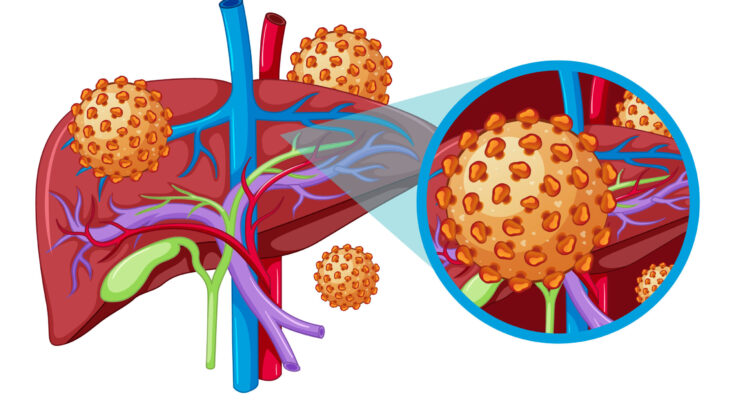
Hepatitis A Symptoms: Hepatitis A is a highly contagious viral infection that primarily affects the liver, leading to a range of health complications from mild symptoms to severe illness.
It is caused by the Hepatitis A virus (HAV) and is mostly transmitted through the ingestion of contaminated food or water.
This comprehensive guide delves into the various symptoms and causes of Hepatitis A, providing essential information to enhance awareness and prevention.
What is Hepatitis A?
Hepatitis A is a highly contagious liver infection caused by the hepatitis A virus (HAV). It is one of several types of hepatitis viruses that include hepatitis B, C, D, and E, each causing different diseases and having different modes of transmission. Unlike hepatitis B and C, which can cause chronic disease, hepatitis A usually provides short-term symptoms and does not lead to chronic liver conditions. Although it can be severe, most people recover completely with no lasting liver damage.
Overview of the Hepatitis A Virus (HAV) and Its Transmission Pathways
The hepatitis A virus is primarily transmitted through the fecal-oral route. This can occur through the consumption of contaminated food or water, or through direct contact with an infectious person. High-risk scenarios include poor hygiene practices, lack of clean water, living in or traveling to areas with high incidence of the virus, and certain sexual practices that involve fecal exposure.
Vaccination against hepatitis A is available and effective, providing an important preventive measure for those at risk. Public health measures that promote good hygiene, proper sanitation, and safe food and water consumption are also critical in controlling the spread of the virus.
However, understanding the dynamics of hepatitis A, its transmission, and prevention can significantly reduce the risk of infection and contribute to better health outcomes.
Key Symptoms of Hepatitis A
Below is a detailed examination of the common symptoms associated with Hepatitis A, the progression of acute symptoms, and an overview of rarer symptoms.
Common Symptoms of Hepatitis A
The most frequent symptoms of Hepatitis A typically appear 2-6 weeks after exposure to the virus. These symptoms are often similar to those of other types of viral hepatitis and can include:
- Jaundice: Yellowing of the skin and the whites of the eyes is one of the most noticeable signs of Hepatitis A.
- Fatigue: Extreme tiredness and a general feeling of unwellness are common.
- Abdominal pain: Particularly pain or discomfort centered in the area of the liver, on the right side of the body just under the lower rib cage.
- Loss of appetite: Often accompanied by weight loss.
- Fever: A mild fever is frequently present.
- Dark urine and pale stool: Changes in urine and stool color can indicate liver issues.
- Nausea and vomiting: These symptoms can further contribute to a loss of appetite and dehydration.
Progression of Acute Symptoms
Hepatitis A symptoms usually develop rapidly and are acute. The initial phase often involves flu-like symptoms, such as fever and body aches, followed by gastrointestinal symptoms like nausea and vomiting. As the disease progresses, jaundice and related symptoms such as itching and pale-colored stools may become more pronounced. For most individuals, symptoms tend to improve within two months of onset, with no lasting liver damage.
Rare Symptoms and Their Manifestation
While the common symptoms of Hepatitis A are well-documented, the virus can occasionally cause more unusual or severe manifestations, including:
- Relapsing Hepatitis: In some cases, patients recover and then experience a recurrence of symptoms a few months later.
- Cholestatic Hepatitis A: This rare form involves severe itching and prolonged jaundice, where the liver struggles to properly process bile.
- Extrahepatic Manifestations: Rarely, Hepatitis A can affect other parts of the body, resulting in conditions such as kidney failure, pancreatitis, or aplastic anemia.
If you suspect you or someone you know might be showing signs of Hepatitis A, consulting a healthcare provider promptly is advised.
Causes and Risk Factors for Hepatitis A
Understanding how the virus is transmitted and identifying the associated risk factors are crucial for prevention and management. This section provides a detailed examination of the transmission methods, significant risk factors, and the role of contaminated food and water in spreading the virus.
Transmission of Hepatitis A
Hepatitis A primarily spreads through the fecal-oral route. This means that the virus is ingested from contact with objects, food, or water contaminated by the feces of an infected person. It is not spread through casual contact or by sneezing or coughing, making direct ingestion of the virus the primary route of transmission. This mode of transmission highlights the importance of proper hygiene and sanitation measures in controlling the spread of the disease.
Risk Factors for Hepatitis A
Several key risk factors increase the likelihood of acquiring hepatitis A:
- Travel to Areas with High Incidence: Travelers to regions where hepatitis A is common are at higher risk, especially if they consume local water or foods that are not properly treated or cooked.
- Poor Sanitation and Hygiene: Individuals living in or visiting areas with poor sanitation practices may be exposed to HAV, particularly if they consume food or water that has not been handled safely.
- Specific Behaviors: Engaging in activities such as eating raw shellfish from contaminated water, sharing drugs and needles, or having close contact with someone infected with HAV can increase the risk.
Role of Contaminated Food and Water
Contaminated food and water are significant vehicles for the spread of hepatitis A. Foods can become contaminated at any point: growing, harvesting, processing, handling, and even after cooking. Common examples include raw or undercooked shellfish from contaminated waters, raw produce, and uncooked foods washed with contaminated water. Additionally, water can be contaminated with the virus if sewage mixes with the water supply.
Preventive measures such as immunization, maintaining high standards of hygiene, and ensuring proper sanitation are critical in combating the spread of hepatitis A. By understanding these transmission paths and risk factors, individuals and health authorities can better prevent the occurrence and spread of hepatitis A, safeguarding public health.
Complications of Hepatitis A: Understanding the Risks
Hepatitis A is an acute viral infection that primarily affects the liver. While many cases are mild and resolve without lasting effects, some individuals may experience complications that can significantly impact their health. Recognizing both short-term complications and the potential long-term risks associated with severe infections is crucial for effective management and prevention.
Short-term Complications and Their Impact on Health
The short-term complications of Hepatitis A, though often temporary, can be severe and include:
- Jaundice: This is characterized by yellowing of the skin and the whites of the eyes. It occurs due to the liver’s reduced ability to process bilirubin, a byproduct of the breakdown of red blood cells.
- Intense Itching: High bilirubin levels can also lead to severe itching, as the substance accumulates in the skin.
- Fatigue: The general feeling of tiredness and weakness is common, as the body directs energy towards fighting the infection and healing the liver.
- Abdominal Pain: Many patients experience discomfort or pain in the abdomen, particularly on the right side where the liver is located.
- Nausea and Vomiting: These symptoms can lead to dehydration, especially if persistent, complicating the recovery process.
- Fever: Although not always present, a fever can accompany the infection as part of the immune response.
These symptoms, while generally resolving as the infection clears, can be extremely debilitating and disrupt daily activities.
Long-term Risks Associated with Severe Infections
In severe cases, Hepatitis A can lead to more significant health issues, including:
- Acute Liver Failure: Although rare, this is a critical condition that can occur if the virus severely damages liver cells more quickly than the body can repair them.
- Relapsing Hepatitis: Some individuals may experience a recurrence of symptoms within six months after the initial infection, leading to further complications.
- Cholestatic Hepatitis: This form of hepatitis is marked by a slow recovery and prolonged jaundice, itching, and fatigue.
These long-term risks highlight the importance of recognizing Hepatitis A infections early and monitoring them closely.
Importance of Medical Intervention in Preventing Complications
Timely medical intervention is essential in managing Hepatitis A and preventing complications. The following strategies are critical:
- Proper Diagnosis: Accurate and prompt diagnosis can help manage symptoms more effectively and monitor the progress of the disease.
- Hydration and Nutrition: Medical guidance on maintaining hydration and proper nutrition can significantly support liver recovery.
- Vaccination: For those at risk, vaccination against Hepatitis A is a highly effective preventive measure.
- Public Health Measures: Ensuring good hygiene practices and adequate sanitation can prevent the spread of the virus.
By understanding the potential complications associated with Hepatitis A and the importance of early medical intervention, individuals and healthcare providers can significantly reduce the impact of the disease. Awareness and preventive care are key in managing the risks associated with this infectious disease.
Diagnosis of Hepatitis A
Diagnosing Hepatitis A is a critical step in managing and preventing the spread of this viral infection, which primarily impacts the liver. The process involves a combination of medical history assessment, physical examinations, and specific diagnostic tests. This comprehensive approach helps healthcare providers confirm the presence of the virus and differentiate it from other types of hepatitis.
List of Diagnostic Tests Used to Confirm Hepatitis A
- Hepatitis A Virus (HAV) IgM Antibody Test: This is the most commonly used test for diagnosing acute Hepatitis A. It detects IgM antibodies, which are produced by the body in response to a Hepatitis A infection. These antibodies typically appear within two weeks of the onset of symptoms and can remain in the blood for up to 6 months.
- Liver Function Tests: While not specific to Hepatitis A, these tests help assess the health of the liver by measuring levels of liver enzymes in the blood. Elevated liver enzymes, such as alanine transaminase (ALT) and aspartate transaminase (AST), can indicate liver inflammation typical of various forms of hepatitis.
- Viral RNA Testing: In some cases, especially in a hospital setting or during an outbreak, viral RNA testing may be conducted using reverse transcription-polymerase chain reaction (RT-PCR) to detect the genetic material of the virus.
These tests provide a reliable confirmation of the Hepatitis A virus and are crucial for accurate diagnosis and management.
The Role of Medical History and Physical Examination in Diagnosis
The initial evaluation of a patient suspected to have Hepatitis A includes a detailed medical history and a thorough physical examination. Here’s how these components play a role in diagnosing the disease:
- Medical History: This includes asking about any recent travel to areas with high Hepatitis A incidence, consumption of contaminated food or water, and close contact with individuals who have Hepatitis A. Knowing if the patient has been vaccinated against Hepatitis A can also guide the diagnostic process.
- Physical Examination: During the physical exam, doctors look for clinical signs of Hepatitis A, such as jaundice (yellowing of the skin and eyes), dark urine, and an enlarged liver. Physical symptoms combined with the patient’s history can lead to a preliminary diagnosis, which is then confirmed through laboratory tests.
However, this thorough approach ensures effective treatment and management of the infection, reducing the risk of complications and transmission.
Treatment Options for Hepatitis A
Here’s a detailed guide on the treatment options available, along with preventive measures to curb the spread of the virus.
List of Treatment Approaches
Hepatitis A treatment primarily focuses on alleviating symptoms and supporting the body’s immune response, as the infection often resolves on its own. Here are the most commonly recommended treatment approaches:
- Supportive Care: Since Hepatitis A is a self-limiting illness for most individuals, supportive care is the mainstay of treatment. This includes managing symptoms and ensuring the body maintains optimal function as it heals.
- Medication for Symptom Relief: Over-the-counter medications may be recommended by healthcare providers to relieve symptoms like fever and pain. However, it’s crucial to avoid any medications that could strain the liver, such as acetaminophen, unless advised by a healthcare professional.
- Monitoring: Regular check-ups are essential to monitor liver function and overall health until symptoms resolve.
Importance of Hydration and Rest
During the recovery phase of Hepatitis A, hydration and rest are paramount. The body needs a lot of energy to fight off the infection and repair liver cells. Ensuring adequate fluid intake helps prevent dehydration caused by symptoms like vomiting and diarrhea. Moreover, resting allows the body to focus its energy on the immune response, speeding up recovery.
Vaccines and Preventive Measures
Prevention is the best strategy against Hepatitis A. Vaccination is highly effective and recommended for:
- All children at age one year.
- Travelers to areas where Hepatitis A is common.
- Individuals with chronic liver disease and other risk factors.
In addition to vaccination, preventive measures play a crucial role in stopping the spread of Hepatitis A. These include:
- Proper Hand Hygiene: Frequent handwashing with soap and water after using the bathroom and before handling food.
- Safe Food Practices: Wash all produce and cook seafood thoroughly.
- Avoiding Contaminated Water: Drink clean, bottled, or boiled water in areas where water sanitation is questionable.
By embracing these treatment and preventive measures, individuals can effectively manage Hepatitis A and mitigate its spread, ensuring better health outcomes for themselves and their communities.
Preventive Measures and Public Health Strategies for Hepatitis A
Hepatitis A is a highly contagious liver infection caused by the hepatitis A virus (HAV). Fortunately, it is preventable through effective strategies focusing on hygiene, vaccination, and public health education. Implementing these measures can significantly reduce the incidence of the disease and prevent outbreaks.
Hygiene Practices to Prevent Hepatitis A
Good personal hygiene is one of the most effective ways to prevent the spread of hepatitis A, especially in regions with higher rates of the disease. The following hygiene practices are recommended:
- Handwashing: Regular and thorough handwashing with soap and water is crucial, especially after using the bathroom, changing diapers, and before preparing or eating food.
- Safe Food and Water: In areas where hepatitis A is common, ensure that water is clean and safe for drinking. Avoid raw or undercooked shellfish. Fruits and vegetables should be washed and peeled before consumption.
- Avoiding Close Contact: Avoid close contact with someone who is infected with the virus. This includes avoiding sharing food, drinks, or utensils.
Hepatitis A Vaccination
Vaccination is the most effective way to prevent hepatitis A infection. The hepatitis A vaccine is safe and highly effective in providing long-lasting protection. Here are key points about the vaccination:
- Who Should Get Vaccinated: Vaccination is recommended for all children aged one year and older, travelers to areas with high rates of hepatitis A, men who have sex with men, drug users, people with chronic liver disease, and those who are at increased risk of exposure.
- Vaccine Schedule: The hepatitis A vaccine is typically given in two shots, six months apart. It can be integrated into the routine childhood vaccination schedule.
- Long-Term Protection: The vaccine provides long-term protection, potentially lasting 20 years or more.
Public Health Campaigns and Education
Public health campaigns and education play a crucial role in reducing the spread of hepatitis A. Effective public health strategies include:
- Awareness Campaigns: Raising awareness about hepatitis A transmission and prevention through media campaigns, community workshops, and school programs.
- Screening and Surveillance: Implementing robust screening and surveillance programs to quickly identify and respond to hepatitis A cases.
- Resource Allocation: Ensuring that adequate resources are allocated for vaccine provision, especially in underserved communities.
- International Cooperation: Collaborating with international health organizations to improve hygiene and healthcare access in regions where hepatitis A is prevalent.
By adopting these strategies, communities can significantly reduce the incidence of hepatitis A and protect public health. Public health officials continue to play a vital role in educating the public and implementing preventive strategies effectively.
FAQs about Hepatitis A Symptoms
What are the first signs of Hepatitis A?
The initial symptoms of Hepatitis A can be mild and include fatigue, nausea, abdominal pain, especially around the liver area, and a loss of appetite. These symptoms typically appear 2-6 weeks after exposure to the Hepatitis A virus.
Can Hepatitis A symptoms appear suddenly?
Yes, symptoms of Hepatitis A can appear suddenly and may include jaundice (yellowing of the skin and eyes), dark urine, and pale stool. These symptoms occur as the virus affects liver function.
How long do Hepatitis A symptoms last?
Symptoms of Hepatitis A usually last less than 2 months, although some people can feel ill for as long as 6 months. Most individuals recover without any permanent liver damage.
Are Hepatitis A symptoms different in children?
Yes, children under the age of 6 often have either no symptoms or very mild symptoms. Older children and adults are more likely to develop more noticeable symptoms, including jaundice.
What should I do if I experience symptoms of Hepatitis A?
If you suspect you have symptoms of Hepatitis A, seek medical advice promptly. Early diagnosis and supportive care are important for recovery. Avoiding alcohol and not taking unnecessary medications can help prevent further liver damage.
Can Hepatitis A symptoms be treated at home?
While there is no specific treatment for Hepatitis A, managing symptoms is crucial. This includes adequate hydration, rest, and eating a balanced diet. However, medical supervision is recommended to monitor the progress of the illness and manage any complications.
When should I see a doctor for Hepatitis A symptoms?
You should consult a healthcare provider if you develop symptoms such as jaundice, severe abdominal pain, prolonged nausea, or any signs of dehydration. Early medical intervention can help manage symptoms effectively and prevent serious complications.
Conclusion
In this article, we explored the essential symptoms and causes of Hepatitis A, a highly contagious liver infection caused by the Hepatitis A virus. Key symptoms include jaundice, fatigue, abdominal pain, loss of appetite, and nausea, among others. The virus primarily spreads through the ingestion of contaminated food or water and close contact with an infected person.
For those at higher risk, including travelers to areas with high Hepatitis A incidence and individuals in close contact with the infected, vaccination is the most effective way to prevent the disease. Additionally, maintaining good hygiene practices, such as thorough handwashing with soap and water, is critical in controlling the spread of the virus.
We strongly encourage at-risk individuals to consult healthcare providers about getting vaccinated and to adhere to preventive measures. Taking these steps will significantly reduce the risk of contracting Hepatitis A and ensure better health and well-being.
References
For those seeking more detailed information or verification of the content covered on the symptoms of Hepatitis A, we recommend consulting the following reputable sources:
- Centers for Disease Control and Prevention (CDC) – This site provides comprehensive information on Hepatitis A, including symptoms, transmission, prevention, and treatment options. Read more about Hepatitis A on the CDC website.
- World Health Organization (WHO) – WHO offers global perspectives and data on Hepatitis A. Their resources include prevention strategies, outbreak monitoring, and vaccination guidelines. Visit WHO’s Hepatitis A resource page.
- Mayo Clinic – A trusted source for health information, the Mayo Clinic provides detailed descriptions of the symptoms of Hepatitis A, diagnosis methods, and management of the disease. Learn more about Hepatitis A at Mayo Clinic.
- MedlinePlus – MedlinePlus offers accessible medical information in both English and Spanish, supported by the National Institute of Health. Their Hepatitis A section covers all aspects of the condition, including symptoms, testing, and risk factors. Explore Hepatitis A on MedlinePlus.
These resources are authoritative and provide reliable information for anyone looking to understand more about Hepatitis A, its symptoms, and overall impact on health.