Thyroid Disease Treatment: The thyroid may be a small, butterfly-shaped gland at the base of your neck, but its importance is enormous. Acting like your body’s thermostat, the thyroid controls how your body uses energy, influences your heart rate, body temperature, and even mood. When it’s working properly, you barely notice it. But when it’s out of balance, the effects can be widespread and significant. Thyroid disease can disrupt every aspect of your health—from how you feel day-to-day to your long-term wellbeing.
Thyroid disorders are among the most common endocrine problems in the world. Despite being so widespread, they’re often misdiagnosed or misunderstood. Why? Because the symptoms can be subtle, develop slowly, or mimic other conditions. That’s why a proper diagnosis and tailored treatment plan are essential for managing thyroid disease effectively.
In this article, we’ll walk through everything you need to know—from understanding thyroid function, causes of disease, diagnostic methods, to treatment options and lifestyle adjustments. Whether you suspect you might have a thyroid problem or you’re supporting someone who does, you’ll find valuable insights to help you navigate this condition with clarity and confidence.
Understanding Thyroid Disease
When we talk about thyroid disease, we’re not referring to just one condition. It’s a broad term that includes a variety of issues affecting how the thyroid gland functions. The two most common types are:
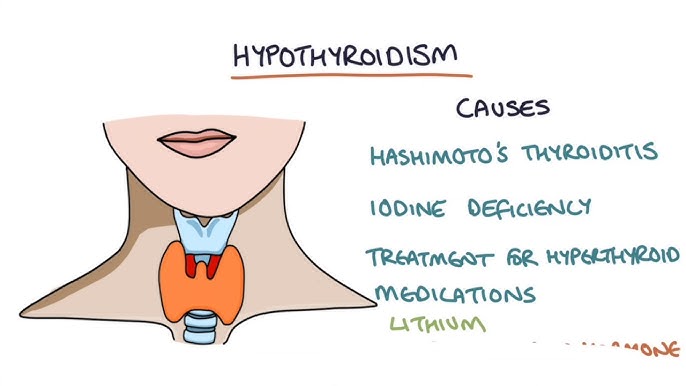
- Hypothyroidism: The thyroid doesn’t produce enough hormones.
- Hyperthyroidism: The thyroid produces too many hormones.
But there are other conditions as well, like thyroid nodules, goiter (enlarged thyroid), thyroiditis (inflammation of the thyroid), and thyroid cancer.
Thyroid disease can affect people of all ages, but it’s especially common in women—particularly those over 30. In fact, women are up to 8 times more likely than men to develop a thyroid disorder. In developing countries, iodine deficiency remains a major cause, while in developed nations, autoimmune diseases like Hashimoto’s thyroiditis and Graves’ disease are the primary culprits.
Millions of people live with undiagnosed thyroid problems, simply because symptoms are attributed to stress, aging, or other medical conditions. That’s why awareness, early detection, and accurate diagnosis are key to reducing the impact of thyroid disease on quality of life.
Functions of the Thyroid Gland
So, what exactly does the thyroid gland do? This little powerhouse produces hormones—primarily thyroxine (T4) and triiodothyronine (T3)—that regulate the body’s metabolism. These hormones control how fast your heart beats, how deep you breathe, how you burn calories, and even how your brain functions.
Here’s how the process works: the pituitary gland in the brain releases thyroid-stimulating hormone (TSH), which tells the thyroid how much hormone to produce. This feedback loop ensures your body maintains hormonal balance.
Key functions of thyroid hormones include:
- Regulating metabolic rate (affects body weight)
- Controlling heart rate and blood pressure
- Supporting digestive function
- Regulating body temperature
- Aiding brain development in infants and children
- Balancing mood and mental health
When hormone levels are out of whack—either too high or too low—you begin to feel the effects throughout your entire body.
Causes of Thyroid Disease
Thyroid disease can stem from a wide variety of causes, some genetic, some environmental, and others related to lifestyle or autoimmune responses. Understanding the root cause is essential for choosing the right treatment and managing the condition effectively.
Let’s break down the primary causes:
1. Autoimmune Disorders
This is one of the most common causes, especially in developed countries. Autoimmune diseases occur when the immune system mistakenly attacks the body’s own tissues. In the case of thyroid disease:
- Hashimoto’s Thyroiditis leads to hypothyroidism. The immune system damages the thyroid, reducing its ability to produce hormones.
- Graves’ Disease causes hyperthyroidism. The immune system stimulates the thyroid to overproduce hormones.
Both conditions can run in families, indicating a strong genetic component.
2. Iodine Deficiency or Excess
The thyroid uses iodine to produce T3 and T4. If your diet lacks sufficient iodine (common in some parts of Asia and Africa), the thyroid can’t function properly, often leading to goiter or hypothyroidism. Conversely, too much iodine can also trigger thyroid problems, especially in people with pre-existing thyroid conditions.
3. Hormonal Changes
Life stages like puberty, pregnancy, postpartum, and menopause can affect thyroid function, particularly in women. Many women experience thyroid dysfunction during or after pregnancy, which may or may not resolve on its own.
4. Genetic Predisposition
If your parents or siblings have thyroid disease, your risk is higher. Specific gene mutations are also being studied that may make some people more susceptible to autoimmune thyroid conditions.
5. Radiation Exposure
Exposure to radiation—either environmental or from previous treatments for cancers in the neck or chest—can damage the thyroid and lead to conditions including thyroid cancer.
6. Certain Medications
Drugs like lithium (used in bipolar disorder), interferon, and amiodarone can negatively affect thyroid hormone production. Always inform your doctor of any long-term medications you’re on.
Understanding the underlying cause of thyroid disease allows healthcare providers to personalize your treatment plan, improve outcomes, and minimize complications.
Symptoms of Thyroid Disorders
Thyroid disease symptoms vary widely depending on whether the condition is causing hormone levels to be too high (hyperthyroidism) or too low (hypothyroidism). However, many symptoms overlap with other conditions, which is why thyroid problems often go undiagnosed for long periods.
Hypothyroidism Symptoms (Underactive Thyroid)
When the thyroid produces too little hormone, your body’s processes slow down. Common signs include:
- Fatigue and sluggishness
- Unexplained weight gain
- Cold intolerance
- Dry skin and brittle hair
- Depression or mood swings
- Constipation
- Puffy face
- Memory problems or “brain fog”
- Slow heart rate
- Menstrual irregularities
If left untreated, severe hypothyroidism can lead to myxedema, a rare but life-threatening condition requiring emergency medical care.
Hyperthyroidism Symptoms (Overactive Thyroid)
In this case, the thyroid produces too much hormone, accelerating your body’s functions. Symptoms may include:
- Rapid heartbeat or palpitations
- Anxiety, irritability, or restlessness
- Sudden weight loss despite normal appetite
- Heat intolerance and excessive sweating
- Tremors (especially in the hands)
- Insomnia
- Frequent bowel movements
- Thinning skin or hair
- Bulging eyes (in Graves’ disease)
Other Symptoms & Complications
Thyroid nodules or goiter may present as visible swelling in the neck. In rare cases, thyroid cancer may not cause symptoms until it’s advanced. Long-term untreated thyroid conditions can lead to infertility, heart disease, osteoporosis, and developmental delays in children.
Since the symptoms can be subtle or overlap with other health issues, early diagnosis through blood tests and clinical evaluation is essential.
Risk Factors for Developing Thyroid Problems
Understanding your personal risk factors can help you stay vigilant and potentially catch thyroid issues early. While anyone can develop thyroid disease, certain factors significantly raise your chances:
1. Gender and Age
Women are far more likely than men to develop thyroid disorders, especially during hormonal transitions like pregnancy or menopause. The risk increases after the age of 30 and peaks between ages 40–60.
2. Family History
A family history of thyroid disease—particularly autoimmune thyroid disease like Graves’ or Hashimoto’s—raises your risk substantially.
3. Iodine Intake
Living in a region with iodine-deficient soil or consuming a diet low in iodine can increase your chances of developing hypothyroidism or goiter. On the flip side, excessive iodine from supplements or medications can worsen thyroid function in those predisposed to autoimmune disease.
4. Preexisting Medical Conditions
People with other autoimmune diseases (such as type 1 diabetes, celiac disease, rheumatoid arthritis, or lupus) are more prone to thyroid issues.
5. Medications
As mentioned, drugs like lithium or amiodarone can affect thyroid hormone levels. Cancer treatments like radiation to the neck or chemotherapy also increase the risk.
6. Pregnancy and Postpartum Period
Women often develop temporary thyroiditis after giving birth. Sometimes it progresses to permanent hypothyroidism.
Being aware of these risk factors can prompt earlier testing and intervention, preventing the condition from worsening or causing long-term complications.
How Thyroid Disease is Diagnosed
Diagnosing thyroid disease involves a combination of symptom assessment, physical examination, blood tests, and imaging. Early and accurate diagnosis is key to preventing serious complications.
1. Clinical Evaluation
Your healthcare provider will first review your symptoms, medical history, and conduct a physical exam. They may feel your neck for thyroid enlargement (goiter) or nodules.
2. Blood Tests
These are the gold standard for diagnosing thyroid problems. Key tests include:
- TSH (Thyroid Stimulating Hormone): High TSH indicates hypothyroidism; low TSH suggests hyperthyroidism.
- Free T4 (Thyroxine): Shows the amount of active thyroid hormone in your blood.
- Free T3 (Triiodothyronine): Especially useful in diagnosing hyperthyroidism.
- Thyroid Antibodies: Used to detect autoimmune thyroid diseases like Hashimoto’s and Graves’.
3. Imaging Tests
- Ultrasound: Helps detect nodules, cysts, or enlargement.
- Radioactive Iodine Uptake Test (RAIU): Shows how much iodine the thyroid absorbs, helping diagnose hyperthyroidism.
- Thyroid Scan: Highlights the shape, size, and position of the gland.
4. Fine Needle Aspiration Biopsy (FNA)
If you have a suspicious lump or nodule, a biopsy may be done to rule out cancer. This involves using a thin needle to extract cells for microscopic examination.
With the right combination of tests, doctors can accurately diagnose the type and severity of thyroid disease and create a targeted treatment plan.
Interpreting Thyroid Test Results
Once you’ve had your thyroid tested, understanding what those numbers mean is the next important step. Your test results give your doctor a snapshot of how well your thyroid is functioning. But for the average person, those numbers—TSH, T3, T4—can look like confusing code. So, let’s break it down in simple terms.
TSH (Thyroid Stimulating Hormone)
TSH is produced by the pituitary gland and is one of the first markers checked. It tells your thyroid how much hormone to make.
- High TSH: Your thyroid isn’t making enough hormones (hypothyroidism).
- Low TSH: Your thyroid is making too much hormone (hyperthyroidism).
A normal range is generally between 0.4 and 4.0 mIU/L, but this can vary slightly depending on the lab.
Free T4 (Thyroxine) and Free T3 (Triiodothyronine)
- Low Free T4 and/or T3 with high TSH: Indicates primary hypothyroidism.
- High Free T4 and/or T3 with low TSH: Suggests hyperthyroidism.
- Normal T3/T4 but abnormal TSH: May indicate early or subclinical thyroid disease.
Thyroid Antibody Tests
These help confirm autoimmune thyroid diseases:
- TPO antibodies (thyroid peroxidase): High in Hashimoto’s disease.
- TSI antibodies (thyroid-stimulating immunoglobulin): High in Graves’ disease.
Other Factors That Influence Results
- Pregnancy
- Medications (like steroids, birth control, or biotin supplements)
- Severe illness
- Time of day the blood was drawn
Proper interpretation should always be done by a healthcare provider who will also consider your symptoms and overall health—not just lab values. Sometimes, repeated testing over time is necessary to get a clearer picture of your thyroid function.
Treatment Options for Thyroid Disorders
Treatment for thyroid disease depends on the type and severity of the disorder. Some conditions, like mild subclinical hypothyroidism, may not need treatment right away. Others, like overt hyperthyroidism or thyroid cancer, require more aggressive interventions.
Let’s explore the main treatment approaches:
1. Lifestyle Modifications
While not a standalone solution, lifestyle changes support thyroid health and improve overall well-being:
- Eating a balanced diet with sufficient iodine, selenium, and zinc
- Managing stress through mindfulness or therapy
- Getting enough sleep
- Exercising regularly to boost metabolism and energy levels
2. Medication-Based Treatment
Most thyroid conditions are managed with medications:
- Hypothyroidism: Treated with synthetic thyroid hormone (levothyroxine).
- Hyperthyroidism: Treated with antithyroid drugs (like methimazole or propylthiouracil) that reduce hormone production.
We’ll go deeper into these medications in the next section.
3. Radioactive Iodine Therapy
Used to treat hyperthyroidism and some forms of thyroid cancer. This therapy destroys overactive thyroid tissue.
4. Surgery
In certain cases, part or all of the thyroid must be removed. This might be necessary if you have:
- Thyroid cancer
- Large goiter causing breathing/swallowing issues
- Hyperthyroidism unresponsive to medications
After surgery, patients usually need lifelong hormone replacement therapy.
5. Watchful Waiting
In cases where nodules are benign or hormone levels are borderline, doctors may monitor the condition over time before starting any treatment.
Each treatment path is personalized based on age, severity, underlying cause, pregnancy status, and overall health. The goal is always to restore hormone balance, relieve symptoms, and prevent complications.
Medications Used in Thyroid Treatment
Medications play a central role in managing both hypo- and hyperthyroidism. Let’s take a closer look at how these drugs work and what to expect.
1. Levothyroxine (Synthroid, Euthyrox, etc.)
This is the standard treatment for hypothyroidism. It’s a synthetic form of thyroxine (T4) and is usually taken once a day on an empty stomach.
Key Points:
- Dosage is based on age, weight, severity of hypothyroidism, and other health conditions.
- Regular blood tests are needed to adjust the dose.
- Most people need to take it for life.
- It has minimal side effects when dosed correctly.
Missed doses or improper absorption (from taking it with food or other medications) can affect its effectiveness, so consistency is key.
2. Antithyroid Medications (Methimazole, Propylthiouracil)
Used primarily for hyperthyroidism, these medications reduce the amount of thyroid hormone the gland produces.
Methimazole:
- Commonly used due to its effectiveness and fewer side effects.
- Often prescribed for Graves’ disease.
Propylthiouracil (PTU):
- Used less frequently but preferred during the first trimester of pregnancy.
Side effects may include rash, liver inflammation, or reduced white blood cells—so regular blood monitoring is required.
3. Beta-Blockers (Propranolol, Atenolol)
These aren’t thyroid-specific drugs, but they help manage symptoms of hyperthyroidism, like fast heart rate, anxiety, and tremors.
4. Calcium and Vitamin D Supplements
If thyroid removal or prolonged hyperthyroidism affects bone health, supplements may be prescribed to prevent osteoporosis.
Always follow your doctor’s instructions and never adjust your dosage without consultation. Proper medication use is the cornerstone of successful thyroid disease management.
Radioactive Iodine Therapy
Radioactive iodine therapy (RAI) is a targeted treatment that has been used for decades to effectively treat overactive thyroid tissue. It’s most commonly recommended for Graves’ disease, toxic nodular goiter, and in some cases, thyroid cancer.
How It Works
You take radioactive iodine (I-131) orally, usually in capsule or liquid form. The thyroid gland naturally absorbs iodine, so the radioactive iodine gets concentrated in thyroid cells and destroys them over time.
This gradually reduces thyroid hormone production without affecting other organs.
Benefits:
- Non-invasive and painless
- No surgical risk
- Highly effective in 70–90% of cases
Possible Side Effects:
- Neck tenderness or swelling
- Dry mouth or taste changes
- Temporary worsening of hyperthyroid symptoms
- Long-term hypothyroidism (requiring levothyroxine therapy)
Precautions After Treatment:
- Limited contact with others (especially children and pregnant women) for several days due to radiation
- Follow specific safety guidelines provided by your doctor
RAI is a convenient alternative to surgery and usually offers permanent results. However, it’s not recommended for pregnant or breastfeeding women, and it may take several months to see full effects.
Surgical Treatment for Thyroid Disease
While not the first line of treatment for most thyroid conditions, surgery becomes necessary in specific situations. It’s often used when other treatments fail or aren’t appropriate, particularly in cases involving large goiters, suspicious nodules, or thyroid cancer.
When is Thyroid Surgery Recommended?
Surgery may be the best option in the following scenarios:
- Thyroid cancer diagnosis or suspicion
- Large goiters that cause difficulty breathing or swallowing
- Hyperthyroidism not responsive to medication or radioactive iodine
- Presence of benign nodules that continue to grow
- Cosmetic concerns due to thyroid enlargement
Types of Thyroid Surgery
There are a few surgical options depending on the condition and severity:
- Lobectomy: Only one lobe of the thyroid is removed. Often used for small nodules.
- Subtotal thyroidectomy: Removes a large portion of the thyroid but not all of it.
- Total thyroidectomy: Removes the entire gland—typically used for cancer cases or diffuse goiter.
Recovery and Aftercare
Thyroid surgery is generally safe, but like any surgery, it comes with risks, including:
- Hoarseness or voice changes (due to nerve damage)
- Low calcium levels (from parathyroid gland disruption)
- Bleeding or infection (rare)
Recovery typically involves a short hospital stay, followed by several weeks of rest at home. If your entire thyroid is removed, you’ll need lifelong hormone replacement therapy with levothyroxine.
Routine follow-ups and blood tests are crucial post-surgery to ensure your hormone levels remain stable and to check for any signs of recurrence, especially in cancer cases.
Managing Thyroid Disorders During Pregnancy
Thyroid hormones are essential for fetal development—especially brain and nervous system development in the first trimester. That’s why untreated thyroid disease during pregnancy can lead to serious complications for both mother and baby.
Hypothyroidism in Pregnancy
If left untreated, hypothyroidism increases the risk of:
- Miscarriage
- Preterm birth
- Low birth weight
- Developmental delays in the baby
Treatment: Levothyroxine is safe during pregnancy and must be adjusted frequently, as hormone demands increase significantly during gestation.
Hyperthyroidism in Pregnancy
Uncontrolled hyperthyroidism can cause:
- Preeclampsia (high blood pressure)
- Congestive heart failure
- Low birth weight or stillbirth
Treatment: Propylthiouracil (PTU) is preferred in the first trimester, and methimazole may be used afterward. RAI therapy is not safe during pregnancy.
Monitoring
Pregnant women with known thyroid disease require:
- Monthly thyroid function tests
- Frequent medication adjustments
- Collaboration between an endocrinologist and obstetrician
Early detection and careful management ensure a healthier pregnancy outcome. If you’re planning to conceive and have a thyroid condition, talk to your doctor beforehand to stabilize your hormone levels.
Long-Term Management and Monitoring
Thyroid disease isn’t always a “one-and-done” type of diagnosis. For many, it’s a chronic condition requiring ongoing care and periodic adjustments. The good news? With proper monitoring, people with thyroid disorders can live long, healthy lives.
Why Long-Term Monitoring Matters
Thyroid hormone needs can change due to:
- Age
- Weight fluctuations
- New medications
- Pregnancy or menopause
- Surgery or other health conditions
Even if your symptoms are stable, regular testing ensures you remain in the optimal range.
Recommended Monitoring Schedule
- Newly diagnosed patients: Blood tests every 6–8 weeks until levels stabilize.
- Stable patients: Tests every 6–12 months, or as advised.
- After surgery or RAI: More frequent tests during the first year.
Signs You May Need a Dose Adjustment
- Feeling more tired than usual
- Weight gain or loss without changes in diet
- Mood changes or depression
- Heart palpitations or anxiety
- Menstrual changes
Keeping a symptom journal and checking in with your doctor regularly helps fine-tune your treatment plan. Many people make the mistake of thinking they can stop taking medication once they feel better—but thyroid replacement therapy is typically lifelong.
Living with Thyroid Disease
Being diagnosed with thyroid disease can feel overwhelming, but it doesn’t have to take over your life. With the right treatment, lifestyle habits, and support, most people manage the condition effectively and thrive.
1. Diet and Nutrition
A nutrient-rich diet supports overall thyroid health. Focus on:
- Iodine: Found in iodized salt, dairy, and seafood
- Selenium: Brazil nuts, sunflower seeds, and tuna
- Zinc: Meat, shellfish, and legumes
- Vitamin D and calcium: Important for bone health, especially in hyperthyroidism
Foods to limit:
- Soy and cruciferous vegetables (like broccoli and cabbage) in excess—they can interfere with hormone absorption.
- Processed foods and sugar, which can worsen fatigue and inflammation.
2. Mental Health
Many people with thyroid issues experience mood swings, anxiety, or depression. These aren’t just emotional responses to being sick—they’re biochemical. Hormones heavily influence brain function.
Consider therapy, mindfulness practices, and connecting with support groups to help maintain emotional balance.
3. Exercise and Lifestyle
Moderate exercise improves energy levels, sleep, and mood. Walking, swimming, and yoga are great low-impact options.
Also:
- Get 7–9 hours of sleep nightly
- Avoid unnecessary stress
- Take medications consistently
- Stick to follow-up appointments
Living with thyroid disease is like learning a new rhythm—it takes time, but once you’re in sync, you can dance to it just fine.
Preventive Measures and Early Detection
While not all thyroid diseases are preventable, early detection can significantly reduce complications. Routine checkups and awareness of risk factors make a huge difference.
What You Can Do:
- Get screened if you have a family history or symptoms
- Eat a balanced diet rich in iodine and selenium
- Avoid smoking, which disrupts thyroid function
- Be mindful of environmental toxins (like perchlorate and BPA)
- Manage stress levels, as chronic stress can exacerbate autoimmune reactions
Annual physical exams that include basic thyroid checks (like feeling for enlargement) and TSH testing can detect issues before symptoms appear. Especially for women over 30, postpartum women, or anyone with autoimmune conditions, regular thyroid evaluation should be a priority.
Innovations and Research in Thyroid Disease
The field of thyroid research is evolving rapidly, offering hope for more accurate diagnostics, personalized therapies, and possibly even a cure in the future.
What’s New:
- Genetic testing for risk profiling
- Improved imaging techniques for thyroid nodules and cancer
- Targeted therapies for aggressive thyroid cancers
- Advancements in bioengineered thyroid tissue for transplant research
- New formulations of levothyroxine (like liquid or softgel) for better absorption
As more is understood about the immune system and the microbiome’s role in autoimmune diseases, there’s increasing potential for preventing and reversing certain types of thyroid disease.
Clinical trials are ongoing for new antithyroid drugs, immunomodulators, and therapies aimed at rebalancing the immune system rather than just treating symptoms.
Stay informed and always ask your healthcare provider about the latest treatment options or clinical trials you might qualify for.
FAQs about Thyroid Disease Treatment
1. Can thyroid disease be cured permanently?
Some forms, like temporary thyroiditis, may resolve on their own. However, most thyroid conditions (especially autoimmune types) require long-term management, not a permanent cure.
2. How often should I check my thyroid levels?
It depends on your condition. Stable patients may test every 6–12 months, while those adjusting medications may need tests every 6–8 weeks.
3. Does thyroid disease affect weight?
Yes. Hypothyroidism often leads to weight gain, while hyperthyroidism may cause weight loss. However, other factors also play a role.
4. Is thyroid disease hereditary?
Yes, especially autoimmune thyroid disorders. If you have a family history, your risk increases significantly.
5. Can diet alone manage thyroid conditions?
Diet supports thyroid health but is not a substitute for medication in most cases. Always consult your doctor before stopping or starting any treatment.
Conclusion
Thyroid disease can be complex, but it’s far from unmanageable. With accurate diagnosis, personalized treatment, and ongoing monitoring, you can live a full and vibrant life. The key lies in understanding the condition, knowing your body, and partnering with your healthcare provider to make informed decisions.
Whether you’re newly diagnosed or have been managing thyroid issues for years, remember: you’re not alone, and help is always available. Stay informed, stay proactive, and give your thyroid the attention it deserves.