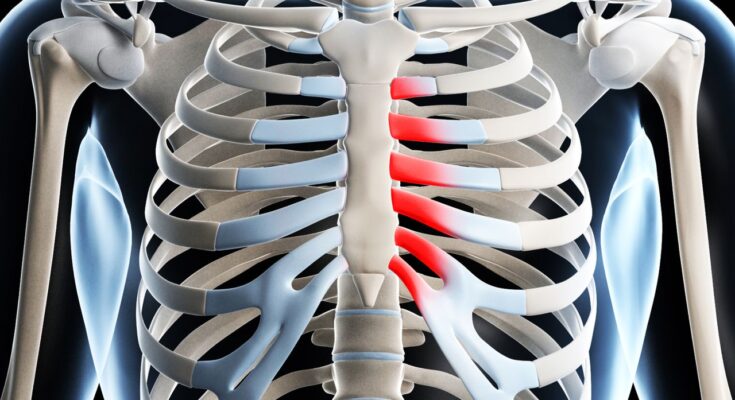
Costochondritis Treatment: Costochondritis, often characterized by chest pain and discomfort, is a condition that affects the cartilage connecting the ribs to the sternum (breastbone).
This condition, while non-life-threatening, can cause significant discomfort and anxiety due to its symptoms mimicking those of a heart attack.
Our comprehensive guide delves into the diagnosis and treatment of costochondritis, aiming to provide valuable insights for those affected.
What is Costochondritis?
Costochondritis is a medical condition characterized by inflammation of the cartilage that connects a rib to the breastbone (sternum). This area, known as the costosternal junction, becomes tender and painful, which can often be mistaken for a heart attack or other heart-related conditions. The pain associated with costochondritis may be sharp, aching, or pressure-like and can become more pronounced with certain activities, such as coughing, deep breathing, or physical movement.
Causes of Costochondritis
The exact cause of costochondritis is often difficult to determine. However, several factors may contribute to the development of this condition. These can include:
- Physical Strain: Heavy lifting, strenuous exercise, or sudden exertion can lead to costochondritis by straining the chest wall muscles and the costosternal junctions.
- Injury: A direct blow to the chest can cause inflammation of the costal cartilage.
- Arthritis: Conditions such as osteoarthritis, rheumatoid arthritis, and ankylosing spondylitis are known to affect the rib joints and may lead to costochondritis.
- Infection: In rare cases, the costochondral joint can become infected by bacteria, viruses, or fungi, particularly in individuals who use IV drugs or have had surgery near the chest area.
- Repetitive Motion: Activities that involve repetitive motion of the upper body, such as rowing or weightlifting, can predispose individuals to developing costochondritis.
Statistics on Prevalence
Costochondritis is relatively common and can affect individuals of any age, but it is more frequently diagnosed in people over 40 years of age. The condition tends to affect females slightly more than males, although the reasons for this disparity are not fully understood.
- Age Groups: While it can occur at any age, middle-aged to older adults are more commonly affected.
- Gender: Studies suggest a slight female predominance in reported cases of costochondritis.
- Prevalence: Exact prevalence rates are difficult to establish due to the self-limiting nature of the condition and the fact that many cases may resolve without medical intervention. However, it is estimated that costochondritis accounts for 10-30% of all chest pain cases seen in primary care settings.
However, understanding costochondritis, its causes, and prevalence can help individuals identify the condition and seek appropriate treatment. Although costochondritis can be painful, it is generally benign and can be managed effectively with conservative treatments such as rest, anti-inflammatory medications, and physical therapy. If you suspect you have costochondritis, consulting with a healthcare provider is essential to receive an accurate diagnosis and appropriate care.
Symptoms of Costochondritis
Identifying the symptoms of costochondritis is crucial for proper diagnosis and treatment. Below, we delve into the common symptoms of costochondritis and offer guidance on differentiating it from similar conditions, such as heart attacks.
Detailed List of Common Symptoms
- Sharp, Aching Chest Pain: The primary symptom of costochondritis is sharp or aching pain in the front of the chest, typically on the left side, but it can affect both sides of the chest.
- Pain Worsened by Physical Activity: Engaging in physical activities or exercises can exacerbate the pain associated with costochondritis.
- Pain Triggered by Pressure: Applying pressure to the rib cage or sternum area where the ribs meet the breastbone can trigger or increase pain, making it a distinctive symptom of costochondritis.
- Pain That Radiates: In some cases, the pain may radiate, creating discomfort in the back or abdomen, though this is less common.
- Tenderness: The affected area is often tender to the touch, which can help in diagnosing costochondritis.
- Redness or Swelling: Although less common, some individuals may experience redness or swelling in the affected area.
Differentiating Costochondritis from Other Conditions
Distinguishing costochondritis from a heart attack or other heart conditions is vital because they can share similar symptoms, such as chest pain. Here are key differences to help identify costochondritis:
- Location and Nature of Pain: Costochondritis pain is usually localized to the area where the ribs meet the sternum and can be reproduced by pressing on the rib joints, which is not typical of heart-related chest pain.
- Physical Activity Impact: While physical activity can worsen costochondritis pain, heart attack pain is more likely to occur during physical exertion but won’t intensify with pressure applied to the chest area.
- Additional Symptoms: Heart attacks may be accompanied by other symptoms such as shortness of breath, nausea, sweating, and pain radiating to the arm or jaw. These symptoms are generally not present with costochondritis.
- Duration: Costochondritis pain can persist for weeks to months and may recur, whereas heart attack symptoms are more acute and develop rapidly.
If you experience persistent chest pain, it is essential to consult with a healthcare provider to receive a correct diagnosis and the necessary treatment. Remember, while costochondritis can be painful, it is typically not life-threatening and can be managed with proper care and treatment.
Diagnosis of Costochondritis
The diagnosis of costochondritis primarily involves a detailed evaluation to rule out other causes of chest pain and confirm the presence of cartilage inflammation. This process is critical as costochondritis symptoms often resemble those of more serious conditions, such as heart attacks or other heart-related problems. A thorough diagnostic approach ensures that the treatment plan addresses the specific needs of the patient, focusing on managing pain and reducing inflammation.
Medical Professionals Who Diagnose Costochondritis
Several types of healthcare providers are qualified to diagnose costochondritis, including:
- Primary Care Physicians (PCPs): Often the first point of contact, PCPs can assess symptoms, perform initial examinations, and refer patients to specialists if necessary.
- Rheumatologists: Specialists in musculoskeletal diseases and systemic autoimmune conditions, rheumatologists have a deep understanding of conditions like costochondritis.
- Orthopedists: Focusing on the musculoskeletal system, orthopedists can diagnose and treat costochondritis, especially when the pain affects the patient’s mobility or quality of life.
- Cardiologists: While not typically involved in the primary diagnosis of costochondritis, cardiologists may be consulted to rule out heart-related conditions when chest pain is a symptom.
Diagnostic Tests and Evaluations
The diagnosis of costochondritis involves a combination of physical exams, medical history reviews, and potentially imaging tests to rule out other conditions. Here’s a closer look at each component:
- Physical Exam: The cornerstone of costochondritis diagnosis, the physical exam focuses on identifying tenderness in the costosternal, costochondral, or costovertebral regions, which is a hallmark of the condition.
- Medical History: A comprehensive review of the patient’s medical history helps to identify potential risk factors, previous injuries, or activities that could contribute to costochondritis symptoms.
- Imaging Tests: While not always necessary, imaging tests such as chest X-rays, CT scans, or MRIs may be ordered to exclude other causes of chest pain, such as fractures, tumors, or heart conditions. These tests provide detailed images of the chest structure, offering invaluable insights into the patient’s condition.
This comprehensive approach ensures that patients receive a correct diagnosis, paving the way for effective treatment and relief from symptoms. Understanding the diagnostic process empowers patients to seek timely medical attention, contributing to better health outcomes.
Treatment Options for Costochondritis
Effective management of this condition involves a combination of home remedies, medical treatments, and alternative therapies. Here, we explore the various options available to alleviate the symptoms of costochondritis, aiming to provide sufferers with relief and an improved quality of life.
Home Remedies and Lifestyle Changes:
- Heat and Cold Therapy: Applying a heating pad or warm compress to the affected area several times a day can help reduce pain and inflammation. Alternatively, ice packs applied for short periods might also offer relief.
- Rest: Limiting physical activity that exacerbates the pain is crucial. It’s important to avoid heavy lifting and strenuous exercises until the pain subsides.
- Over-the-Counter Pain Relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin IB) or naproxen (Aleve) can help reduce inflammation and pain.
- Posture Improvement: Practicing good posture can alleviate pressure on the costosternal joints. Ergonomic adjustments to the workspace and being mindful of posture during daily activities can be beneficial.
- Stretching Exercises: Gentle stretching exercises, especially those focused on the chest and ribcage, can improve mobility and reduce discomfort.
Medical Treatments:
- Prescription Medications: For severe or persistent pain, doctors may prescribe stronger anti-inflammatory medications, muscle relaxants, or even certain antidepressants known to help manage chronic pain.
- Physical Therapy: A physical therapist can teach exercises specifically designed to stretch the chest and strengthen the muscles supporting the ribcage, which may help reduce symptoms.
- Corticosteroid Injections: In cases where the pain is severe and not responding to other treatments, a doctor might recommend an injection of corticosteroids directly into the affected area to reduce inflammation.
Alternative Therapies:
- Acupuncture: This ancient Chinese practice involves inserting thin needles into specific points on the body. It may help some people by reducing pain and inflammation.
- TENS (Transcutaneous Electrical Nerve Stimulation): A TENS unit delivers small electrical impulses through the skin, which can help alleviate pain in some individuals.
- Yoga and Tai Chi: These gentle forms of exercise can help improve posture, flexibility, and stress management, potentially reducing the symptoms of costochondritis.
It’s important for individuals suffering from this condition to consult with healthcare professionals to tailor a treatment plan that best suits their specific needs. With the right management strategies, most people can achieve a good quality of life despite the challenges posed by costochondritis.
Managing Pain and Recovery
Recovering from an injury or surgery can be a challenging journey, but understanding how to manage pain and navigate the recovery process can make a significant difference. Below, we offer insights into effective pain management techniques, what to expect during recovery, and when it’s crucial to seek further medical assistance.
Tips for Managing Pain During the Recovery Process
- Follow Your Doctor’s Advice: Adhering to the pain management plan prescribed by your healthcare provider is paramount. Whether it involves medication, physical therapy, or rest, following their guidance ensures a safer and more efficient recovery.
- Stay Active Within Limits: Gentle movements and exercises, as recommended by a physical therapist, can help maintain flexibility and strength without exacerbating pain. It’s crucial to understand your body’s limits and not push through severe pain.
- Use Ice and Heat Therapy: Applying ice to reduce inflammation and heat to relax muscles can be effective strategies for pain relief. Ensure to use these therapies as advised to avoid skin damage or other issues.
- Practice Relaxation Techniques: Mindfulness, meditation, and deep-breathing exercises can help reduce the perception of pain by calming the mind and body, promoting a sense of well-being.
- Stay Hydrated and Maintain a Balanced Diet: Proper nutrition and hydration support the body’s natural healing processes, potentially reducing recovery time and discomfort.
What to Expect During the Recovery Period
The recovery process can vary significantly depending on the nature of your injury or surgery. Generally, you can expect:
- Initial Pain and Discomfort: It’s normal to experience pain immediately after surgery or an injury. This should gradually improve over time.
- Fluctuations in Pain Levels: Pain levels can change based on activity levels, time of day, and recovery progress.
- Milestones in Recovery: Your healthcare provider may outline specific milestones, such as increased mobility or decreased pain levels, as indicators of recovery progress.
- The Importance of Rest: Adequate rest is crucial for recovery, even if it means adjusting your usual activity levels.
When to Seek Further Medical Help
While some discomfort during recovery is expected, there are certain signs that indicate the need for additional medical attention:
- Increased or Unmanageable Pain: If pain worsens or becomes unmanageable despite following your prescribed pain management plan, it’s important to consult with your healthcare provider.
- Signs of Infection: Redness, swelling, warmth at the site of surgery or injury, fever, or unusual drainage are signs of infection that require immediate medical attention.
- Limited Progress in Recovery: If you’re not noticing improvements or if recovery milestones are not being met, a reassessment of your recovery plan may be needed.
- New Symptoms: Any new symptoms or concerns that arise during the recovery process should be discussed with your healthcare provider to ensure they are not indicative of complications.
Navigating the recovery process requires patience, adherence to professional medical advice, and attentiveness to your body’s signals. By employing effective pain management strategies, setting realistic expectations for recovery, and knowing when to seek further help, you can support your body’s healing process and work towards a successful recovery.
Prevention of Costochondritis: Insights and Expert Opinions
Costochondritis, a condition characterized by inflammation of the cartilage that connects a rib to the sternum, can cause chest pain reminiscent of a heart attack. While the exact cause is often unknown, strategies focusing on lifestyle and exercise can potentially minimize the risk of its onset and recurrence. Here, we delve into preventive measures supported by insights and expert opinions.
Understanding the Basics
Before we explore prevention, understanding the triggers of costochondritis is crucial. Factors such as repetitive trauma or unusual physical activity can contribute to the development of this condition. In some cases, respiratory infections and overuse injuries from activities like heavy lifting or intense workouts can also lead to costochondritis.
Lifestyle Modifications
1. Maintain a Healthy Weight: Excess body weight can put additional stress on your chest and ribcage, exacerbating the risk of inflammation. A balanced diet and regular exercise can help manage weight and reduce this risk.
2. Good Posture: Poor posture, especially while sitting for prolonged periods, can strain the chest area. Practicing good posture helps in evenly distributing the stress across the body, thereby minimizing the strain on the cartilage connecting the ribs to the sternum.
3. Stress Management: Stress can have a physical impact on your body, including the tightening of muscles, which can exacerbate chest pain. Techniques such as deep breathing, meditation, and yoga can help manage stress levels.
Exercise Tips
1. Gradual Progression: When engaging in any physical activity or exercise routine, it’s important to gradually increase the intensity. This helps in avoiding sudden strain on the chest area, which could trigger costochondritis.
2. Stretching: Incorporating stretching exercises into your daily routine can improve flexibility and reduce the chances of muscle and cartilage strain. Focus on stretches that enhance chest and upper body flexibility.
3. Strength Training: Building strength in the chest and upper body can help support the ribcage, reducing the risk of costochondritis. However, it’s essential to perform these exercises under guidance to ensure they are done correctly and safely.
4. Avoid Repetitive Strain: Be mindful of activities that put repetitive strain on the chest area, such as certain sports or occupations. Taking regular breaks and varying your activities can help minimize this risk.
Expert Opinions
Experts agree that while it may not be possible to prevent costochondritis entirely, adopting a proactive approach towards maintaining overall health can significantly reduce the likelihood of its occurrence. Regular check-ups with a healthcare provider can also help identify and mitigate any potential risk factors early on.
However, a combination of lifestyle changes and mindful exercise practices can play a pivotal role in preventing costochondritis. By understanding the potential triggers and adopting preventive strategies, individuals can significantly reduce their risk of experiencing this painful condition. Remember, it’s always advisable to consult with a healthcare professional before starting any new exercise or wellness program.
When to See a Doctor for Costochondritis
Experiencing chest pain can be alarming, and it’s often challenging to determine its cause without professional help. Costochondritis, an inflammation of the cartilage that connects a rib to the sternum, can mimic the pain of a heart attack or other serious conditions. Although it is usually benign, understanding when to seek medical attention for chest pain related to costochondritis is crucial. This guide aims to provide clear guidelines on recognizing the signs that necessitate a visit to the doctor, emphasizing the importance of early diagnosis and treatment to prevent potential complications.
Recognizing the Symptoms of Costochondritis
Costochondritis typically presents as sharp, aching, or pressure-like pain in the chest, particularly in the upper ribs on one or both sides of the sternum. The pain may worsen with deep breathing, coughing, or physical activity. While these symptoms are characteristic of costochondritis, they are also common to several other more serious conditions, making it essential to discern when professional evaluation is necessary.
When to Seek Medical Attention
- Persistent or Severe Pain: If chest pain is severe, doesn’t improve with rest, or persists for several days, it’s time to see a doctor. Persistent pain may indicate a more severe condition or the need for targeted treatment to manage costochondritis symptoms.
- Difficulty Breathing: Experiencing shortness of breath or difficulty breathing alongside chest pain warrants immediate medical attention, as these symptoms can indicate serious heart or lung conditions.
- Pain Spreading: If the pain spreads to the arms, back, neck, or jaw, or is accompanied by symptoms such as dizziness, sweating, or nausea, seek emergency medical care. These signs could indicate a heart attack or other critical conditions.
- Fever or Signs of Infection: While rare, costochondritis can sometimes be associated with infection. If you experience fever, swelling, redness, or pus discharge in the chest area, contact your healthcare provider promptly.
- No Improvement with Home Care: If symptoms of costochondritis do not improve with home treatment methods like rest, heat application, or over-the-counter pain relievers within a week, a doctor’s visit is advisable.
The Importance of Early Diagnosis and Treatment
Early diagnosis and treatment of costochondritis are key to preventing potential complications, such as persistent pain that interferes with daily activities or the progression to chronic pain conditions. A healthcare provider can offer a comprehensive evaluation to rule out other causes of chest pain, provide effective treatment options, and offer guidance on managing symptoms.
However, while costochondritis is often not a cause for serious concern, it is important to be vigilant about chest pain and to understand when medical attention is necessary. By recognizing the symptoms and knowing when to seek help, you can ensure prompt treatment and minimize the impact of costochondritis on your health and well-being. Prioritizing your health by responding appropriately to chest pain not only aids in managing costochondritis but also helps in the early detection of more serious conditions, safeguarding your overall health.
FAQ Section: Understanding Costochondritis
What is costochondritis?
Costochondritis is an inflammation of the cartilage that connects a rib to the breastbone (sternum). This condition can cause chest pain that may be mistaken for a heart attack or other heart conditions, but it is not associated with the heart and is relatively harmless, though it can be uncomfortable or painful.
What causes costochondritis?
The exact cause of costochondritis is often unknown, but it can result from a variety of factors including physical trauma to the chest, repetitive strain (such as from heavy lifting or strenuous exercise), certain viral or bacterial infections, and arthritis. In many cases, costochondritis occurs without any identifiable reason.
How is costochondritis diagnosed?
Costochondritis is typically diagnosed through a physical examination. Your doctor will look for tenderness in the area where the ribs meet the breastbone. In some cases, further tests may be conducted to rule out other conditions that can cause similar symptoms, such as heart disease, other types of arthritis, or respiratory conditions.
What are the symptoms of costochondritis?
The primary symptom of costochondritis is chest pain, which can vary in intensity from mild to severe. The pain may be sharp, aching, or pressure-like and is often worsened by coughing, deep breathing, or physical activity. The pain is usually localized to the front of the chest but can spread to the back or abdomen.
How is costochondritis treated?
Treatment for costochondritis focuses on relieving pain and reducing inflammation. Options may include over-the-counter pain relievers such as ibuprofen or naproxen, heat or ice packs, and rest. Avoiding activities that worsen the pain is also recommended. In more severe cases, your doctor may prescribe stronger medications or physical therapy.
Can costochondritis go away on its own?
Yes, in many cases, costochondritis will resolve on its own without specific treatment. The condition can be persistent, lasting for weeks or even months, but it usually goes away gradually with rest and over-the-counter treatments to manage pain.
Is costochondritis a serious condition?
While costochondritis can cause significant discomfort, it is generally not considered a serious condition. It does not lead to any permanent damage to the heart or lungs. However, because chest pain can be a sign of more serious conditions, it is important to get a proper diagnosis from a healthcare provider.
Can exercise help with costochondritis?
Exercise can be beneficial for overall health, but it’s important to approach it cautiously if you have costochondritis. Low-impact activities and stretching exercises can help, but high-impact exercises or those that strain the chest area may worsen symptoms. It’s best to consult with a healthcare professional or a physical therapist to design a safe exercise plan.
Conclusion:
Accurate diagnosis is the cornerstone of effective treatment. It not only ensures that the pain is indeed due to costochondritis but also rules out other serious conditions that may mimic its symptoms. Once diagnosed, a tailored treatment plan, which may include pain management strategies, physical therapy, and lifestyle adjustments, can significantly reduce discomfort and improve daily functioning.
It cannot be overstated how important it is to consult with healthcare professionals when dealing with costochondritis. Self-diagnosis and treatment might not only be ineffective but could potentially exacerbate the condition. Healthcare providers can offer personalized advice and treatment plans based on the latest medical research and their clinical experience. They can guide you through the recovery process, adjusting treatments as necessary to ensure the best possible outcome.
In conclusion, if you or someone you know is experiencing chest pain that may be related to costochondritis, prompt action is advised. Seek professional medical advice to navigate your way to an accurate diagnosis and effective treatment. Remember, with the right approach, you can achieve relief from costochondritis and return to your daily activities without discomfort.