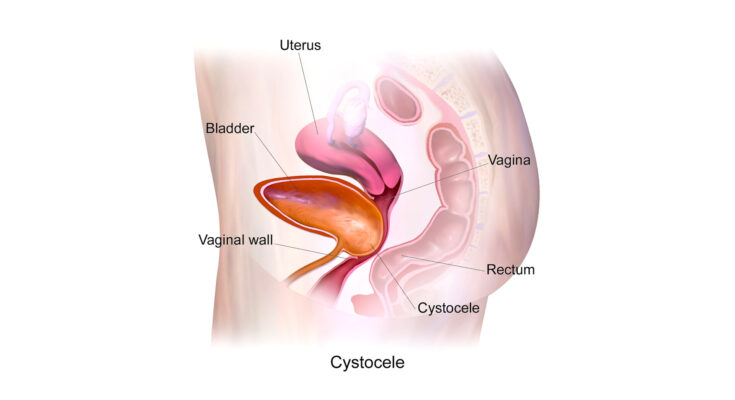
Anterior Vaginal Prolapse Diagnosis: Anterior vaginal prolapse, commonly referred to as a cystocele, is a condition that occurs when the bladder descends into the vagina.
This condition primarily affects women, particularly those who have experienced childbirth, menopause, or have a history of heavy lifting.
Understanding the diagnosis and treatment options for anterior vaginal prolapse is crucial for maintaining quality of life and sexual health.
Understanding Anterior Vaginal Prolapse
Anterior vaginal prolapse, commonly known as a bladder prolapse or cystocele, is a condition where the bladder sags or bulges into the vagina. This occurs when the pelvic floor muscles and tissues, which normally support the bladder, become weak or stretched. Understanding this condition is crucial, as it can significantly impact a woman’s quality of life.
Definition and Explanation
Anterior vaginal prolapse is characterized by the descent of the anterior vaginal wall and the bladder into the vaginal canal. This condition often arises due to a weakening in the pelvic floor muscles. The weakening can be a result of various factors, such as childbirth, aging, or surgery. Women with this condition may experience discomfort, urinary issues, and other complications that can affect daily activities.
Causes and Risk Factors
Several factors contribute to the development of anterior vaginal prolapse. Key causes include:
- Childbirth: Vaginal delivery can stretch or tear pelvic floor muscles.
- Aging: Natural loss of estrogen during menopause can weaken pelvic tissues.
- Heavy lifting or straining: Regularly lifting heavy objects or straining can stress pelvic muscles.
- Overweight or obesity: Excess weight increases pressure on pelvic organs.
- Previous pelvic surgery: Surgeries like a hysterectomy can affect pelvic support.
Statistics on Prevalence and Demographics Affected
Anterior vaginal prolapse is a common condition, particularly among older women and those who have had vaginal childbirth. According to studies, the prevalence increases with age. However, it can affect women of all ages, depending on their risk factors. It’s estimated that a significant percentage of women over the age of 50 experience some form of pelvic organ prolapse, which includes anterior vaginal prolapse.
Understanding anterior vaginal prolapse is vital for early recognition and management. Women experiencing symptoms should consult a healthcare provider for proper diagnosis and treatment options. Regular pelvic floor exercises, maintaining a healthy weight, and avoiding excessive straining can help prevent or alleviate the condition.
Symptoms of Anterior Vaginal Prolapse
Anterior vaginal prolapse, a condition affecting many women, manifests through various symptoms that are essential to recognize. The most common indicators include:
- Sensation of Pelvic Pressure: A feeling of heaviness or pressure in the pelvic area is often reported.
- Vaginal Bulging: Many patients describe a noticeable bulge in the vaginal area, which can be physically felt or seen.
- Discomfort During Intercourse: Experiencing pain or discomfort during sexual activities is a frequent symptom.
- Urinary Problems: Issues such as urinary incontinence, frequent urination, or a sensation of incomplete bladder emptying can occur.
- Lower Back Pain: Some individuals may also experience persistent lower back pain.
These symptoms can range from mild to severe, and their presence is a clear indicator that medical consultation is advisable.
Impact on Quality of Life and Health
The impact of anterior vaginal prolapse on a woman’s quality of life and overall health can be significant. It may lead to:
- Emotional Stress: Feelings of embarrassment or anxiety due to the condition’s symptoms.
- Physical Limitations: Difficulties in performing regular physical activities, affecting daily life.
- Sexual Health Concerns: Reduced sexual satisfaction or avoidance of sexual activity due to discomfort.
Understanding these impacts is vital, as they underscore the importance of addressing the condition proactively.
When to Seek Medical Advice
Seeking medical advice is crucial when symptoms of anterior vaginal prolapse become apparent. It’s especially important to consult a healthcare provider if:
- Symptoms Worsen: If there’s an increase in discomfort or if new symptoms develop.
- Impact on Daily Life: When the condition starts affecting daily activities or mental well-being.
- Concerns About Sexual Health: If experiencing pain during intercourse or other sexual health concerns.
Early intervention can lead to better management of the condition, improving both health and quality of life. Don’t hesitate to reach out to a healthcare professional for guidance and treatment options.
Diagnosis of Anterior Vaginal Prolapse
Understanding the diagnosis of anterior vaginal prolapse is crucial for both patients and healthcare providers. This condition, involving the weakening or displacement of the vaginal wall, can significantly impact a woman’s quality of life. Early and accurate diagnosis is key to effective management and treatment.
Overview of Diagnostic Procedures
The journey to diagnosing anterior vaginal prolapse typically begins with a comprehensive evaluation. This process is designed to assess the extent of the prolapse and identify any underlying causes or related conditions. Diagnostic procedures are non-invasive and tailored to each individual’s symptoms and medical history.
- Initial Consultation: This is the first step where the patient discusses symptoms and concerns with their healthcare provider. Common symptoms include a feeling of pressure or fullness in the pelvic area, discomfort during physical activities, and urinary problems.
- Medical History Review: A thorough review of the patient’s medical history is conducted. This includes any previous pregnancies, childbirth experiences, surgeries, and overall health status.
- Lifestyle and Symptom Assessment: Understanding the patient’s lifestyle, including physical activity levels and any factors that may exacerbate symptoms, is important.
Role of Medical History and Physical Examination
The cornerstone of diagnosing anterior vaginal prolapse is a detailed medical history and a comprehensive physical examination.
- Medical History: This includes gathering information about any previous gynecological issues, the number of pregnancies and deliveries, the mode of delivery (vaginal or cesarean), menopause status, and any previous pelvic surgeries.
- Physical Examination: A pelvic exam is conducted to assess the strength and structure of the vaginal walls and pelvic floor muscles. This examination helps in determining the degree of prolapse.
- Visual Inspection: The healthcare provider may also perform a visual inspection of the vaginal area to observe any noticeable prolapse.
Additional Tests
In some cases, additional tests may be required to further understand the extent of the prolapse or to rule out other conditions.
- Ultrasound: This imaging test can provide detailed images of the pelvic organs and help in assessing any abnormalities.
- Urodynamic Testing: For patients experiencing urinary symptoms, urodynamic tests can assess bladder function and help determine if the prolapse is affecting urinary control.
- MRI: In rare cases, an MRI may be used to get a detailed view of the pelvic floor and surrounding structures.
However, diagnosing anterior vaginal prolapse involves a combination of medical history review, physical examination, and possibly additional tests. Understanding this process is key for patients seeking to manage their symptoms effectively and healthcare providers aiming to deliver optimal care.
Treatment Options for Anterior Vaginal Prolapse
Understanding the range of treatment options is crucial for effective management. This guide provides an in-depth overview of the various approaches, tailored to cater to different stages and severity of the condition.
Non-Surgical Treatments
- Lifestyle Changes: Modifying certain lifestyle factors can alleviate symptoms. This includes weight management, dietary adjustments to prevent constipation, and avoiding activities that exacerbate the prolapse.
- Pelvic Floor Exercises: Strengthening the pelvic floor muscles through targeted exercises, often guided by a physiotherapist, can provide significant relief and prevent worsening of the prolapse.
- Pessary Use: A pessary, a device inserted into the vagina, supports the pelvic organs. This non-invasive option is ideal for those who prefer not to undergo surgery or are not suitable candidates for surgical intervention.
Surgical Options and Advancements
Surgery is often considered when non-surgical treatments fail to provide adequate relief. The latest advancements in surgical treatments for anterior vaginal prolapse focus on minimizing invasiveness and enhancing recovery times. These procedures can include:
- Anterior Vaginal Wall Repair: This traditional approach involves strengthening the vaginal wall.
- Mesh Procedures: While controversial, mesh procedures can offer a more permanent solution, with recent advancements aimed at reducing complications.
- Robotic and Laparoscopic Surgery: These minimally invasive techniques allow for more precision and potentially quicker recovery.
Customizing Treatment to Individual Needs
Each patient’s experience with anterior vaginal prolapse is unique. Customizing treatment plans to individual needs is paramount. Factors influencing treatment choice include age, severity of symptoms, overall health, and personal preferences. Collaboration between patient and healthcare provider is key to selecting the most appropriate and effective treatment strategy.
This comprehensive approach ensures that individuals facing anterior vaginal prolapse have access to a full spectrum of options, ranging from conservative to advanced surgical interventions, tailored to their specific needs and circumstances.
Recovery and Management for Anterior Vaginal Prolapse
Dealing with anterior vaginal prolapse can be challenging, but with the right care and lifestyle adjustments, recovery and prevention of recurrence is highly achievable. This section aims to guide you through post-treatment care, lifestyle modifications, and the long-term outlook for those dealing with this condition.
Post-Treatment Care and Management
After treatment, which may include surgery or nonsurgical methods, it’s crucial to follow your healthcare provider’s instructions for post-treatment care. This often involves:
- Rest and Recovery: Ensure ample rest to allow your body to heal. Avoid strenuous activities or lifting heavy objects for a recommended period.
- Pain Management: Follow prescribed pain management techniques and medications to alleviate discomfort.
- Follow-up Appointments: Attend all scheduled follow-up appointments to monitor your recovery and address any concerns promptly.
Lifestyle Modifications for Recovery and Prevention of Recurrence
Lifestyle changes play a vital role in recovery and preventing the recurrence of anterior vaginal prolapse:
- Pelvic Floor Exercises: Regularly perform pelvic floor exercises, like Kegels, to strengthen the muscles supporting your pelvic organs.
- Weight Management: Maintain a healthy weight to reduce pressure on your pelvic floor.
- Dietary Adjustments: High-fiber diets can prevent constipation, thereby reducing strain during bowel movements.
- Hydration: Adequate water intake is essential for preventing constipation.
- Quit Smoking: Smoking can worsen prolapse symptoms, so consider quitting or reducing smoking.
Long-term Outlook and Follow-up Care
The long-term outlook for anterior vaginal prolapse depends on various factors, including the severity of the prolapse, treatment method, and adherence to lifestyle modifications. Regular follow-up care is essential to monitor your condition and prevent recurrence. It may include:
- Routine Examinations: Regular pelvic exams to check the status of the prolapse.
- Monitoring Symptoms: Stay vigilant for any new or worsening symptoms and report them to your healthcare provider.
- Continued Lifestyle Adjustments: Maintain the lifestyle changes you’ve adopted for lasting results.
However, managing anterior vaginal prolapse involves a combination of professional medical care, self-care, and lifestyle adjustments. Adhering to these guidelines can significantly improve your quality of life and reduce the risk of recurrence. Remember, regular communication with your healthcare provider is key to a successful recovery.
Challenges and Considerations in Anterior Vaginal Prolapse (Cystocele) Treatment
Addressing this condition effectively requires a nuanced understanding of its challenges and considerations, particularly in diagnosis and treatment.
Challenges in Diagnosis
- Symptom Overlap: The symptoms of anterior vaginal prolapse often mimic those of other pelvic disorders, which can lead to misdiagnosis or delayed treatment.
- Patient Hesitancy: Many women may be reluctant to discuss symptoms due to embarrassment or cultural taboos surrounding pelvic health, leading to under-reporting.
- Assessment Complexity: Accurate diagnosis often requires specialized physical examinations and imaging, which may not be readily available in all healthcare settings.
Challenges in Treatment
- Varied Severity: Treatments must be tailored to the severity of the prolapse, ranging from conservative management to surgical intervention.
- Recurrence Risks: There is a significant risk of recurrence post-treatment, demanding ongoing monitoring and potential repeated interventions.
- Individual Health Factors: Co-existing conditions, such as obesity or diabetes, can complicate treatment choices and outcomes.
Considerations for Different Age Groups and Health Conditions
- Younger Women: In younger patients, fertility and childbirth plans must be considered, favoring conservative treatments where possible.
- Postmenopausal Women: Hormonal changes in postmenopausal women can affect tissue integrity, impacting both the risk of prolapse and treatment efficacy.
- Existing Health Conditions: Conditions like osteoporosis or cardiovascular diseases may influence treatment options, particularly concerning surgical risks.
- Lifestyle Factors: Weight management, physical activity, and pelvic floor exercises play a significant role in managing cystocele, especially in prevention and post-treatment care.
However, treating anterior vaginal prolapse is a complex process that demands a personalized approach. Healthcare providers must navigate the intricacies of diagnosis, consider the patient’s age, health conditions, and lifestyle, and continuously adapt to evolving challenges in treatment methodologies.
FAQs About Anterior Vaginal Prolapse and Its Treatment
1. What is Anterior Vaginal Prolapse?
Anterior vaginal prolapse, often referred to as a cystocele, occurs when the bladder drops into the vagina. This condition typically arises due to weakened pelvic floor muscles.
2. What Causes Anterior Vaginal Prolapse?
It’s commonly caused by factors like childbirth, aging, and increased abdominal pressure from activities such as heavy lifting. Hormonal changes during menopause can also contribute to its development.
3. What are the Symptoms of Anterior Vaginal Prolapse?
Symptoms may include a feeling of pressure or fullness in the pelvic area, discomfort during intercourse, urinary problems, and visible bulging at the vaginal opening.
4. How is Anterior Vaginal Prolapse Diagnosed?
A healthcare provider can diagnose this condition through a physical examination. In some cases, additional tests like ultrasound or cystoscopy may be required.
5. What are the Treatment Options for Anterior Vaginal Prolapse?
Treatment varies based on severity and symptoms. Options include pelvic floor exercises, pessary devices, and in more severe cases, surgical intervention.
6. Can Lifestyle Changes Help with Anterior Vaginal Prolapse?
Yes, lifestyle modifications such as maintaining a healthy weight, avoiding heavy lifting, and performing pelvic floor exercises can be beneficial.
7. Is Surgery Always Necessary for Anterior Vaginal Prolapse?
Not always. Surgery is typically recommended for more severe cases or when other treatments haven’t been effective.
8. What are the Risks of Anterior Vaginal Prolapse Surgery?
As with any surgery, risks include infection, bleeding, and complications related to anesthesia. Specific risks related to this surgery can be discussed with your healthcare provider.
9. How Long is the Recovery After Anterior Vaginal Prolapse Surgery?
Recovery time varies, but patients are often advised to limit physical activity for several weeks post-surgery.
10. Can Anterior Vaginal Prolapse Recur After Treatment?
There is a possibility of recurrence, especially if underlying causes such as chronic pressure on the pelvic floor are not addressed.
Conclusion
Anterior vaginal prolapse, while a challenging condition, is not insurmountable. Understanding its causes, symptoms, and the range of available treatments is the first step towards managing it effectively.
Remember, seeking professional medical advice is paramount in ensuring a safe and effective treatment journey. With the right care and attention, individuals can lead a comfortable and fulfilling life, despite this condition.