Dilated Cardiomyopathy Symptoms: Dilated Cardiomyopathy (DCM) is a significant medical condition that affects the heart’s ability to pump blood efficiently.
Characterized by an enlarged and weakened heart muscle, this disease can lead to heart failure and other serious health complications if not properly managed.
This article aims to provide a comprehensive overview of the symptoms and causes of Dilated Cardiomyopathy, offering valuable insights for those affected by or interested in understanding this condition.
Understanding Dilated Cardiomyopathy
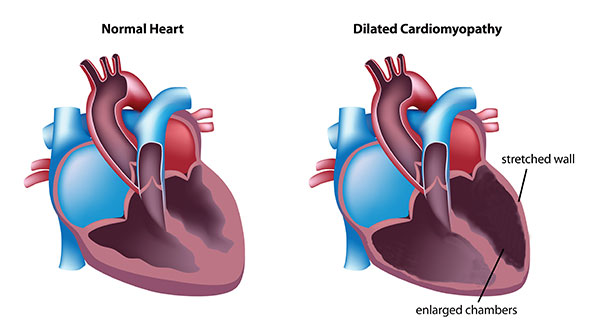
Dilated cardiomyopathy (DCM) is a condition that affects the heart’s ability to pump blood effectively. It’s characterized by an enlargement and weakening of the heart’s left ventricle, which is the main pumping chamber. This enlargement can affect the heart’s structure and function, leading to a decrease in blood flow throughout the body and can result in heart failure or arrhythmias if left untreated.
Statistics and Prevalence
Dilated cardiomyopathy is not as rare as one might think. It is among the most common types of cardiomyopathy and a leading cause of heart failure worldwide. The condition affects individuals of all ages but is most commonly diagnosed in people between the ages of 20 and 60. According to the American Heart Association, DCM affects approximately 1 out of every 2,500 individuals globally. However, it’s important to note that the prevalence can vary significantly by region, age, and gender.
Studies suggest that DCM may be slightly more common in men than in women. Furthermore, certain genetic factors can increase the risk of developing DCM, indicating that family history plays a crucial role in its prevalence. Environmental factors, such as exposure to toxins, use of certain medications, and viral infections, have also been linked to the development of dilated cardiomyopathy, suggesting that both genetics and lifestyle can influence an individual’s risk.
However, understanding the implications of dilated cardiomyopathy is essential for early diagnosis and treatment. With advancements in medical technology and treatments, many individuals with DCM can manage their symptoms effectively and lead active, fulfilling lives. Awareness and education about the condition’s signs, symptoms, and risk factors are key to improving outcomes for those affected by DCM.
Symptoms of Dilated Cardiomyopathy
Understanding the symptoms of dilated cardiomyopathy is crucial for early diagnosis and treatment. Symptoms range from early signs that may be mild and vague to advanced symptoms that indicate significant heart dysfunction.
Early Signs and Symptoms
In the initial stages, individuals with dilated cardiomyopathy might not experience any symptoms. However, as the condition progresses, early signs and symptoms can emerge, often subtle and easily overlooked. These include:
- Fatigue: A common early symptom, where individuals feel unusually tired or exhausted from routine activities.
- Shortness of Breath: Initially noticeable during physical exertion, but as the condition progresses, it can occur even at rest.
- Swelling (Edema): Fluid accumulation may cause swelling in the legs, ankles, and feet.
- Palpitations: Irregular heartbeats or the sensation of a fluttering heart can be an early warning sign.
Advanced Symptoms
As dilated cardiomyopathy advances, symptoms become more pronounced and severe, reflecting the heart’s inability to pump blood efficiently. Advanced symptoms include:
- Persistent Shortness of Breath: Aggravated by even minimal activity or while lying flat.
- Severe Swelling: Extensive fluid buildup leading to swelling in the legs, ankles, and abdomen.
- Chest Pain: Especially during activities or stress, indicating potential strain on the heart.
- Dizziness and Fainting: Caused by inadequate blood flow to the brain.
- Rapid Weight Gain: Sudden weight increase due to fluid retention.
- Coughing: Persistent coughing or wheezing, which may be worse at night.
Recognizing these symptoms promptly and seeking medical attention can significantly impact the management and outcome of dilated cardiomyopathy. Early diagnosis allows for interventions that can help manage symptoms, improve quality of life, and potentially slow the progression of the disease.
Causes and Risk Factors of Dilated Cardiomyopathy
Understanding the causes and risk factors of dilated cardiomyopathy can help in its prevention, early detection, and treatment. Here, we delve into the primary causes and risk factors associated with DCM.
Genetic Factors
Genetics play a significant role in the development of dilated cardiomyopathy. It’s estimated that 20-35% of DCM cases have a familial basis, meaning they are inherited from one’s parents. Specific gene mutations can affect the heart’s structure and function, leading to the development of DCM. If you have a family history of DCM, it’s crucial to inform your healthcare provider, as you may be at an increased risk of developing the condition.
Viral Infections Leading to Inflammation of the Heart
Viral infections are a common cause of inflammation of the heart muscle, known as myocarditis, which can progress to dilated cardiomyopathy. Viruses such as Coxsackievirus, Adenovirus, and Parvovirus B19 are known to affect the heart. The inflammation resulting from these viral infections can damage the heart muscle, reducing its ability to pump blood efficiently and leading to DCM in some individuals.
Alcohol Abuse and Toxic Exposure
Excessive alcohol consumption is a well-documented risk factor for developing dilated cardiomyopathy. Alcohol has a toxic effect on the heart muscle, leading to its weakening and eventual enlargement. Additionally, exposure to certain toxins, including chemotherapy drugs and exposure to heavy metals, can also lead to DCM. Limiting alcohol intake and avoiding toxic exposures can reduce the risk of developing this condition.
Underlying Conditions
Several underlying health conditions can increase the risk of developing dilated cardiomyopathy. High blood pressure (hypertension) and coronary artery disease are among the leading risk factors. These conditions can put undue stress on the heart, leading to weakening and enlargement of the left ventricle. Managing these underlying conditions through lifestyle changes and medication can help reduce the risk of developing DCM.
Dilated cardiomyopathy is a complex condition with various causes and risk factors. Genetic predisposition, viral infections, alcohol abuse, toxic exposure, and underlying health conditions all contribute to the development of DCM. Understanding these risk factors is essential for prevention and early detection. If you are at risk of DCM, it’s crucial to adopt a heart-healthy lifestyle and seek regular medical check-ups to monitor your heart health.
Diagnosing Dilated Cardiomyopathy
Early detection and diagnosis are critical to managing and potentially improving outcomes for those affected by this condition. Here, we delve into the diagnosis process, emphasizing the significance of early detection, the role of physical examinations and medical history, and the diagnostic tests employed.
Physical Examination and Medical History
The journey to diagnosing Dilated Cardiomyopathy begins with a thorough physical examination and a detailed medical history. Healthcare providers look for signs and symptoms indicative of heart failure, such as shortness of breath, fatigue, swelling in the legs, and irregular heartbeats. A comprehensive medical history helps to identify any underlying conditions or genetic predispositions that might contribute to the development of DCM. Factors such as a family history of heart disease, alcohol consumption, and exposure to toxins are considered critical in assessing risk.
Diagnostic Tests
Following the initial evaluation, several diagnostic tests are essential in confirming the presence of Dilated Cardiomyopathy:
- Echocardiogram: This non-invasive test uses ultrasound waves to create images of the heart, allowing doctors to assess the size of the heart chambers, the extent of dilation, and the heart’s pumping efficiency. An echocardiogram is pivotal in diagnosing DCM by revealing structural heart changes and functional impairments.
- Magnetic Resonance Imaging (MRI): Cardiac MRI provides detailed images of the heart’s structure and function. It is particularly useful in distinguishing DCM from other heart conditions and assessing the extent of damage or scarring within the heart muscle.
- Blood Tests: While not diagnostic of DCM itself, blood tests can identify markers of heart failure and rule out other conditions. Tests may include checking for levels of B-type natriuretic peptide (BNP) or N-terminal pro b-type natriuretic peptide (NT-proBNP), which are elevated in heart failure.
The Importance of Early Detection
Early detection of Dilated Cardiomyopathy is crucial. It allows for the timely initiation of treatment strategies aimed at managing symptoms, slowing disease progression, and improving quality of life. Early intervention can also mitigate the risk of complications such as heart failure, arrhythmias, and thromboembolic events, which can have life-threatening consequences.
However, diagnosing Dilated Cardiomyopathy involves a multifaceted approach that includes a detailed physical examination, a comprehensive review of medical history, and specific diagnostic tests. Recognizing the importance of early detection can significantly influence the management and prognosis of DCM, underscoring the need for awareness and timely medical intervention. By prioritizing these diagnostic steps, healthcare providers can offer effective treatment plans tailored to the individual needs of those affected by this challenging condition.
Treatment Options for Dilated Cardiomyopathy
Managing this condition involves a comprehensive approach, including medications, lifestyle adjustments, and possibly surgical or non-surgical interventions. Below, we explore these treatment options in detail, focusing on enhancing both understanding and accessibility of the information.
Medications
Medications play a pivotal role in managing dilated cardiomyopathy by improving heart function, controlling symptoms, and preventing complications. The most common classes of medications used include:
- ACE inhibitors or ARBs (Angiotensin II Receptor Blockers): These drugs help relax blood vessels, lowering blood pressure and reducing the heart’s workload.
- Beta-blockers: They slow down the heart rate and reduce blood pressure, which can improve heart function and symptoms.
- Diuretics: Also known as water pills, diuretics help eliminate excess fluid in the body, reducing symptoms such as swelling and shortness of breath.
- Aldosterone antagonists: These can help reduce fluid retention and offer protection against heart damage.
- Digitalis: This medication can strengthen the heart muscle, improving its ability to pump blood.
Each patient’s medication regimen is tailored based on their specific symptoms and the severity of their condition. Regular follow-ups are necessary to adjust the treatment as needed and to monitor for any side effects.
Lifestyle Changes and Management
Adopting healthy lifestyle changes is essential for managing dilated cardiomyopathy. These modifications can help alleviate symptoms, improve quality of life, and slow the progression of the disease. Key recommendations include:
- Dietary adjustments: A heart-healthy diet low in salt, saturated fats, and cholesterol is advised to help manage blood pressure and prevent fluid retention.
- Physical activity: Engaging in moderate exercise, as recommended by a healthcare provider, can improve heart health and physical fitness. However, it’s crucial to balance activity with rest.
- Avoiding alcohol and smoking: These substances can worsen heart health and are discouraged.
- Regular monitoring: Keeping track of blood pressure, cholesterol levels, and weight can help manage the condition effectively.
- Stress management: Techniques such as meditation, deep breathing, or yoga can help reduce stress, which is beneficial for heart health.
Surgical and Non-Surgical Procedures
In some cases, medications and lifestyle changes may not be sufficient to manage dilated cardiomyopathy effectively. Surgical or non-surgical procedures may be necessary, including:
- Cardiac resynchronization therapy (CRT): This involves the implantation of a special pacemaker that helps the heart’s chambers beat in sync, improving heart function.
- Implantable cardioverter-defibrillators (ICDs): ICDs are devices implanted to monitor heart rhythms and deliver electrical shocks when necessary to prevent life-threatening arrhythmias.
- Heart valve surgery: If dilated cardiomyopathy has led to significant heart valve problems, surgery may be required to repair or replace the affected valve(s).
- Heart transplant: In severe cases where other treatments have failed and the heart is severely damaged, a heart transplant may be considered as a last resort.
Treatment for dilated cardiomyopathy is highly individualized and depends on various factors, including the cause of the condition, the severity of symptoms, and the presence of any complications. Ongoing care from a team of heart specialists is crucial to effectively manage the disease and improve the patient’s quality of life.
By understanding and implementing the appropriate treatment options, individuals with dilated cardiomyopathy can lead active and fulfilling lives. Regular consultations with healthcare providers, adherence to prescribed treatments, and commitment to lifestyle changes are key components of successful management.
Managing Symptoms and Preventing Progression of Dilated Cardiomyopathy
Managing symptoms and preventing its progression are crucial for maintaining quality of life and minimizing complications. This article provides insights into the importance of regular monitoring, lifestyle modifications, and coping strategies to support patients with DCM.
Regular Monitoring and Follow-Ups
Regular monitoring and follow-up appointments with a healthcare provider are essential for managing dilated cardiomyopathy effectively. These appointments allow for the assessment of heart function, monitoring of symptom progression, and adjustments to treatment plans as necessary. Routine echocardiograms, electrocardiograms, and blood tests can help track the health of your heart and the effectiveness of your treatment. It’s also an opportunity to discuss any new symptoms or concerns with your healthcare provider, ensuring that your condition is managed as effectively as possible.
Importance of Lifestyle Modifications
Lifestyle modifications play a significant role in managing dilated cardiomyopathy and improving overall heart health. Here are key changes that can make a difference:
- Healthy Diet: Consuming a heart-healthy diet that is low in saturated fats, trans fats, and cholesterol can help manage blood pressure and reduce heart disease risk. Increasing intake of fruits, vegetables, whole grains, and lean proteins is beneficial.
- Regular Exercise: Engaging in regular, moderate exercise can improve heart health and physical fitness. However, it’s important to consult with a healthcare provider before starting any new exercise regimen.
- Limiting Alcohol and Avoiding Smoking: Alcohol can worsen heart conditions, and smoking is a major risk factor for heart diseases. Limiting alcohol consumption and quitting smoking are critical steps in managing DCM.
- Weight Management: Maintaining a healthy weight can reduce the strain on the heart and help manage symptoms of DCM.
Coping Strategies and Support for Patients
Living with dilated cardiomyopathy can be challenging, but there are strategies and support systems that can help:
- Emotional Support: Emotional and psychological support is vital. Consider joining a support group for people with heart conditions to connect with others facing similar challenges.
- Stress Management: Stress can negatively affect heart health. Techniques such as meditation, deep breathing exercises, and yoga can help manage stress levels.
- Education: Educating yourself about dilated cardiomyopathy can empower you to make informed decisions about your care and treatment. Ask your healthcare provider for resources or seek reputable information online.
It’s important to work closely with your healthcare team to tailor a management plan that suits your individual needs and lifestyle. Regular monitoring, lifestyle modifications, and a strong support network are key components of effective DCM management.
FAQs on Dilated Cardiomyopathy
What is Dilated Cardiomyopathy?
Dilated cardiomyopathy is a disease of the heart muscle, primarily affecting the heart’s ventricles. In DCM, the ventricles enlarge (dilate) and cannot pump blood effectively. This condition can lead to heart failure and other complications.
What Causes Dilated Cardiomyopathy?
The exact cause of DCM is often unknown. However, it can be linked to genetic factors, viral infections, autoimmune diseases, exposure to toxins (including alcohol and certain drugs), and underlying medical conditions such as diabetes and thyroid disorders.
What are the Symptoms of Dilated Cardiomyopathy?
Symptoms of DCM can vary widely from none to severe. They may include shortness of breath, fatigue, swelling of the legs and feet (edema), irregular heartbeats that feel rapid, fluttering, or pounding (palpitations), and chest pain.
How is Dilated Cardiomyopathy Diagnosed?
Diagnosis of DCM involves a combination of patient history, physical examination, and diagnostic tests. These tests may include an echocardiogram (echo), electrocardiogram (ECG), MRI, blood tests, and sometimes a biopsy of the heart muscle.
Can Dilated Cardiomyopathy be Treated?
While there is no cure for DCM, treatments are available to help manage symptoms and prevent complications. Treatment options include medications, lifestyle changes (such as diet and exercise), and in severe cases, devices like pacemakers or defibrillators, or heart transplant.
Is Dilated Cardiomyopathy Hereditary?
Yes, DCM can be hereditary. If you have a family history of DCM or other heart diseases, it is important to inform your doctor as you may be at increased risk.
Can Lifestyle Changes Affect Dilated Cardiomyopathy?
Lifestyle changes can significantly impact the management of DCM. Regular exercise, a heart-healthy diet, avoiding alcohol and tobacco, and managing stress can help improve heart function and quality of life.
What is the Prognosis for Someone with Dilated Cardiomyopathy?
The prognosis for individuals with DCM varies. Factors affecting prognosis include the cause of the condition, how early it is diagnosed, how well symptoms are managed, and the presence of other health issues. With proper treatment and lifestyle adjustments, many people with DCM can lead active, normal lives.
Conclusion
If you or someone you know is experiencing symptoms that could be indicative of dilated cardiomyopathy, it is essential to seek medical advice promptly. Early diagnosis and treatment can significantly improve the quality of life and prognosis for individuals with DCM.
Treatments may include medications, lifestyle changes, and in some cases, surgical interventions such as the implantation of devices to support heart function. Consulting a healthcare provider can also provide valuable information and access to support and resources for managing the condition.
In conclusion, while dilated cardiomyopathy is a serious heart condition, understanding its symptoms and causes, seeking timely medical advice, and staying informed about the latest research and treatments can empower individuals to manage the condition effectively. With the continued advancements in medical research, there is hope for even better outcomes and quality of life for those affected by DCM.