Graves’ Disease Treatment: Graves’ disease is an autoimmune disorder that is the most common cause of hyperthyroidism, where the thyroid gland produces excessive hormones.
It significantly impacts various bodily functions and can lead to severe health complications if not properly managed.
Understanding Graves’ Disease
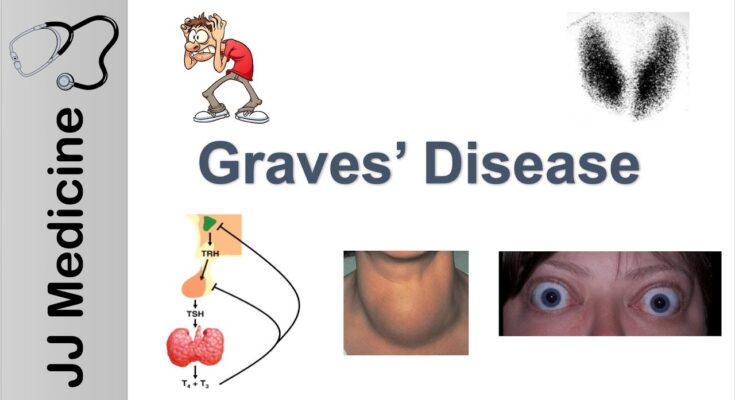
Graves’ Disease is an autoimmune disorder that primarily affects the thyroid gland, causing it to become overactive, a condition known as hyperthyroidism. This disease leads the thyroid gland to produce excess thyroid hormones, which can accelerate the body’s metabolism, affecting various bodily functions. Understanding Graves’ Disease is crucial because it not only impacts physical health but also emotional and psychological well-being.
Symptoms of Graves’ Disease
The symptoms of Graves’ Disease can be diverse and affect multiple body systems. Common signs include:
- Increased Heart Rate: Patients may experience palpitations or an unusually fast heartbeat.
- Weight Loss: Unexpected weight loss, even when eating habits haven’t changed.
- Tremors: Fine shaking, particularly in the hands.
- Increased Sensitivity to Heat: Feeling overheated in environments that others find comfortable.
- Sweating: Excessive perspiration is common.
- Changes in Menstrual Cycles: Women may notice lighter or less frequent periods.
- Erectile Dysfunction and Reduced Libido: Sexual health issues can occur in men.
- Anxiety and Irritability: Mood swings and nervousness are prevalent.
- Fatigue: Despite high energy levels at times, fatigue can occur due to disrupted sleep.
- Enlarged Thyroid Gland: Also known as a goiter, which may be visible as a bulge at the base of the neck.
- Eye Issues: Such as bulging eyes, dry or irritated eyes, and vision problems.
Recognizing these symptoms early can lead to a quicker diagnosis and improved management of the disease.
Causes and Risk Factors of Graves’ Disease
Graves’ Disease is caused by a malfunction in the immune system. The body’s defense system mistakenly attacks the thyroid gland, causing it to overproduce hormones. Several factors can increase the risk of developing Graves’ Disease:
- Genetic Predisposition: A family history of the disease significantly raises the risk.
- Gender: Women are more likely to develop Graves’ Disease than men.
- Age: It most commonly affects people between the ages of 30 and 50.
- Other Autoimmune Disorders: Having another autoimmune disorder, such as type 1 diabetes or rheumatoid arthritis, can increase risk.
- Stress: Emotional or physical stress can trigger the onset of the disease.
- Pregnancy: Hormonal changes during pregnancy can contribute to the development of Graves’ Disease.
- Smoking: Tobacco use can affect the immune system and has been linked specifically to Graves’ eye disease, a related condition.
However, understanding these causes and risk factors can help individuals assess their risk and seek medical advice if they exhibit symptoms of Graves’ Disease. Early intervention and treatment can effectively manage symptoms and improve quality of life.
Diagnosis of Graves’ Disease
Initial Assessment and Symptoms to Watch For
Graves’ disease is an autoimmune disorder that primarily affects the thyroid gland, leading to hyperthyroidism. Early diagnosis is crucial for effective management. The initial assessment starts with recognizing the hallmark symptoms to watch for. Common symptoms include:
- Increased heart rate: Often described as palpitations.
- Weight loss: Occurs despite normal or increased appetite.
- Heat intolerance: Along with excessive sweating.
- Tremors: Especially noticeable in the hands.
- Mood changes: Such as irritability and anxiety.
- Fatigue: Despite seeming overactive, individuals may experience unexplained tiredness.
- Eye issues: Including bulging eyes (exophthalmos), which is one of the most distinctive signs.
If you or someone you know exhibits these symptoms, consulting a healthcare professional is advisable for a thorough assessment.
Diagnostic Tests for Graves’ Disease
To confirm a diagnosis of Graves’ disease and assess the extent of thyroid dysfunction, several diagnostic tests are typically conducted:
- Blood Tests: These are fundamental in diagnosing Graves’ disease. They measure levels of thyroid hormones — free thyroxine (T4) and triiodothyronine (T3) — and thyroid-stimulating hormone (TSH). In Graves’ disease, T4 and T3 levels are often elevated while TSH levels are suppressed due to the negative feedback mechanism.
- Thyroid Scan and Uptake: This involves ingesting a radioactive iodine isotope and then scanning the thyroid gland. A high uptake of radioactive iodine indicates that the thyroid gland is overactive, a common sign of Graves’ disease.
- Thyroid-Stimulating Immunoglobulin (TSI) Tests: These tests detect the presence of specific antibodies typical in Graves’ disease, helping further confirm the diagnosis.
Role of Healthcare Professionals in the Diagnosis of Graves’ Disease
The diagnosis of Graves’ disease is a multidisciplinary effort, involving a range of healthcare professionals:
- Primary Care Physicians typically conduct the initial evaluation based on symptoms and medical history.
- Endocrinologists specialize in hormonal diseases and play a crucial role in both the diagnosis and management of the condition.
- Radiologists are essential for conducting and interpreting thyroid scans.
- Immunologists may be involved in cases where distinguishing between different autoimmune disorders is challenging.
The collaboration among these professionals ensures a comprehensive evaluation, accurate diagnosis, and the initiation of an appropriate treatment plan. Prompt and accurate diagnosis is essential to manage the symptoms effectively and prevent complications such as thyroid storm, a potentially life-threatening condition.
By understanding the symptoms, available diagnostic tests, and the importance of professional healthcare intervention, individuals can seek timely medical advice, leading to better health outcomes in managing Graves’ disease.
Treatment Options for Graves’ Disease
Here, we’ll explore the various treatment options, their mechanisms, effectiveness, and considerations to help those affected make informed decisions.
Medications for Graves’ Disease
1. Anti-thyroid Medications: Commonly prescribed anti-thyroid drugs include Methimazole and Propylthiouracil (PTU). These medications help reduce the production of thyroid hormones.
- How They Work: Anti-thyroid medications inhibit the thyroid’s ability to synthesize hormones.
- Potential Side Effects: Side effects may include rash, joint pain, liver failure, or a decrease in white blood cells, which can lead to an increased risk of infection.
2. Beta Blockers: Drugs like Propranolol are used to alleviate the symptoms without affecting the thyroid hormone levels.
- How They Work: Beta blockers block the action of adrenaline and other similar compounds, reducing heart rate and blood pressure, thereby easing symptoms such as anxiety, rapid pulse, and tremors.
- Potential Side Effects: Common side effects include fatigue, cold hands and feet, and sleep disturbances.
Radioactive Iodine Therapy
This form of treatment involves ingesting radioactive iodine-131, which destroys the overactive thyroid cells.
- Process and Effectiveness: The radioactive iodine is taken orally and specifically targets thyroid cells, effectively decreasing the thyroid’s hormone production. This treatment has a high success rate, often curing hyperthyroidism with a single dose.
- Safety and Long-term Considerations: While considered safe, this therapy may lead to hypothyroidism, requiring lifelong thyroid hormone replacement. It is not recommended for pregnant women or those breastfeeding.
Surgical Treatments
Surgery may be considered in cases where medications are not effective, or when there is a significant goiter causing physical discomfort or cosmetic concerns.
1. When Surgery is Necessary: Indications for surgery include resistance to medication, large goiter, suspicion of thyroid cancer, or coexisting nodules.
Types of Surgeries:
- Thyroidectomy: Partial or complete removal of the thyroid gland.
- Process: Performed under general anesthesia, this surgery involves making an incision in the neck to access the thyroid.
- Recovery and Potential Complications: Recovery typically involves a hospital stay. Potential complications can include hypothyroidism, damage to the vocal cords, and parathyroid glands, which can affect calcium levels in the body.
It’s essential to consult with healthcare professionals to weigh the benefits and risks of each treatment option. This comprehensive approach helps manage the symptoms effectively and improve quality of life.
Managing Graves’ Disease
Graves’ disease, an autoimmune disorder that leads to overactivity of the thyroid gland (hyperthyroidism), requires careful management to control symptoms and maintain a healthy lifestyle. Here are essential strategies for managing Graves’ disease through lifestyle modifications and self-care.
Lifestyle Modifications for Symptom Management
- Dietary Adjustments: Incorporate a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. Specific nutrients such as selenium and calcium can support thyroid health. Limiting stimulants like caffeine and avoiding excessive iodine intake are also beneficial.
- Regular Exercise: Moderate exercise can help manage stress and improve overall well-being. However, it’s important to tailor activities according to energy levels, as fatigue can be a challenge.
- Stress Reduction: Stress can exacerbate symptoms of Graves’ disease. Techniques such as yoga, meditation, and deep breathing can be effective in reducing stress levels.
- Avoid Smoking: Smoking can affect the immune system and worsen the eye problems often associated with Graves’ disease. Quitting smoking is strongly recommended for overall health improvement.
- Sleep Hygiene: Ensuring adequate sleep is crucial; poor sleep can worsen symptoms. Establish a regular bedtime routine and create a comfortable sleep environment.
Importance of Regular Follow-Ups and Monitoring Thyroid Levels
Regular follow-ups with a healthcare provider are vital in managing Graves’ disease. These visits allow for:
- Monitoring of Thyroid Levels: Regular testing of thyroid hormone levels helps in adjusting medications to ensure they are at optimal levels for health and comfort.
- Evaluation of Symptoms: Ongoing assessments can track the progress of symptoms and the effectiveness of treatment strategies.
- Adjustment of Treatment Plans: Treatment may need adjustments over time, and regular check-ups provide the opportunity to refine therapies as needed.
- Prevention of Complications: Early detection of any complications associated with the disease or its treatment can be managed more effectively with regular healthcare visits.
Adopting these lifestyle changes and ensuring consistent medical follow-up can significantly enhance quality of life for those managing Graves’ disease. These steps not only help in controlling the symptoms but also in leading a healthier and more balanced life.
Complications and Challenges of Untreated Graves’ Disease
Managing this condition also presents various challenges that require careful attention. Below, we explore both the potential complications of untreated Graves’ disease and the challenges faced in its management.
Potential Complications of Untreated Graves’ Disease
- Thyroid Storm: This severe, sudden exacerbation of hyperthyroid symptoms can be life-threatening. It requires immediate medical intervention.
- Heart Problems: Chronic untreated hyperthyroidism can lead to atrial fibrillation—a type of irregular heartbeat—which significantly increases the risk of stroke. Additionally, it can cause cardiomyopathy, which impairs the heart muscle’s ability to pump blood effectively.
- Osteoporosis: Excessive thyroid hormone can interfere with the body’s ability to incorporate calcium into the bone. This can lead to weakened bones, increasing the risk of fractures.
- Eye Problems (Graves’ Ophthalmopathy): About 30% of people with Graves’ disease will develop some form of eye trouble, such as bulging eyes, double vision, or light sensitivity. In severe cases, it can lead to vision loss.
- Pregnancy Issues: Pregnant women with uncontrolled hyperthyroidism from Graves’ disease may face increased risks of pregnancy complications, including preterm birth, preeclampsia, and miscarriage.
Challenges in Managing Graves’ Disease
- Diagnosis Challenges: The symptoms of Graves’ disease can mimic those of other conditions, making accurate diagnosis challenging. Symptoms like anxiety, palpitations, and weight loss can be easily attributed to less serious health issues.
- Treatment Side Effects: The most common treatments for Graves’ disease include anti-thyroid medications, radioactive iodine, and surgery. Each treatment option comes with its own set of potential side effects, such as agranulocytosis (a potentially serious decrease in white blood cells) from anti-thyroid drugs, or permanent hypothyroidism requiring lifelong supplementation with thyroid hormone post-radioactive iodine treatment or surgery.
- Monitoring and Adjusting Treatment: Managing Graves’ disease often requires ongoing monitoring and adjustments in treatment to ensure thyroid hormone levels remain within a target range. This can be cumbersome and requires frequent visits to healthcare providers.
- Psychological Impact: The symptoms and chronic nature of Graves’ disease can also take a psychological toll, contributing to anxiety and depression, which themselves need to be managed as part of the overall treatment plan.
The management of Graves’ disease is a delicate balancing act that requires close collaboration between patients and their healthcare providers. By understanding the potential complications and acknowledging the challenges in managing the disease, patients can be better prepared to tackle their condition effectively.
Latest Advances in the Treatment of Graves’ Disease
Graves’ disease, a prevalent form of hyperthyroidism, has seen significant advancements in treatment methods thanks to ongoing research and innovative therapies. This article explores the most recent research findings and emerging treatments that are shaping the future of care for Graves’ disease patients.
Recent Research Findings
Recent studies have shed light on new aspects of Graves’ disease, enhancing our understanding of its pathophysiology and paving the way for innovative treatment approaches. Key findings include the identification of specific genetic markers that may predict susceptibility to Graves’ disease, as well as how environmental factors like stress and diet interact with genetic predispositions to influence disease development.
Furthermore, advancements in imaging and diagnostic technologies have improved the accuracy of Graves’ disease diagnosis. For instance, the use of high-resolution ultrasound technology has become more prominent, allowing for better visualization of the thyroid gland’s condition and activity. This precision is crucial for tailoring treatments to individual needs, leading to improved patient outcomes.
Emerging Treatments and Therapies
In the realm of treatments, there are several exciting developments:
- Biological Therapies: New biologic drugs targeting immune system components specifically involved in the autoimmune attack on the thyroid gland are under development. These treatments aim to reduce thyroid inflammation and prevent excessive hormone production without the side effects associated with traditional therapies.
- Diet and Lifestyle Interventions: There is a growing interest in how diet and lifestyle can affect Graves’ disease. Research is exploring how specific dietary patterns might influence the disease’s progression or mitigate symptoms. For example, studies suggest that diets rich in selenium and low in iodine can help manage symptoms.
- Advanced Drug Therapies: Scientists are also working on refining antithyroid medications to enhance their efficacy and reduce side effects. These advancements include the development of new formulations and delivery methods, such as sustained-release tablets that could improve the quality of life for patients by simplifying dosing schedules.
- Therapeutic Vaccines: Experimental vaccines designed to teach the immune system to tolerate thyroid antigens without attacking them are in early clinical trials. This approach represents a radical shift towards potentially curative treatments for autoimmune thyroid diseases.
These recent and emerging advancements offer hope for more effective and personalized treatment strategies for Graves’ disease, addressing both the symptoms and the underlying autoimmune processes. As research continues to evolve, it is expected that these innovations will significantly improve the quality of life for those affected by this challenging condition.
FAQs about Graves’ Disease Treatment
What is the most common treatment for Graves’ Disease?
The most common treatment for Graves’ Disease includes anti-thyroid medications, radioactive iodine therapy, and sometimes surgery. These treatments aim to reduce thyroid hormone production and alleviate symptoms.
How long does it take for treatment to work?
Treatment duration can vary depending on the method used. Anti-thyroid medications may start to show results within a few weeks, but it could take several months to achieve full control. Radioactive iodine therapy often requires several weeks to months to be fully effective.
Are there any side effects of Graves’ Disease treatments?
Yes, treatments for Graves’ Disease can have side effects. Anti-thyroid medications may cause rash, joint pain, or liver issues. Radioactive iodine can lead to a temporary increase in symptoms and may eventually cause hypothyroidism, requiring ongoing thyroid hormone replacement therapy.
Can Graves’ Disease come back after treatment?
There is a possibility of relapse in Graves’ Disease. The risk varies with the type of treatment. For example, approximately 20-30% of patients treated with anti-thyroid drugs may experience a recurrence. Discussing long-term management strategies with your healthcare provider is important.
Is surgery a good option for Graves’ Disease?
Surgery to remove the thyroid gland (thyroidectomy) might be recommended if other treatments are ineffective or if there’s a large goiter causing discomfort. It’s a definitive treatment but requires lifelong thyroid hormone replacement.
Can I manage Graves’ Disease with lifestyle changes?
While lifestyle changes alone cannot cure Graves’ Disease, they can complement medical treatments. Avoiding iodine-rich foods, managing stress, and quitting smoking are beneficial in managing symptoms.
Is it safe to get pregnant while undergoing treatment for Graves’ Disease?
Pregnancy requires careful management if you have Graves’ Disease. Some treatments, particularly radioactive iodine, are not safe during pregnancy. Always consult your doctor to adjust your treatment plan if you are pregnant or planning to become pregnant.
Conclusion
In summary, recognizing and treating Graves’ Disease is crucial for maintaining optimal health and well-being. This autoimmune disorder can significantly impact various aspects of an individual’s life if left unmanaged.
Timely diagnosis and appropriate treatment are essential to control the symptoms and prevent long-term complications. We strongly encourage all patients to maintain open communication with their healthcare providers. Working closely with medical professionals ensures that treatment plans are effective and tailored to individual needs.
Remember, managing Graves’ Disease is a collaborative effort, and proactive patient involvement is key to achieving the best possible health outcomes. Stay informed, stay engaged, and prioritize your health.
References
For those seeking further information on the treatment of Graves’ Disease, the following reputable sources offer in-depth knowledge and are excellent for validating the details provided in our discussion:
- Mayo Clinic – This comprehensive resource provides detailed insights into the diagnosis, treatment options, and management of Graves’ Disease. Read more about Graves’ Disease on the Mayo Clinic website.
- National Institutes of Health (NIH) – NIH offers a wealth of scientific articles and research papers that delve into the complexities of Graves’ Disease, including its symptoms, causes, and treatments. Explore NIH resources on Graves’ Disease.
- American Thyroid Association (ATA) – The ATA is a leading authority on thyroid-related health issues. Their website contains guidelines for the diagnosis and management of Graves’ Disease, supported by the latest research. Visit the American Thyroid Association for more information.
These sources are recognized for their credibility in the medical field and provide valuable insights for both patients and healthcare providers interested in understanding and managing Graves’ Disease effectively.