Cyclothymia Treatment: Cyclothymia, also known as Cyclothymic Disorder, is a complex mood disorder that sits within the bipolar spectrum.
It is characterized by chronic, fluctuating mood disturbances involving numerous periods of hypomanic symptoms and periods of depressive symptoms. Understanding, diagnosing, and treating Cyclothymia is critical for improving the lives of those affected by it.
This article delves deeply into the nuances of Cyclothymia, offering comprehensive insights into its diagnosis and treatment.
Understanding Cyclothymia
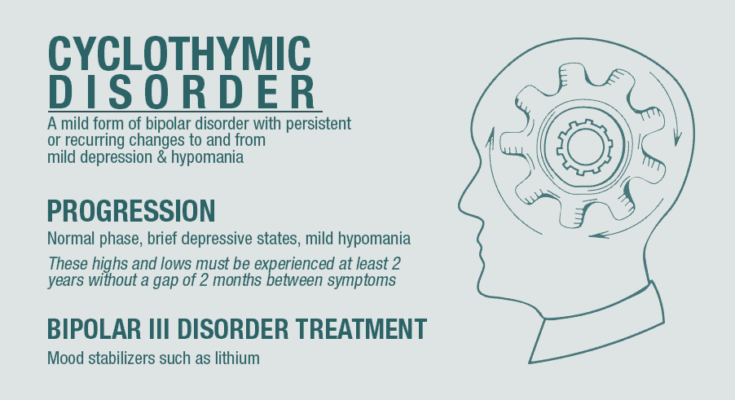
Cyclothymia, also known as Cyclothymic Disorder, is a mood disorder that causes emotional ups and downs, but with less severe symptoms than those found in bipolar disorder. Understanding the nuances of Cyclothymia is essential for recognizing its impact on individuals’ lives and differentiating it from other mood disorders.
Characteristics of Cyclothymic Disorder
Cyclothymic Disorder is characterized by periods of hypomanic symptoms followed by episodes of depressive symptoms. These mood swings are less intense than those experienced in Bipolar I or II Disorders but are more chronic and can affect individuals’ daily functioning and quality of life. Key characteristics include:
- Mood Swings: Individuals experience noticeable fluctuations in mood, from feeling upbeat and energized (hypomanic episodes) to feeling low and sad (depressive episodes).
- Duration: Symptoms persist for at least two years in adults and one year in children and adolescents, with no symptom-free period lasting longer than two months.
- Severity: While the symptoms of cyclothymia are milder than those of full-blown bipolar disorder or major depression, they are significant enough to interfere with daily life but not severe enough to warrant a diagnosis of bipolar disorder or major depressive disorder.
Comparison with Other Mood Disorders
Cyclothymia is unique when compared to other mood disorders such as Bipolar Disorder and Major Depression, primarily in terms of symptom severity and duration. Here are key distinctions:
- Bipolar Disorder: Bipolar disorder is marked by more extreme episodes of mania or hypomania and depression. Cyclothymia’s mood swings are less severe and are ongoing without the extended periods of normal mood seen in bipolar disorder.
- Major Depression: Unlike major depression, which involves prolonged periods of severe depression, cyclothymia includes episodes of mild depression interspersed with periods of hypomania.
Understanding these differences is crucial for accurate diagnosis and treatment.
Statistics on Prevalence and Demographics Affected
Cyclothymia affects a broad demographic, with estimates suggesting that it impacts 0.4% to 1% of the population. It can develop in late adolescence or early adult life, and the onset is often gradual. Both men and women are equally likely to be diagnosed with Cyclothymic Disorder, contrasting with some mood disorders that show a higher prevalence in one gender.
The disorder is chronic, and while some individuals may experience periods where symptoms are less pronounced, many will continue to experience mood swings throughout their lives. Early diagnosis and treatment are key to managing symptoms effectively.
However, Cyclothymia is a chronic mood disorder characterized by milder, yet significant, mood swings than those seen in bipolar disorder and major depression. Its unique features, including the chronic nature of mood fluctuations and the less severe but still impactful symptoms, underscore the importance of understanding and recognizing this disorder. Awareness and education can lead to better outcomes for those affected, through timely and appropriate interventions.
Symptoms of Cyclothymia
Understanding its symptoms is crucial for recognizing its presence and seeking appropriate help. This guide aims to provide a detailed overview of cyclothymia symptoms, their impact on daily life and relationships, and advice on when to seek professional assistance.
Detailed List of Cyclothymia Symptoms
Cyclothymia symptoms can be divided into two categories: hypomanic and depressive episodes. These symptoms fluctuate, but they are less intense than those experienced in bipolar I or II disorders.
Hypomanic Symptoms:
- Elevated mood or euphoria
- Increased self-esteem or grandiosity
- Decreased need for sleep
- More talkative than usual or pressure to keep talking
- Flight of ideas or subjective experience that thoughts are racing
- Distractibility
- Increase in goal-directed activity (either socially, at work or school, or sexually) or physical restlessness
- Engaging in activities with a high potential for painful consequences (e.g., unrestrained buying sprees, sexual indiscretions)
Depressive Symptoms:
- Feelings of sadness, emptiness, or hopelessness
- Marked loss of interest or pleasure in all, or almost all, activities
- Significant weight loss when not dieting, weight gain, or decrease or increase in appetite
- Insomnia or hypersomnia
- Psychomotor agitation or retardation
- Fatigue or loss of energy
- Feelings of worthlessness or excessive or inappropriate guilt
- Diminished ability to think or concentrate, or indecisiveness
- Thoughts of death or suicide, or suicide attempt
Impact on Daily Life and Relationships
The fluctuating nature of cyclothymia can significantly disrupt daily life and relationships. During hypomanic episodes, individuals may take on too many tasks, leading to stress and uncompleted projects once a depressive episode hits. The impulsive behaviors common in hypomanic phases can also strain relationships, leading to conflicts or misunderstandings.
Depressive episodes, on the other hand, can make it difficult for individuals to maintain their responsibilities at work or home. The lack of energy and motivation can result in neglected duties and isolation from social activities, further impacting relationships negatively.
When to Seek Help: Recognizing the Severity and Persistence of Symptoms
Recognizing the need for professional help is a critical step toward managing cyclothymia. It’s essential to seek assistance if:
- The symptoms significantly impact your quality of life, including your ability to work, maintain relationships, and perform daily activities.
- You notice a persistent pattern of emotional highs and lows over at least two years (one year in children and adolescents).
- Your mood swings are not caused by substance abuse or another medical condition.
Early diagnosis and treatment are key to managing cyclothymia effectively. Treatments may include psychotherapy, medications, or a combination of both, tailored to the individual’s needs. If you or someone you know is experiencing these symptoms, reaching out to a healthcare professional can provide the necessary support and guidance.
However, understanding cyclothymia and its effects is the first step toward seeking help and managing symptoms. By recognizing the signs and knowing when to seek professional advice, individuals can navigate their condition more effectively and improve their quality of life.
Causes and Risk Factors of Cyclothymia (Cyclothymic Disorder)
Understanding the potential causes and risk factors associated with cyclothymia is crucial for awareness and early intervention. While the exact cause of cyclothymia remains unknown, research suggests a combination of genetic, biological, and environmental factors play a significant role.
Genetic Factors
Evidence indicates a genetic predisposition to cyclothymia. If a close family member, such as a parent or sibling, has been diagnosed with cyclothymia or another mood disorder, the likelihood of developing cyclothymic disorder increases. Studies on twins and families suggest that the risk is partially inherited, pointing towards a genetic component in the disorder’s onset.
Biological Factors
Biological aspects, including brain structure and neurotransmitter function, are believed to influence the development of cyclothymia. Neurotransmitters are chemical messengers in the brain responsible for communication between nerve cells. An imbalance in these chemicals, particularly serotonin, dopamine, and norepinephrine, may contribute to mood disorders, including cyclothymia. Moreover, differences in brain structure and function observed in people with mood disorders might also play a role, although further research is needed to understand these connections fully.
Environmental Factors
Environmental triggers and stressful life events can also contribute to the onset of cyclothymia. Events such as the death of a loved one, relationship issues, financial problems, or significant life changes can trigger the development of cyclothymic disorder in individuals predisposed to mood disorders. Additionally, substance abuse and certain medications may exacerbate or trigger symptoms.
Risk Factors
Several factors may increase the likelihood of developing cyclothymia, including:
- Family History: Having a family member with cyclothymia or another mood disorder increases your risk.
- Stressful Life Events: Major life changes or stressful events can trigger the onset of cyclothymic disorder.
- Personality and Psychological Factors: Certain personality traits, such as high neuroticism, or psychological issues, like anxiety disorders, may predispose individuals to cyclothymia.
- Substance Abuse: The use of drugs or alcohol can complicate or trigger mood disorders, including cyclothymia.
It’s important to note that having one or more risk factors does not mean a person will definitely develop cyclothymia. Similarly, individuals without these risk factors can still develop the disorder. Early detection and treatment are crucial for managing symptoms and improving quality of life. If you or someone you know is experiencing symptoms of cyclothymia, seeking professional help is a vital step towards recovery.
However, cyclothymia’s causes are multifaceted, involving genetic, biological, and environmental factors. By understanding these aspects and recognizing the risk factors, individuals can seek early intervention and support, leading to better outcomes and management of the disorder.
Diagnosis of Cyclothymia
Diagnosing cyclothymia—a mood disorder characterized by fluctuations between mild depressive and hypomanic states—requires a careful and systematic approach. Healthcare professionals rely on specific criteria, face common challenges, and utilize patient history and symptom tracking to make accurate diagnoses.
Criteria Used by Healthcare Professionals
The diagnosis of cyclothymia hinges on the criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), published by the American Psychiatric Association. These criteria include experiencing periods of hypomanic symptoms and periods of depressive symptoms for at least two years (one year in children and adolescents), without the symptoms meeting the full criteria for a major depressive episode, manic episode, or hypomanic episode. Importantly, these mood swings are significant enough to cause distress or impairment in social, occupational, or other important areas of functioning.
Healthcare professionals conduct thorough psychiatric evaluations, which may involve:
- Psychological questionnaires to understand the mood fluctuations and their impact on daily life.
- Clinical interviews to gather comprehensive medical, psychiatric, and family history.
- Physical examinations and lab tests to rule out other conditions that might mimic or contribute to mood disorders.
Common Challenges in Diagnosing Cyclothymia
Diagnosing cyclothymia presents unique challenges, primarily because its symptoms can be subtle and may overlap with other mood disorders such as major depression, bipolar disorder, and even personality disorders. Additionally, individuals with cyclothymia might not seek help during hypomanic episodes as they often feel more productive and well during these times.
To address these challenges, healthcare providers may:
- Employ longitudinal assessments: Continuously monitoring symptoms over time helps distinguish cyclothymia from other mood disorders.
- Use specialized screening tools: These tools are designed to pick up the nuances of cyclothymic disorder, aiding in accurate diagnosis.
- Consultation with specialists: In complex cases, specialists in mood disorders may be consulted to provide additional insight and confirm the diagnosis.
The Role of Medical History and Symptom Tracking in Diagnosis
A detailed medical history and systematic symptom tracking play crucial roles in diagnosing cyclothymia. Patients are often encouraged to keep a mood diary, documenting daily emotional states, sleep patterns, and significant life events. This practice helps in identifying the cyclical patterns of mood changes characteristic of cyclothymia.
Healthcare professionals also delve into family history, as genetic predisposition is a known risk factor for cyclothymic disorder and other mood disorders. Understanding the patient’s personal and family medical history aids in ruling out other potential causes and tailoring the diagnostic process to the individual’s specific situation.
However, diagnosing cyclothymia is a comprehensive process that involves a detailed evaluation of symptoms against established criteria, addressing the inherent challenges with targeted strategies, and leveraging patient history and symptom tracking. By adopting a meticulous approach, healthcare professionals can ensure accurate diagnosis and appropriate management of cyclothymia, ultimately enhancing the quality of life for those affected.
Cyclothymia Treatment Options
Treatment options for cyclothymia focus on managing symptoms, preventing the progression to bipolar disorder, and improving quality of life. Here, we explore the various treatment modalities, including medications, psychotherapy, lifestyle and home remedies, and emerging treatments.
Medications
Although there’s no one-size-fits-all medication for cyclothymia, doctors may prescribe a variety of medications to help manage the symptoms. These can include:
- Mood Stabilizers: Drugs such as lithium are often the first line of defense in stabilizing mood swings associated with cyclothymia.
- Anticonvulsants: Medications like valproic acid and lamotrigine may also be effective in stabilizing mood.
- Antipsychotics: In some cases, especially when symptoms are severe, atypical antipsychotics may be recommended.
- Antidepressants: These are used cautiously due to the risk of triggering manic episodes, often in combination with a mood stabilizer.
It’s crucial for individuals to work closely with their healthcare provider to find the most effective medication regimen, as response to treatment can vary widely.
Psychotherapy
Psychotherapy plays a pivotal role in treating cyclothymia, with several approaches showing effectiveness:
- Cognitive Behavioral Therapy (CBT): Helps individuals identify and change negative thought patterns and behaviors, aiming to manage symptoms better.
- Interpersonal and Social Rhythm Therapy (IPSRT): Focuses on stabilizing daily rhythms such as sleeping, eating, and activity schedules, which can help manage mood swings.
- Psychoeducation: Learning about cyclothymia can empower patients to manage their condition more effectively.
Therapy can provide tools and strategies for coping with stress, improving relationships, and maintaining a stable mood.
Lifestyle and Home Remedies
In addition to medical treatments, lifestyle adjustments and home remedies can significantly aid in managing cyclothymia:
- Regular Exercise: Engaging in physical activity can help reduce depressive symptoms and improve overall mood.
- Healthy Diet: A balanced diet can have a positive impact on mood and energy levels.
- Sleep Hygiene: Maintaining a regular sleep schedule helps stabilize mood swings.
- Stress Management: Techniques such as meditation, yoga, and deep-breathing exercises can reduce stress and improve emotional well-being.
Emerging Treatments
Research into new treatments for cyclothymia is ongoing, with some promising avenues:
- Transcranial Magnetic Stimulation (TMS): A non-invasive procedure that uses magnetic fields to stimulate nerve cells in the brain, which could help improve symptoms of depression.
- Ketamine Infusions: Though primarily researched for major depression, ketamine shows potential for rapid mood improvement in mood disorders, including cyclothymia.
Emerging treatments offer hope for those who have not found relief with current treatment options, though further research is needed to fully understand their efficacy and safety.
However, managing cyclothymia requires a comprehensive approach that includes medication, psychotherapy, lifestyle adjustments, and staying informed about emerging treatments. It’s essential for individuals with cyclothymia to work closely with their healthcare team to develop a personalized treatment plan that addresses their unique needs. With proper management, people with cyclothymia can lead fulfilling lives.
Living with Cyclothymia
Managing cyclothymia effectively requires a comprehensive approach, focusing on daily coping strategies, as well as the importance of ongoing treatment and regular check-ins with healthcare providers.
Tips for Managing Cyclothymia on a Daily Basis
- Establish a Routine: Maintaining a consistent schedule for sleeping, eating, and physical activity can help stabilize mood swings. Your body thrives on regularity, and a predictable routine can be soothing to your mental health.
- Monitor Mood Changes: Keeping a mood diary can be an effective way to track your emotional states, identify triggers, and recognize patterns. This awareness can empower you to take proactive steps to mitigate the onset of a mood episode.
- Practice Mindfulness and Stress Reduction Techniques: Techniques such as meditation, deep breathing exercises, and yoga can reduce stress and increase your sense of well-being. Mindfulness helps you stay present and can decrease the severity of mood swings.
- Stay Active: Regular physical activity is known to improve mood and can be particularly beneficial for those living with cyclothymia. Aim for activities you enjoy, which can range from walking or cycling to more structured exercise programs.
- Seek Support: Connecting with support groups or participating in therapy sessions can provide valuable coping strategies. Sharing experiences with others who understand what you’re going through can be incredibly supportive.
The Importance of Ongoing Treatment and Regular Check-Ins with Healthcare Providers
Living with cyclothymia necessitates a long-term management plan, which includes ongoing treatment and regular engagement with healthcare professionals.
- Medication Management: For some, medication may be a part of managing cyclothymia. Regular consultations with a healthcare provider are vital to monitor the effectiveness of any prescribed medication and to make adjustments as needed.
- Therapeutic Support: Psychotherapy, such as cognitive behavioral therapy (CBT), can be effective in managing cyclothymia. It can help you develop coping strategies, address negative thought patterns, and improve your overall mental health.
- Regular Check-Ins: Regular appointments with your healthcare provider are crucial to monitor your condition and make necessary adjustments to your treatment plan. These check-ins provide an opportunity to discuss any concerns or changes in your mood and to receive professional guidance.
Recognizing the importance of ongoing treatment and maintaining regular check-ins with healthcare providers are crucial steps in managing cyclothymia effectively. With the right strategies and support, individuals with cyclothymia can navigate their condition successfully, achieving stability and improving their quality of life.
FAQs About Cyclothymia
What is cyclothymia?
Cyclothymia, also known as cyclothymic disorder, is a chronic mood disorder that is characterized by periods of hypomanic symptoms (mild to moderate levels of mania) and periods of depressive symptoms. These symptoms are less severe than those found in full-blown bipolar disorder but can still significantly impact an individual’s life.
How is cyclothymia diagnosed?
A diagnosis of cyclothymia typically involves a thorough evaluation by a mental health professional. This evaluation may include a detailed interview about your symptoms, mood history, and any family history of mood disorders. To be diagnosed with cyclothymia, individuals must experience symptoms of hypomania and depression for at least two years (one year in children and adolescents) with no more than two months symptom-free.
What causes cyclothymia?
The exact cause of cyclothymia is not known, but it is believed to be a combination of genetic, biochemical, and environmental factors. A family history of mood disorders may increase the risk of developing cyclothymia.
How is cyclothymia treated?
Treatment for cyclothymia typically involves a combination of psychotherapy and medication. Cognitive-behavioral therapy (CBT) can help individuals manage their symptoms and develop coping strategies. Medications, such as mood stabilizers and antidepressants, may also be prescribed to help regulate mood swings.
Can cyclothymia turn into bipolar disorder?
While cyclothymia is a separate condition, some individuals may go on to develop bipolar I or II disorder. It’s important for those with cyclothymia to be closely monitored by a mental health professional for any changes in their mood patterns or symptom severity.
Is cyclothymia common?
Cyclothymia is less well-known than other mood disorders like depression and bipolar disorder, making it seem less common. However, it is estimated that cyclothymia affects a small percentage of the population. Due to its mild symptoms, it is often undiagnosed or misdiagnosed as another mood disorder.
How can I support someone with cyclothymia?
Supporting someone with cyclothymia involves being patient, understanding, and encouraging them to seek and continue treatment. Educating yourself about the disorder can also help you provide the empathy and support they need. Encourage healthy lifestyle choices, such as regular exercise, a balanced diet, and sufficient sleep, which can help manage symptoms.
Conclusion
In summary, acknowledging and addressing cyclothymia is crucial for the well-being of individuals and the broader community. This mood disorder, characterized by fluctuations between mild depression and hypomania, often goes unrecognized, leading to unnecessary suffering and missed opportunities for treatment. Recognizing the signs of cyclothymia not only empowers individuals to seek the help they need but also enhances societal understanding and acceptance of mental health conditions.
It’s essential for those experiencing the symptoms of cyclothymia to reach out for professional help. Mental health professionals can provide accurate diagnoses and tailored treatment plans that can significantly improve quality of life. Treatments may include therapy, medication, and lifestyle adjustments, all aimed at stabilizing mood swings and reducing their impact on daily life.
Moreover, society as a whole benefits when we foster an environment of awareness and understanding regarding mental health. Breaking down the stigma associated with mental health conditions like cyclothymia encourages more people to seek help and promotes a culture of support and empathy. Everyone has a role to play in this endeavor, from individuals sharing their stories to organizations advocating for better mental health resources.
In conclusion, cyclothymia is a manageable condition with the right support and treatment. By prioritizing mental health, encouraging open conversations, and advocating for comprehensive care, we can make a significant difference in the lives of those affected. Let’s commit to supporting each other in recognizing and addressing mental health conditions, moving towards a future where everyone feels empowered to seek the help they need.