Angina Treatment: Angina, a symptom of coronary artery disease, is a critical health concern globally. It manifests as chest pain or discomfort, usually due to reduced blood flow to the heart muscle.
Understanding angina’s intricacies, including its diagnosis and treatment, is vital for both patients and healthcare providers.
Understanding Angina
Angina, a symptom of coronary artery disease, is a condition marked by chest pain or discomfort due to reduced blood flow to the heart. This vital information helps individuals recognize the warning signs and seek appropriate care.
Definition and Explanation of Angina
Angina is not a disease but a symptom of an underlying heart problem, usually coronary heart disease (CHD). It typically occurs when the heart muscle doesn’t get as much blood and oxygen as it needs, often because of narrowing or blockage in the heart arteries. This can lead to chest pain or discomfort, often felt as pressure, squeezing, or aching in the chest.
Types of Angina
- Stable Angina: This most common form occurs during physical exertion or stress. The pain is predictable and usually subsides with rest or medication.
- Unstable Angina: More serious and unpredictable, this type can occur at rest and signals a higher risk of a heart attack. It requires immediate medical attention.
- Variant (Prinzmetal’s) Angina: This rare form is caused by a spasm in the heart’s arteries. It can occur at rest and is often severe.
Causes and Risk Factors of Angina
The primary cause of angina is reduced blood flow to the heart muscle due to coronary artery disease. Risk factors include:
- Age: Increased risk in men over 45 and women over 55.
- Tobacco Use: Smoking and long-term exposure to secondhand smoke damage the interior walls of arteries.
- High Blood Pressure: Over time, it can damage arteries leading to the heart.
- High Cholesterol: High levels of bad cholesterol can lead to plaque buildup in arteries.
- Diabetes: Increases the risk of coronary artery disease.
- Obesity: Excess weight typically worsens other risk factors.
- Physical Inactivity: Contributes to high cholesterol and obesity.
- Stress: Can damage arteries and worsen other risk factors for CHD.
- Family History: A family history of heart disease increases the risk.
Understanding angina and its various forms is crucial for prompt diagnosis and treatment, which can significantly improve quality of life and reduce the risk of heart attack. Regular check-ups and addressing risk factors are key preventive measures. If you experience symptoms of angina, seek medical attention immediately.
Symptoms of Angina: Understanding the Signs
Recognizing the differences between angina symptoms and other types of chest pain can be crucial for early intervention and treatment.
Common Symptoms of Angina
- Chest Pain or Discomfort: The most common symptom, often felt in the chest’s center.
- Radiating Pain: Pain may spread to the arms, neck, jaw, shoulder, or back.
- Shortness of Breath: Difficulty in breathing or feeling winded, often accompanying chest pain.
- Nausea and Fatigue: Feeling sick to your stomach, unusually tired, or weak.
- Dizziness or Lightheadedness: Feeling faint or dizzy, especially with activity.
How Angina Differs from Other Chest Pain
Angina pain is usually triggered by physical exertion or stress and subsides with rest or medication. In contrast, other types of chest pain, like that from a stomach issue, may worsen when lying down or after eating.
Recognizing a Heart Attack vs. Angina
While angina is a symptom of a strained heart, a heart attack occurs when the blood flow to the heart is significantly or completely blocked. Here’s how to distinguish:
- Duration: Heart attack pain is usually more prolonged and intense than angina.
- Response to Rest or Medication: Angina typically eases with rest or angina medication, but heart attack symptoms do not.
- Additional Symptoms: Heart attacks often come with severe symptoms, like cold sweats, nausea, and an overwhelming sense of anxiety.
Understanding the symptoms of angina and how they differ from other types of chest pain, including heart attacks, is crucial. If you experience any of these symptoms, seek medical advice immediately. Early detection and treatment can save lives and prevent more severe heart conditions.
Diagnosing Angina
Here we will provides a comprehensive overview of the various diagnostic methods employed in detecting angina, emphasizing the significance of early diagnosis in effectively managing this condition.
Diagnostic Methods for Angina
- Electrocardiogram (ECG): An ECG records the electrical activity of the heart and is a primary tool in diagnosing angina. It helps in identifying irregular heart rhythms and signs of heart strain or damage.
- Stress Testing: Stress tests, conducted while the patient exercises, measure the heart’s performance and blood flow under stress. These tests can reveal problems with blood flow within the heart, a key indicator of angina.
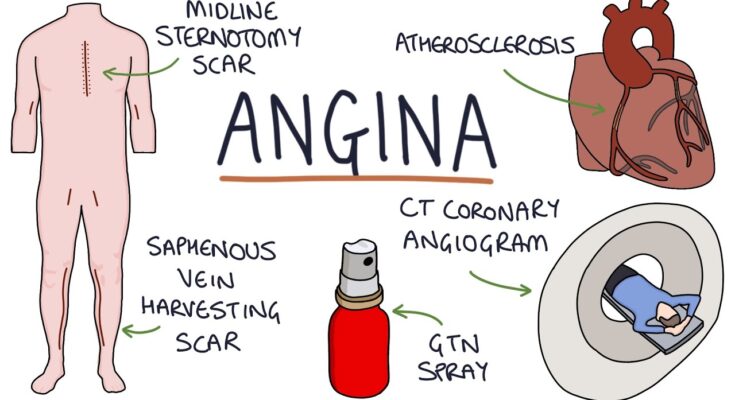
- Imaging Techniques: Various imaging methods, such as echocardiograms, coronary angiograms, and cardiac CT scans, are used to visualize the heart’s structure and blood flow. These techniques can identify blockages in the coronary arteries, the root cause of angina.
Importance of Early Diagnosis in Angina Management
Early diagnosis of angina is vital for several reasons:
- Preventing Heart Damage: Early detection allows for timely intervention, preventing potential heart damage.
- Improving Quality of Life: Accurate diagnosis leads to appropriate treatment plans, improving the patient’s overall quality of life.
- Reducing Risk of Heart Attacks: Early management of angina reduces the risk of more severe complications like heart attacks.
However, employing these diagnostic methods effectively and recognizing the importance of early diagnosis are key to managing angina. Early intervention not only saves lives but also enhances the patient’s quality of life, making it a critical aspect of healthcare in cardiac conditions.
Angina Treatment Strategies
Understanding First-Line Treatments for Angina
It’s crucial to address angina promptly with effective treatment strategies. The first line of defense typically involves a combination of medications and lifestyle modifications.
Medications: Patients are often prescribed a range of drugs such as nitrates (to widen blood vessels and improve blood flow to the heart), beta-blockers (to decrease heart workload and oxygen demand), and calcium channel blockers (to relax heart arteries). Each of these medications plays a vital role in managing the symptoms of angina.
Lifestyle Changes: Alongside medication, lifestyle adjustments are essential. This includes embracing a heart-healthy diet, engaging in regular exercise (as recommended by a healthcare provider), quitting smoking, and managing stress. These changes can significantly reduce the frequency and severity of angina attacks.
Exploring Various Angina Treatment Options
While first-line treatments are effective for many, there’s a range of other options available for managing angina:
- Angioplasty and Stenting: In cases where angina is caused by significant blockages in the arteries, procedures like angioplasty (widening narrowed arteries) and stenting (placing a small mesh tube to keep the artery open) can be effective.
- Coronary Artery Bypass Surgery: For severe coronary artery disease, this surgery creates a new pathway for blood to reach the heart, bypassing blocked arteries.
- Enhanced External Counterpulsation (EECP): This non-invasive treatment involves compressing blood vessels in the lower limbs to increase blood flow to the heart.
Each of these options has its indications and considerations, which should be discussed with a healthcare provider.
The Role of Medication in Angina Management
Medications remain a cornerstone in the management of angina.
- Nitrates: These are among the most commonly prescribed medications for angina. They work rapidly to relieve pain by widening blood vessels and reducing the heart’s oxygen demand.
- Beta-Blockers: By slowing down the heartbeat, beta-blockers reduce the heart’s workload and oxygen needs, thus helping in angina control.
- Calcium Channel Blockers: These drugs relax and widen the arteries, improving blood flow to the heart muscle and easing angina symptoms.
However, managing angina involves a comprehensive approach that combines medication, lifestyle changes, and potentially more invasive procedures. It’s vital to work closely with a healthcare provider to determine the best treatment plan for individual needs.
Living with Angina
Living with angina can be challenging, but with the right lifestyle modifications and preventive measures, it’s possible to manage the condition effectively and maintain a good quality of life. Here’s a guide on how to live well with angina, focusing on diet, exercise, and psychological support.
Lifestyle Modifications and Preventive Measures for Angina
Managing angina involves addressing the underlying causes and adopting heart-healthy habits.
Heart-Healthy Habits
- Quit Smoking: Smoking is a major risk factor for heart disease. Quitting smoking can significantly reduce the risk of angina and other heart-related issues.
- Control Blood Pressure and Cholesterol: High blood pressure and cholesterol can aggravate angina. Regular check-ups and medication (if prescribed) are crucial.
- Stress Management: Stress can trigger angina. Techniques like meditation, yoga, or other relaxation methods can help manage stress levels.
Managing Angina through Diet and Exercise
Diet for Heart Health
- Balanced Diet: Focus on a diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats.
- Limit Saturated Fats and Salt: Reducing saturated fats and salt can help manage cholesterol levels and blood pressure, reducing the risk of angina.
Exercise Regularly
- Start Slow: Gradually increase your activity level, especially if you’ve been inactive.
- Choose Heart-Healthy Activities: Walking, swimming, and cycling are great options. Always consult with a healthcare provider before starting any new exercise regimen.
Psychological Impact and Support Systems for Individuals with Angina
Addressing Mental Health
- Understanding the Emotional Impact: Angina can lead to fear, anxiety, and depression. Recognizing these emotions is the first step in managing them.
- Seek Professional Help: Consult a mental health professional if you’re struggling to cope with the emotional aspects of angina.
Building a Support System
- Family and Friends: Keep close contact with loved ones. Sharing your experiences can provide emotional support.
- Support Groups: Joining a support group for people with heart conditions can provide a sense of community and shared understanding.
Education and Empowerment
- Stay Informed: Understanding your condition empowers you to make informed decisions about your health.
- Regular Medical Check-ups: Regular visits to your healthcare provider are important for managing angina effectively.
Living with angina requires a multifaceted approach that includes lifestyle changes, dietary adjustments, regular exercise, and addressing the psychological impacts. With these strategies, individuals with angina can lead fulfilling lives while effectively managing their condition. Remember, it’s important to work closely with healthcare professionals to tailor these recommendations to your individual needs.
Prevention of Angina: Essential Strategies for Heart Health
Preventing angina involves adopting a heart-healthy lifestyle to mitigate the risk factors associated with coronary artery disease.
Regular Health Check-Ups: Your First Line of Defense
Regular health check-ups play a crucial role in preventing angina. These check-ups can help identify risk factors such as high blood pressure, high cholesterol, and diabetes early on. Early detection enables timely intervention, significantly reducing the risk of developing angina.
Lifestyle Changes: A Cornerstone in Preventing Angina
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins helps maintain a healthy weight and reduces cholesterol levels, both vital in preventing angina.
- Regular Exercise: Engaging in moderate physical activity for at least 30 minutes most days of the week improves cardiovascular health and helps prevent angina.
- Smoking Cessation: Smoking is a major risk factor for coronary artery disease. Quitting smoking significantly reduces the risk of developing angina.
- Stress Management: Chronic stress can strain the heart and contribute to angina. Techniques like mindfulness, yoga, or other relaxation methods can be beneficial.
- Moderate Alcohol Consumption: Excessive alcohol intake can increase blood pressure. Limiting alcohol consumption can help in preventing angina.
- Weight Management: Being overweight increases the strain on your heart. Maintaining a healthy weight is essential in preventing angina and other heart-related issues.
Risk Factor Management: A Targeted Approach
Managing existing health conditions is crucial in preventing angina. Conditions like high blood pressure, high cholesterol, and diabetes directly impact heart health. Working with a healthcare provider to manage these conditions through medication, diet, and lifestyle changes is essential.
Preventing angina involves a multifaceted approach focused on regular health check-ups and comprehensive risk factor management. By adopting a healthy lifestyle, managing existing health conditions, and staying vigilant about heart health, individuals can significantly reduce their risk of developing angina.
FAQ Section: Understanding Angina and Its Treatment
1. What is angina?
Angina is a type of chest pain caused by reduced blood flow to the heart muscles. It’s often a symptom of coronary artery disease and can feel like pressure or squeezing in your chest.
2. What are the main causes of angina?
The primary cause of angina is the narrowing of coronary arteries due to plaque buildup, known as atherosclerosis. Other factors like stress, physical exertion, and cold weather can also trigger angina.
3. How is angina diagnosed?
Doctors diagnose angina through a patient’s medical history, a physical exam, and various tests like electrocardiograms (ECG), stress tests, echocardiograms, or coronary angiography.
4. What are the different types of angina?
There are mainly three types: stable angina (occurs predictably and with exertion), unstable angina (more unpredictable and severe), and variant (Prinzmetal’s) angina (caused by a spasm in coronary arteries).
5. What treatments are available for angina?
Treatment options include lifestyle changes, medications (like nitrates, beta-blockers, or calcium channel blockers), and in some cases, medical procedures like angioplasty or coronary artery bypass surgery.
6. Can lifestyle changes help with angina?
Yes, lifestyle changes such as maintaining a healthy weight, quitting smoking, eating a heart-healthy diet, and regular exercise can significantly help manage angina.
7. Is angina a heart attack?
No, angina is not a heart attack, but it indicates a higher risk of heart attacks. Immediate medical attention is necessary if chest pain is severe, prolonged, or accompanied by other symptoms like shortness of breath or sweating.
8. How can I prevent angina?
Preventing angina involves controlling risk factors like high blood pressure, high cholesterol, diabetes, obesity, and smoking. Regular check-ups and following a heart-healthy lifestyle are also crucial.
9. When should I see a doctor for angina?
You should see a doctor if you experience symptoms of angina, especially if they’re new, worsening, or occurring more frequently. Early diagnosis and treatment are essential.
10. Can angina be cured?
While there’s no cure for angina, it can be effectively managed with treatment and lifestyle changes. Ongoing care and monitoring are important to manage symptoms and prevent complications.
Conclusion
In conclusion, addressing angina with a comprehensive approach is not just about treating a symptom; it’s about taking proactive steps towards safeguarding heart health, preventing serious complications, and enhancing the overall well-being of patients.
This approach underscores the importance of integrated care, where diagnosis, treatment, and patient education are seamlessly interwoven to ensure the best possible outcomes.