Anal Fistula Symptoms: Anal fistulas are a challenging and often painful condition that affects a significant portion of the population.
Understanding the symptoms and causes of anal fistulas is crucial for early diagnosis and effective treatment.
This comprehensive guide aims to provide in-depth information on this medical condition, helping individuals identify potential signs and understand the underlying causes.
Understanding Anal Fistulas
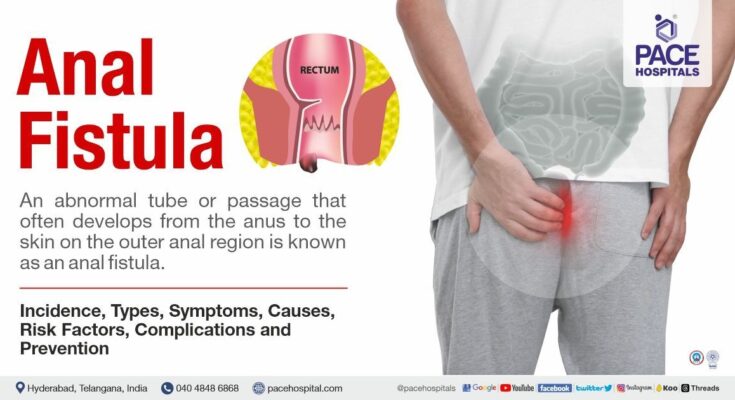
Anal fistulas, commonly misunderstood and often misdiagnosed, are abnormal connections between the epithelial-lined surface of the anal canal and the perianal skin. They originate from an infection near the anus, leading to an abscess that develops into a fistula. This medical condition is characterized by pain, discomfort, and sometimes the discharge of pus or blood. Understanding the intricate nature of anal fistulas is crucial for effective diagnosis and treatment.
Differentiation from Other Similar Conditions
Distinguishing anal fistulas from other anal or rectal conditions is vital for proper management. They are often confused with hemorrhoids, fissures, or abscesses, each with unique symptoms and treatments. Hemorrhoids, for instance, are swollen veins in the rectum and anus, causing itching, pain, and bleeding. Fissures refer to small tears in the lining of the anus, often resulting from hard stools or constipation. Abscesses are pus-filled infections near the anus or rectum. Unlike these conditions, fistulas are defined by their tract-like nature, forming a tunnel between different areas near the anus.
Prevalence or Statistics
Anal fistulas are not exceptionally common but are significant due to the discomfort they cause. Statistics indicate that they are more prevalent in men than in women and are most commonly diagnosed in individuals between 20 and 40 years old. The prevalence rate varies globally, but certain lifestyle factors, such as diet and hygiene, can influence their occurrence. Additionally, individuals with specific medical conditions, like Crohn’s disease or other inflammatory bowel diseases, are at a higher risk of developing anal fistulas.
By understanding anal fistulas, their differentiation from similar conditions, and their prevalence, individuals and healthcare professionals can better approach diagnosis and treatment, leading to more effective management and improved patient outcomes.
Symptoms of Anal Fistulas
A comprehensive overview of the symptoms associated with anal fistulas, offering guidance on how to recognize them and understand when it’s essential to seek medical advice.
Identifying Symptoms of Anal Fistulas
Anal fistulas, primarily caused by an infection near the anus leading to an abscess, can manifest through various symptoms. Recognizing these signs is crucial for timely treatment. Here are the key symptoms to be aware of:
- Persistent Pain: This is often throbbing and worsens when sitting down.
- Irritation of the Skin: The area around the anus becomes irritated, red, and swollen.
- Discharge: A foul-smelling discharge that may be pus or blood.
- Bleeding: Noticeable bleeding when using the toilet.
- Swelling: A noticeable lump or swelling near the anus.
- Fever and Discomfort: In some cases, a fever and general feeling of being unwell.
How to Recognize These Symptoms
To accurately recognize the symptoms of anal fistulas, it’s important to pay attention to your body’s signals. If you experience persistent pain around the anus, especially if accompanied by discharge or swelling, it’s a strong indicator. The discomfort might increase during bowel movements, sitting, or physical activities. Skin irritation and bleeding are also key signs to watch out for.
When to Seek Medical Advice
It’s crucial to consult a healthcare professional if you experience any of the symptoms mentioned above, especially if they persist or worsen over time. Anal fistulas can lead to complications if left untreated, including infection spread and recurrence of abscesses. Early medical intervention can provide effective treatment and prevent further health issues.
However, understanding and recognizing the symptoms of anal fistulas is vital for timely medical intervention. Persistent pain, discharge, bleeding, and swelling near the anus are clear indicators that should prompt a visit to a healthcare provider. Staying informed and vigilant about these symptoms ensures better health outcomes and effective management of the condition.
Causes of Anal Fistulas
In this comprehensive breakdown, we will explore the various causes, risk factors, and contributing conditions that lead to the development of anal fistulas, and how they are connected to the onset of symptoms.
Primary Causes of Anal Fistulas
- Anal Abscesses: The most common cause of anal fistulas is an anal abscess. An abscess is a collection of pus that results from an infection. When these abscesses don’t heal properly, they can develop into a fistula.
- Inflammatory Bowel Diseases (IBD): Conditions like Crohn’s disease and ulcerative colitis, which cause chronic inflammation of the gastrointestinal tract, can also lead to the development of anal fistulas.
- Diverticulitis: Inflammation or infection of small pouches that can form in your intestines (diverticula) may contribute to fistula formation.
- Infection: Bacterial, fungal, or viral infections in the anal area can lead to the formation of an abscess and eventually a fistula.
Risk Factors and Contributing Conditions
- Chronic Constipation: Repeated strain during bowel movements can increase the risk of developing an anal fistula.
- Sexually Transmitted Infections (STIs): Certain STIs can cause infections in the anal area, potentially leading to fistulas.
- Previous Surgery: Surgeries near the anus, such as for hemorrhoids, can sometimes lead to fistulas.
- Trauma: Injury to the anal area can also be a contributing factor.
Connection Between Causes and Symptoms
The development of symptoms in anal fistulas is closely tied to the underlying cause. For instance:
- Fistulas stemming from abscesses often present with pain, swelling, and redness.
- In cases related to IBD, symptoms may include irregular bowel movements and abdominal pain.
- Infections typically present with fever and drainage from the fistula.
Understanding the causes and their connection to symptoms is vital for diagnosis and treatment. Early intervention can prevent complications and improve outcomes.
By providing a detailed analysis of the causes, risk factors, and symptom development of anal fistulas, this article serves as a valuable resource for individuals seeking to understand this medical condition. For those experiencing symptoms, consulting a healthcare professional for a proper diagnosis and treatment plan is essential.
Diagnosing Anal Fistulas: A Comprehensive Guide
Here, we delve into the diagnostic process for anal fistulas, offering insights into the types of medical tests and examinations used, as well as the critical role of symptoms in reaching an accurate diagnosis.
1. Recognizing the Symptoms: The First Step in Diagnosis
The journey to diagnosing an anal fistula often begins with a keen understanding of the symptoms. Patients may experience discomfort, pain, or irritation around the anal area, along with other signs like abnormal discharge or bleeding. Recognizing these symptoms is crucial, as it prompts the individual to seek medical attention, setting the stage for a more thorough evaluation by healthcare professionals.
2. Medical Examinations: The Cornerstone of Diagnosis
Upon consulting a healthcare provider, a series of medical examinations are typically conducted. These include:
- Physical Examination: A fundamental aspect of the diagnostic process, where a doctor visually inspects the anal area and may perform a digital rectal exam to feel for abnormalities.
- Anoscopy: A specialized procedure where a small instrument, an anoscope, is inserted into the anus to provide a clearer view of the internal anal canal.
- Proctosigmoidoscopy: In some cases, a more extensive examination of the lower bowel may be necessary, for which proctosigmoidoscopy is used.
3. Advanced Diagnostic Tests: Enhancing Accuracy
In addition to physical examinations, healthcare providers may employ advanced diagnostic tests to confirm the presence of an anal fistula and understand its complexity. These tests include:
- Ultrasound: This imaging test can help visualize the fistula and determine its path.
- Magnetic Resonance Imaging (MRI): An MRI provides a detailed image of the anal region, aiding in the assessment of the fistula’s route and the identification of any abscesses.
- Fistulography: A specialized X-ray procedure where a contrast dye is injected into the fistula tract to make it visible on X-ray images.
4. The Role of Symptoms in Diagnosis
Symptoms play a pivotal role in the diagnostic process. They not only alert individuals to the possibility of an anal fistula but also provide healthcare providers with essential clues about the severity and nature of the condition. A detailed understanding of the patient’s symptoms, combined with the results from physical examinations and diagnostic tests, enables a comprehensive evaluation and an accurate diagnosis.
Diagnosing anal fistulas requires a multi-faceted approach that encompasses a careful assessment of symptoms, thorough physical examinations, and advanced diagnostic tests. By leveraging these tools, healthcare professionals can accurately identify and effectively manage this condition, offering relief and improving the quality of life for those affected.
Complications Associated with Anal Fistulas
These fistulas, essentially abnormal connections between the anal canal and the skin near the anus, can significantly impact a patient’s quality of life.
The Risks of Untreated Anal Fistulas
If left untreated, anal fistulas can lead to a range of complications, some of which are severe:
- Infection and Abscess Formation: The primary risk is the development of an abscess, a painful collection of pus caused by infection. Abscesses can exacerbate discomfort and lead to further complications.
- Recurrent or Chronic Infections: Repeated infections are common in untreated fistulas. These infections can become chronic, causing ongoing pain and discomfort.
- Spread of Infection: In severe cases, the infection can spread to other parts of the body, leading to more serious health issues.
- Fecal Incontinence: In some cases, the fistula can damage the muscles that control bowel movements, leading to fecal incontinence.
- Impact on Mental Health: The persistent discomfort and stress associated with untreated anal fistulas can significantly affect mental health, leading to conditions like anxiety and depression.
The Importance of Early Detection and Treatment
Early detection and treatment of anal fistulas are crucial. Timely medical intervention can prevent the aforementioned complications and improve the overall prognosis. Treatment options vary depending on the severity and location of the fistula but may include:
- Surgical Intervention: The most common treatment, surgery aims to close the fistula while preserving anal sphincter function.
- Medication: In certain cases, antibiotics or other medications may be used to treat infection or underlying conditions contributing to fistula formation.
- Lifestyle Modifications: Dietary changes and improved hygiene can assist in managing symptoms and preventing exacerbation.
However, understanding the potential complications of anal fistulas highlights the importance of seeking medical advice at the earliest signs of this condition. Prompt treatment not only alleviates discomfort but also plays a vital role in preventing serious health consequences. Regular check-ups and being attentive to symptoms are key in managing this condition effectively.
Treatment Options for Anal Fistulas
Anal fistulas, a challenging condition to manage, require a well-thought-out treatment plan. Understanding the common approaches and how they alleviate symptoms is key to effective management.
Common Treatment Approaches
- Surgical Intervention: The most prevalent treatment for anal fistulas is surgery. Procedures like fistulotomy involve cutting open the fistula tract, allowing it to heal from the inside out. Surgeons may opt for different techniques based on the fistula’s complexity and location.
- Seton Placement: In cases where fistulotomy isn’t viable, a seton—a thread-like device—may be used. This technique helps drain the fistula and aids in the gradual healing process.
- Advancement Flap Procedure: This surgical method involves creating a flap from the rectal wall to cover the internal fistula opening, promoting healing while preserving sphincter muscles.
- Fibrin Glue and Bioprosthetic Plugs: These less invasive options involve sealing the fistula tract with fibrin glue or placing a biodegradable plug. They are often preferred for their minimal impact on continence.
- Medications and Antibiotics: In some cases, particularly for individuals with inflammatory bowel disease, medication may be used to control infection and inflammation.
Alleviating Symptoms
Effective treatment of anal fistulas not only addresses the physical condition but also significantly improves the patient’s quality of life. The chosen treatment method aims to:
- Relieve Pain and Discomfort: Surgical and non-surgical treatments reduce the pain and discomfort associated with anal fistulas, allowing patients to resume daily activities with ease.
- Prevent Infections: By properly managing the fistula, the risk of recurrent infections and abscesses is greatly reduced.
- Maintain Continence: Advanced surgical techniques focus on preserving the anal sphincter muscles, ensuring that continence is maintained post-treatment.
- Promote Healing: The ultimate goal of any treatment is to promote the healing of the fistula, preventing recurrence and enabling a return to normalcy.
However, the treatment of anal fistulas, though complex, offers several approaches tailored to individual needs. Consulting with healthcare professionals to choose the right treatment plan is crucial for effective management and symptom relief.
Prevention and Management of Anal Fistulas
Prevention Tips for Anal Fistulas
Anal fistulas, though complex, can often be prevented with certain lifestyle adjustments. Here are some effective prevention strategies:
- Maintain Hygiene: Regular and thorough cleaning of the anal area helps prevent infections that can lead to fistulas.
- Healthy Bowel Movements: Strive for regular bowel movements to avoid constipation and straining, which can contribute to the development of fistulas. Including fiber-rich foods in your diet can aid in this.
- Stay Hydrated: Adequate water intake keeps the stool soft, reducing the strain during bowel movements.
- Prompt Treatment of Anorectal Conditions: Early treatment of conditions like hemorrhoids, abscesses, and inflammatory bowel diseases (IBD) can prevent fistula formation.
- Regular Exercise: Exercise aids in maintaining a healthy bowel routine and can prevent constipation.
Dietary and Lifestyle Changes for Symptom Management
If you’re managing an anal fistula, certain lifestyle and dietary changes can alleviate symptoms:
- Fiber-Rich Diet: High-fiber foods like fruits, vegetables, and whole grains can help in smoother bowel movements.
- Fluid Intake: Increasing your water intake helps soften stools, making them easier to pass.
- Avoid Irritants: Spicy foods, caffeine, and alcohol can aggravate symptoms, so it’s best to limit them.
- Sitz Baths: Regular warm baths can reduce discomfort and promote healing.
- Stress Management: Stress can exacerbate symptoms, so incorporating stress-reduction techniques like yoga or meditation can be beneficial.
Remember, while these tips can help in prevention and management, it’s important to consult a healthcare professional for a personalized treatment plan. Regular medical check-ups and following your doctor’s advice are crucial in effectively dealing with anal fistulas.
FAQs: Understanding Anal Fistula Symptoms and Causes
Q1: What are the typical symptoms of an anal fistula?
A: Common symptoms include discomfort and pain around the anus, particularly when sitting or moving. There might also be swelling, redness, or tenderness. In some cases, patients notice an abnormal discharge or bleeding from the area.
Q2: Can anal fistulas lead to other complications if left untreated?
A: Yes, untreated anal fistulas can lead to serious complications like recurrent abscesses, systemic infection, and even increased risk of certain types of cancer in chronic cases.
Q3: What causes an anal fistula to develop?
A: Anal fistulas often result from an infection in the anal glands. Other causes include conditions like Crohn’s disease, previous surgery, trauma to the area, or an underlying condition such as tuberculosis.
Q4: Are certain individuals more at risk of developing an anal fistula?
A: People with inflammatory bowel diseases like Crohn’s disease or ulcerative colitis are at a higher risk. Also, individuals with a history of anal abscesses, chronic constipation, or who have undergone previous rectal surgery may be more susceptible.
Q5: How is an anal fistula diagnosed?
A: Diagnosis typically involves a physical examination, and in some cases, additional tests like an ultrasound, MRI, or a fistulogram may be required to assess the fistula’s path.
Q6: What are the treatment options for an anal fistula?
A: Treatment varies depending on the fistula’s complexity. Options range from medication to manage symptoms to surgical procedures like fistulotomy or seton placement, aimed at healing the fistula while preserving sphincter muscles.
Conclusion
We strongly encourage anyone experiencing symptoms indicative of an anal fissure to seek medical advice. Early consultation with a healthcare professional can lead to effective treatment plans, alleviate symptoms, and prevent complications. Remember, addressing anal fissure symptoms promptly not only ensures better health outcomes but also improves overall quality of life.
Don’t let discomfort or hesitation hinder your path to wellness. Recognizing and acting upon these symptoms is a step towards a healthier, more comfortable life.