects that contribute to optic nerve inflammation. This could lead to long-term solutions for patients predisposed to recurrent episodes of optic neuritis.
The Importance of Clinical Trials and Patient Participation
Clinical trials play a pivotal role in the advancement of optic neuritis treatments. The participation of patients in these trials is crucial for several reasons:
- Safety and Efficacy: Clinical trials are essential for determining the safety and effectiveness of new treatments. Patient participation helps ensure that therapies are tested on a diverse population, leading to more reliable data.
- Speeding Up Innovation: The more participants in a trial, the quicker researchers can gather the data needed to evaluate the potential of a new treatment. This accelerates the development process and brings new therapies to the market faster.
- Empowering Patients: Participating in clinical trials gives patients the opportunity to access cutting-edge treatments that are not yet widely available. It also allows them to contribute to scientific research that could benefit future generations.
- Tailored Treatments: Through trials, researchers can identify which treatments work best for specific patient groups. This information is crucial for developing personalized medicine approaches, which can significantly improve treatment outcomes.
As we continue to support these endeavors, we can look forward to breakthroughs that will enhance the quality of life and vision for those affected by this challenging condition.
FAQs about Optic Neuritis Treatment
What is Optic Neuritis?
Optic Neuritis is an inflammation of the optic nerve, which can cause sudden vision loss and pain, especially when moving the eyes.
What Causes Optic Neuritis?
Common causes include autoimmune disorders like multiple sclerosis, infections, and certain medications. Sometimes, the exact cause is unknown.
What are the Symptoms of Optic Neuritis?
Symptoms include blurred vision, loss of color vision, and eye pain. Some people may also experience flashes of light or a blind spot in the center of their vision.
How is Optic Neuritis Diagnosed?
Diagnosis typically involves a comprehensive eye exam, MRI scans, blood tests, and sometimes a lumbar puncture to rule out other conditions.
What Treatments are Available for Optic Neuritis?
Treatment options include corticosteroids to reduce inflammation and speed up recovery. In some cases, plasma exchange therapy might be used. Treatment for underlying conditions, such as multiple sclerosis, is also crucial.
Can Optic Neuritis be Cured?
While many people recover their vision fully or partially, some may have lasting vision problems. Early diagnosis and treatment can improve the chances of recovery.
Is Optic Neuritis a Recurrent Condition?
For some, particularly those with multiple sclerosis, optic neuritis can recur. Ongoing treatment and monitoring are essential to manage the condition effectively.
How Can I Manage Life with Optic Neuritis?
Managing optic neuritis involves regular medical check-ups, adhering to treatment plans, and making lifestyle adjustments to cope with vision changes. Support groups and counseling can also be beneficial.
Where Can I Find More Information?
Consult your eye doctor or neurologist for personalized advice. Reliable resources include medical websites like the Mayo Clinic, National Eye Institute, and multiple sclerosis organizations.
Conclusion
Recognizing and treating optic neuritis is crucial for preserving vision and maintaining overall eye health. Early detection can prevent serious complications and ensure better outcomes.
If you experience any visual symptoms, it’s essential to seek professional advice promptly. Don’t hesitate to consult an eye care specialist to get the proper diagnosis and treatment, ensuring the best care for your vision.
References
For further reading and to validate the information provided on Optic Neuritis treatment, here are some reputable sources:
- Mayo Clinic – A comprehensive guide on the symptoms, causes, and treatments of Optic Neuritis. Read more
- National Eye Institute – Detailed information on diagnosis and current research on Optic Neuritis. Learn more
- American Academy of Ophthalmology – Expert articles on treatment options and patient care for Optic Neuritis. Explore further
These sources offer in-depth knowledge and updates on Optic Neuritis, ensuring you have access to accurate and reliable information.