Hypospadias Symptoms: Hypospadias is a congenital condition affecting the urethra in males, where the urinary opening is not located at the usual position at the tip of the penis. This condition can influence both urinary function and reproductive health.
However, understanding the symptoms and causes of hypospadias is crucial for early diagnosis and effective treatment.
Understanding Hypospadias
Hypospadias is a congenital condition affecting males where the opening of the urethra is not located at the tip of the penis. This can lead to challenges with urination and, later in life, sexual health. Understanding the prevalence and diagnosis of hypospadias can help parents and caregivers better prepare and manage this condition.
Statistics on the Prevalence of Hypospadias
Hypospadias is relatively common, though its frequency can vary by region and population. Generally, it affects about 1 in every 200 to 300 male births worldwide. This makes it one of the most common congenital anomalies in males. Monitoring trends and understanding these statistics are crucial as they help in the early identification and treatment of the condition.
Age of Diagnosis for Hypospadias
Hypospadias is typically diagnosed shortly after birth during the first examination by a pediatrician. The condition is identified by the abnormal placement of the urethral opening. Early diagnosis is essential for planning potential treatments, which are usually surgical and are most effectively performed during the first year of life. Early intervention is aimed at improving functional outcomes and minimizing future complications related to the condition.
By increasing awareness and understanding of hypospadias, healthcare providers can ensure timely and effective treatment, significantly improving the quality of life for those affected.
Symptoms of Hypospadias
Understanding its symptoms can aid in early diagnosis and treatment. Here’s an overview of the primary and secondary symptoms, as well as guidance on identifying symptoms in infants.
Primary Symptoms of Hypospadias
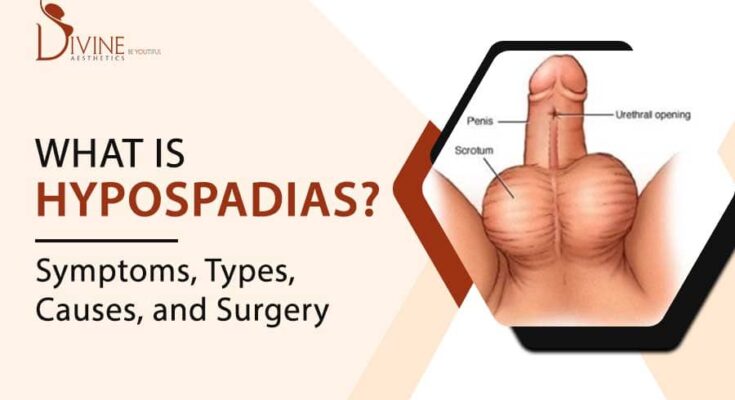
The most noticeable symptom of hypospadias is the position of the urethral opening. Instead of being located at the tip of the penis, it may be found anywhere along the underside of the penis, from just below the tip to the scrotum. Primary symptoms include:
- Abnormal Position of Urethral Opening: The urethra does not open at the usual location at the tip of the penis.
- Downward Curve of the Penis: Known as chordee, this curvature can occur as the child grows.
- Hooded Appearance of the Penis: The foreskin may be underdeveloped on the underside, giving the penis a hooded appearance.
Secondary Symptoms and Related Complications
While the primary symptoms focus on the physical abnormalities, secondary symptoms can involve functional issues related to urination and future sexual function. These include:
- Spraying or Dribbling During Urination: The abnormal position of the urethra can affect the urine stream, causing spraying or dribbling.
- Difficulty Aiming Urine Stream: This can make toilet training more challenging as the child may have difficulty directing the urine stream.
- Potential for Urinary Tract Infections: Misdirected urine flow can increase the risk of infections.
How to Identify Symptoms in Infants
Detecting hypospadias in infants requires careful observation of the physical structure and urinary habits:
- Examine the Urethral Opening: During diaper changes, take a moment to check the location of the urethral opening.
- Observe the Urine Stream: Noticing how the urine flows during changes can help identify any abnormal spraying or dribbling.
- Look for Penile Curvature: While slight curves can be normal, significant curvature combined with other symptoms might indicate hypospadias.
If you observe any of these symptoms in your child, consulting a pediatric urologist can provide a thorough evaluation and discuss potential treatment options. Early diagnosis and appropriate treatment can help mitigate complications and improve outcomes.
Causes of Hypospadias
Understanding the causes of hypospadias is essential for medical professionals and expectant parents alike. This condition is influenced by a combination of genetic factors, environmental influences, and hormone imbalances.
Genetic Factors Contributing to Hypospadias
Genetics play a significant role in the development of hypospadias, though no single gene is solely responsible. Instead, a combination of genes contributes to the condition, reflecting a complex inheritance pattern. Here are some genetic factors linked to hypospadias:
- Family History: The risk of hypospadias is higher in infants with a family history of the condition, suggesting a hereditary component.
- Specific Gene Mutations: Mutations in certain genes involved in urogenital development, such as the SRD5A2 gene or the WT1 gene, have been associated with hypospadias.
- Chromosomal Anomalies: Conditions like Klinefelter syndrome (47,XXY) or abnormalities in the sex chromosomes can increase the risk of hypospadias.
Environmental Influences
Environmental factors can also significantly impact the incidence of hypospadias by affecting fetal development. Key environmental influences include:
- Maternal Diet and Health: Poor maternal nutrition, obesity, or diabetes can increase the risk of congenital abnormalities, including hypospadias.
- Exposure to Harmful Substances: Pesticides, certain medications during pregnancy (like anti-epileptic drugs), and other chemicals have been linked to a higher risk of hypospadias in newborns.
- Lifestyle Factors: Smoking or alcohol consumption during pregnancy can adversely affect fetal development and contribute to the occurrence of hypospadias.
The Role of Hormone Imbalances
Hormonal factors are critical in the development of the male reproductive system. Imbalances in these hormones can lead to abnormalities like hypospadias:
- Androgen Function: Hypospadias can result from disruptions in androgen hormones, which are crucial for male genital development. Insufficient hormone levels or the body’s inability to respond to these hormones properly can lead to the condition.
- Endocrine Disruptors: Exposure to endocrine-disrupting chemicals (EDCs) that mimic or interfere with the body’s natural hormones, such as BPA (bisphenol A) or phthalates, is increasingly linked to hypospadias. These chemicals can be found in plastics, cosmetics, and pesticides.
However, the causes of hypospadias are multifactorial, involving a delicate interplay between genetic predispositions, environmental exposures, and hormonal balances. Early diagnosis and understanding the underlying causes are crucial for effective management and treatment of hypospadias.
Diagnosing Hypospadias
Proper diagnosis is crucial for effective treatment and management. Here, we explore the common diagnostic procedures, the roles of healthcare professionals, and the importance of early detection.
Common Diagnostic Procedures
- Physical Examination: The primary method for diagnosing hypospadias is a thorough physical examination of the genitals. This is typically performed by a pediatrician shortly after birth. The doctor will look for the location of the urethral meatus (the opening through which urine exits the body) and assess any associated penile curvature.
- Urine Flow Test: This test may be conducted to observe the stream of urine and determine if there are any abnormalities in the flow that could suggest hypospadias or related issues.
- Ultrasound: In some cases, an ultrasound might be recommended to examine the urinary tract for any abnormalities that are not visible through a physical exam alone.
- Genitourethrogram: This is a specific type of X-ray used to visualize the urethra and bladder, providing detailed images that help in assessing the urethral opening’s location and any associated abnormalities.
Role of Pediatricians and Urologists in Diagnosis
- Pediatricians: They are usually the first to identify potential signs of hypospadias during routine newborn examinations. Pediatricians play a crucial role in the early screening and referral to specialists for further assessment and treatment.
- Urologists: Specialists in the urinary tract and male reproductive organs, urologists are critical in confirming the diagnosis of hypospadias and planning the appropriate treatment. They perform more detailed evaluations and are involved in any surgical procedures that may be required to correct the condition.
Importance of Early Detection
Early detection of hypospadias is essential for several reasons:
- Improves Surgical Outcomes: Early diagnosis allows for timely surgical intervention, typically performed before the child is 18 months old. Surgery at a younger age can reduce complications and improve cosmetic and functional outcomes.
- Reduces Emotional and Psychological Impact: Addressing the condition early can help avoid potential emotional and psychological stress for the child and family as the child grows.
- Prevents Future Complications: Timely treatment prevents complications related to abnormal urination, sexual function, and fertility issues that might arise as the child matures.
However, diagnosing hypospadias involves a combination of clinical evaluation and specialized tests. The roles of pediatricians and urologists are integral in the diagnostic process, emphasizing the importance of early detection for optimal management and treatment outcomes.
Treatment Options for Hypospadias
Hypospadias is a congenital condition affecting males where the urethral opening is not located at the tip of the penis. Treatment is essential not only for urinary functionality but also for sexual health and cosmetic reasons. Here, we explore the necessary treatments for hypospadias, focusing on the optimal timing for intervention, the surgical options available, and the post-surgical care required to ensure the best outcomes.
Overview of Treatment Necessity and Timing
The decision to treat hypospadias is driven by several factors, including the severity of the condition and associated urinary problems. Typically, surgery is recommended to correct hypospadias and is ideally performed when a child is between 6 and 18 months old. This timing helps reduce the psychological and emotional impact of the surgery and takes advantage of the rapid healing capabilities of infants. Early intervention is also thought to improve the cosmetic and functional outcomes of the surgery.
Surgical Options and Outcomes
Surgical correction of hypospadias aims to achieve a functional, straight penis with a cosmetically normal appearance. The type of surgery depends on the severity of the hypospadias. Common procedures include:
- Urethroplasty: This involves reconstructing the urethra to extend it to the tip of the penis. Techniques vary from simple skin flaps to more complex tissue grafts.
- Chordee Correction: If the penis is curved during an erection (a condition known as chordee), this needs to be corrected during surgery to ensure normal function.
- Meatoplasty and Glanuloplasty: These procedures involve reconstructing the meatus (urethral opening) and the glans (the head of the penis), respectively, to improve function and appearance.
The outcomes of these surgeries are generally positive, with high rates of success in terms of both function and appearance. However, complications can occur, such as fistulas (small abnormal connections), strictures (narrowing of the urethra), and the need for further surgery.
Post-Surgical Care and Monitoring
After surgery, careful monitoring is crucial to ensure proper healing and to identify any complications early. Post-surgical care typically includes:
- Pain Management: Appropriate pain relief is provided to keep the child comfortable.
- Wound Care: Instructions are given for cleaning the surgical site to prevent infection and ensure optimal healing.
- Catheter Care: If a catheter is used post-surgery to aid in urination, guidelines are provided for its care and maintenance.
- Activity Restrictions: Limitations on certain activities, such as bathing in tubs or engaging in vigorous play, are advised to avoid stressing the surgical site.
Regular follow-up appointments are essential to assess the surgical site and the child’s urination pattern. These visits also help in the early detection of any issues that might require further intervention.
Through timely and appropriate treatment, children with hypospadias can lead a normal life with excellent functional and cosmetic outcomes. Ensuring adherence to post-surgical care and regular monitoring is key to achieving these results.
Living with Hypospadias
Living with hypospadias can have various impacts on quality of life and mental health, but there are numerous resources available to support patients and their families. Understanding the long-term prognosis and the necessary follow-up care can also help in managing the condition effectively.
Impact on Quality of Life and Mental Health
Hypospadias, a congenital condition where the urethral opening is not located at the tip of the penis, can affect individuals in different ways. Some of the potential impacts on quality of life and mental health include:
- Self-esteem Issues: Children and adults alike may experience feelings of being different, which can affect self-esteem and body image.
- Social Challenges: Concerns about physical appearance and urinary function may lead to social anxiety and avoidance of activities like swimming or sports.
- Sexual Health Concerns: In more severe cases, hypospadias may impact sexual function, which can lead to anxiety and stress about intimate relationships in adulthood.
Support Resources for Parents and Patients
There are several resources and support systems available to help those affected by hypospadias manage the psychological and physical aspects of the condition:
- Medical Support: Regular consultations with urologists who specialize in hypospadias are crucial. They can provide medical advice, treatment options, and reassurance.
- Support Groups: Joining support groups where families share experiences and coping strategies can be immensely beneficial. Organizations such as the Hypospadias and Epispadias Association (HEA) offer resources and community support.
- Counseling Services: Professional counselors or psychologists can help manage any mental health issues related to living with hypospadias, such as low self-esteem or social anxiety.
Long-term Prognosis and Follow-up Care
The long-term prognosis for individuals with hypospadias is generally positive, especially with early treatment:
- Surgical Outcomes: Many children undergo surgery to correct the urethral opening, which typically results in good cosmetic and functional outcomes.
- Follow-Up Care: Regular follow-up appointments are essential to monitor recovery after surgery and to manage any complications. These might include monitoring for urinary tract infections or assessing urinary flow.
- Ongoing Assessment: As the child grows, further assessments may be needed to ensure that the urinary and reproductive systems are functioning well, and additional interventions can be considered if necessary.
However, managing hypospadias involves a combination of medical treatment, psychological support, and community resources. With the right support and care, individuals with hypospadias can lead fulfilling lives.
FAQs about Hypospadias Symptoms
What is hypospadias?
Hypospadias is a congenital condition in males where the opening of the urethra is not located at the tip of the penis. Instead, it is positioned along the underside of the penis, which can vary in severity and location.
What are the common symptoms of hypospadias?
The most noticeable symptom of hypospadias is the misplacement of the urethral opening. Other symptoms may include:
- A downward curve of the penis (chordee)
- A hooded appearance of the penis because the foreskin is not fully developed on the underside
- Difficulty with urination that may spray or require the individual to sit
- A misshapen urinary stream
Can hypospadias cause pain?
Typically, hypospadias does not cause pain on its own. However, associated conditions like chordee may cause discomfort or pain during erections as the child matures.
How is hypospadias detected?
Hypospadias is often detected at birth during the initial physical examination of the newborn. Doctors will observe the placement of the urethral opening and other physical characteristics of the genitals to diagnose this condition.
Does hypospadias affect urination?
Yes, hypospadias can affect the way urine is expelled. The abnormal location of the urethral opening may lead to challenges in directing the urine stream, potentially causing spraying or the need for altered positioning during urination.
Can hypospadias be corrected?
Yes, hypospadias can be corrected with surgery. The procedure typically involves reconstructing the urethra to extend it to the tip of the penis, correcting any penile curvature, and if necessary, modifying the foreskin. This surgery is usually recommended before the child reaches 18 months of age to ensure optimal outcomes both functionally and cosmetically.
Is follow-up necessary after surgery for hypospadias?
Following surgery, regular follow-up appointments are necessary to ensure the success of the repair and monitor for any potential complications. These check-ups also help ensure that urination and future sexual function are normal.
Conclusion
Recognizing the symptoms of hypospadias and understanding its causes is crucial for timely and effective treatment. This congenital condition affects the urethral opening in males and, if identified early, can be corrected with medical interventions that have high success rates.
Symptoms such as an abnormal urethral opening or difficulties with urination are key indicators that should prompt consultation with a healthcare professional.
We encourage parents and guardians to seek medical advice if they suspect hypospadias, as early diagnosis can significantly improve the quality of life for those affected.
Remember, healthcare professionals are your best resource for advice and treatment options tailored to individual needs.
References
For those seeking more detailed information on hypospadias symptoms and to validate the data presented, here are some reputable sources that can be explored further:
- Mayo Clinic – Provides a comprehensive overview of hypospadias, detailing symptoms, causes, and treatment options. Read more at Mayo Clinic’s Hypospadias Resource.
- MedlinePlus – A service of the U.S. National Library of Medicine, this site offers accessible, reliable health information on hypospadias. Explore further at MedlinePlus on Hypospadias.
- Johns Hopkins Medicine – Known for its expertise in pediatric urology, Johns Hopkins provides valuable insights into the diagnosis and management of hypospadias. Visit Johns Hopkins Medicine’s Pediatric Urology Section for more information.
These sources are recognized for their accuracy and thoroughness in medical topics, making them excellent references for understanding hypospadias more deeply.