COVID-19 Treatment: In the wake of the global COVID-19 pandemic, understanding the nuances of diagnosis and treatment for this novel coronavirus has become paramount.
With the virus’s widespread impact, the medical community has been rapidly evolving its approach to combat the pandemic.
This comprehensive guide delves deep into the latest methodologies for diagnosing and treating COVID-19, offering insight into the frontline strategies being employed to mitigate the virus’s effects.
Understanding COVID-19
COVID-19, the illness caused by the SARS-CoV-2 virus, has affected millions worldwide since its emergence in late 2019. This disease can spread from person to person, primarily through respiratory droplets produced when an infected person coughs, sneezes, or talks. People can also contract the virus by touching surfaces or objects contaminated with the virus and then touching their face. Understanding the basics of the virus, its symptoms, risk factors, and possible complications is crucial for prevention and management.
Brief Description of the Virus (SARS-CoV-2) and How It Spreads
SARS-CoV-2 is a novel coronavirus that was first identified in Wuhan, China. It belongs to a large family of viruses known for causing respiratory illnesses. COVID-19 spreads mainly through close contact with an infected person. The virus can spread from an infected person’s mouth or nose in small liquid particles when they cough, sneeze, speak, sing, or breathe. These particles range from larger respiratory droplets to smaller aerosols, making it essential to maintain physical distancing, wear masks, and practice good hygiene.
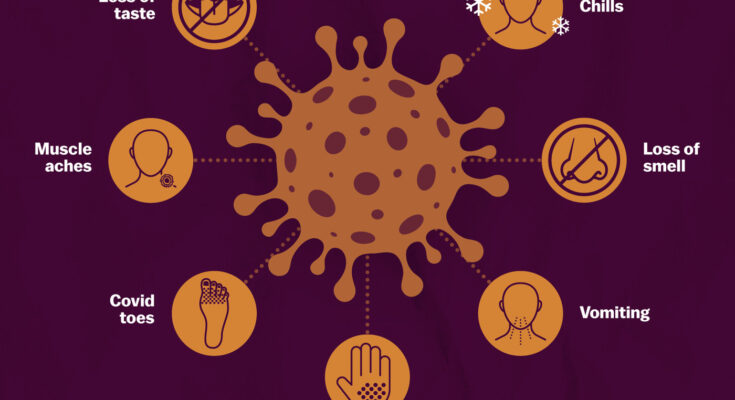
Symptoms of COVID-19
COVID-19 symptoms can vary from mild to severe and may appear 2-14 days after exposure to the virus. Common symptoms include:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
It’s important to monitor your health and seek medical attention if you experience symptoms, especially if they are severe or worsen.
Risk Factors and Complications Associated with COVID-19
Certain factors can increase the risk of severe illness from COVID-19, including:
- Older age, particularly those aged 65 and older
- Underlying medical conditions, such as heart or lung disease, diabetes, obesity, or a weakened immune system
Complications from severe COVID-19 can be serious and include:
- Pneumonia and trouble breathing
- Organ failure in severe cases
- Heart problems
- Acute kidney injury
- Additional viral and bacterial infections
- Long-term health effects, often referred to as “long COVID,” which can include a range of ongoing health problems
Preventive measures, such as vaccination, wearing masks, hand hygiene, and physical distancing, are crucial in reducing the spread of the virus and mitigating the risk of infection and complications.
By understanding the nature of SARS-CoV-2, recognizing the symptoms of COVID-19, being aware of the risk factors and potential complications, individuals can take informed steps to protect themselves and others. Staying informed through reliable sources and adhering to public health guidelines remains key in the fight against COVID-19.
Diagnosis of COVID-19
The diagnosis of COVID-19 is critical in managing and controlling the spread of this highly contagious virus. It involves identifying the presence of SARS-CoV-2, the virus responsible for COVID-19, in individuals through various testing methods. These tests are pivotal in ensuring early detection, treatment, and the isolation of infected individuals to prevent further transmission.
List of COVID-19 Testing Methods
- PCR Tests: Polymerase Chain Reaction (PCR) tests are considered the gold standard for detecting the virus’s genetic material. They are highly accurate and are performed in a laboratory setting.
- Antigen Tests: Also known as rapid tests, antigen tests detect specific proteins from the virus. They provide results more quickly than PCR tests but are generally less accurate.
- Antibody Tests: These tests look for antibodies produced in response to SARS-CoV-2 infection. They can help identify individuals who have been infected in the past but are not suitable for diagnosing an active infection.
- Saliva Tests: A less invasive testing method where samples are collected through saliva. While convenient, its availability and accuracy can vary.
- Home Testing Kits: These allow individuals to collect samples at home and either get results on the spot (antigen tests) or send the sample to a lab for processing (PCR tests).
Criteria for Getting Tested: Symptoms, Exposure, and Other Considerations
- Symptoms: Individuals experiencing symptoms such as fever, cough, difficulty breathing, loss of taste or smell, and fatigue should consider getting tested.
- Exposure: Those who have been in close contact with a confirmed COVID-19 case are advised to get tested, regardless of their symptom status.
- Other Considerations: Healthcare workers, individuals in high-risk settings, and those planning to travel may also need to undergo testing based on local health guidelines.
Steps to Take if You Test Positive for COVID-19
- Isolate Yourself: Stay away from others, including those in your household, to prevent the spread of the virus.
- Inform Close Contacts: Notify people you’ve been in close contact with so they can take appropriate precautions.
- Seek Medical Advice: Contact your healthcare provider for advice on managing your symptoms and when it’s safe to end isolation.
- Rest and Hydrate: Ensure you get plenty of rest, stay hydrated, and follow any treatment recommendations from your healthcare provider.
- Follow Public Health Guidelines: Adhere to any additional guidelines from your local public health authorities, which may include reporting your test results and participating in contact tracing efforts.
Understanding the importance of COVID-19 testing and following recommended actions upon testing positive are crucial steps in combating the pandemic. By staying informed and adhering to health guidelines, individuals can play a significant role in protecting themselves and their communities.
Treatment Options for COVID-19
As the virus continues to affect populations worldwide, understanding the available treatments is crucial for patients and healthcare providers alike. This article provides an overview of current FDA-approved treatments, emergency use authorizations, and the importance of supportive care at home.
FDA-Approved Treatments and Emergency Use Authorizations
The U.S. Food and Drug Administration (FDA) has approved and authorized various treatments for COVID-19, reflecting the evolving nature of the pandemic and the scientific community’s response. These treatments are primarily designed for hospitalized patients and range from antiviral drugs to immunotherapies.
Antiviral Drugs
Remdesivir, an antiviral drug, has emerged as a cornerstone in treating COVID-19. Approved by the FDA, it works by inhibiting the virus’s replication mechanism, offering a treatment pathway for patients with severe symptoms. Remdesivir’s approval underscores the progress in understanding and combating the virus at a molecular level.
Monoclonal Antibodies
Monoclonal antibodies represent a significant advancement in COVID-19 treatment, targeting the virus directly to prevent it from entering cells. These laboratory-made proteins mimic the immune system’s ability to fight off harmful pathogens. Emergency use authorizations have facilitated their use, especially for high-risk patients, to reduce the severity of the disease and hospitalization rates.
Corticosteroids
Dexamethasone, a corticosteroid, has been identified as an effective treatment for critically ill COVID-19 patients. By reducing inflammation and suppressing the immune system’s overreaction, dexamethasone can decrease mortality rates among those requiring oxygen or mechanical ventilation.
Investigational Treatments and Clinical Trials
Beyond approved treatments, numerous investigational drugs and therapies are undergoing clinical trials. These potential treatments, ranging from new antiviral medications to immune modulators, highlight the ongoing research efforts to find more effective and accessible COVID-19 therapies.
Importance of Supportive Care: Managing Symptoms at Home
For many patients with mild to moderate COVID-19 symptoms, home care remains a vital component of the treatment strategy. Supportive care focuses on relieving symptoms and includes hydration, rest, and over-the-counter medications to reduce fever and pain. Monitoring for symptom progression is crucial, as early hospitalization can be necessary for worsening conditions.
However, understanding the available treatment options for COVID-19, from hospital-based therapies to home care practices, is essential for navigating the pandemic. As research continues and new treatments emerge, staying informed about these developments will help patients and healthcare providers make informed decisions about care and treatment strategies.
Home Care and Management of Mild COVID-19
With the ongoing presence of COVID-19, understanding how to manage mild cases at home has become essential. If you or a loved one are experiencing symptoms of COVID-19 that are not severe, such as a mild fever, cough, or fatigue, there are effective steps you can take to care for yourselves while minimizing the risk of spreading the virus to others. This guide will provide you with essential guidelines for self-isolation, symptom management, and knowing when it’s critical to seek emergency medical attention.
Guidelines for Self-Isolation and Preventing the Spread within Households
- Stay in a Separate Room: If you have COVID-19, isolate yourself in a single room, away from other household members as much as possible. Use a separate bathroom if available.
- Limit Contact: Avoid sharing personal household items like dishes, towels, and bedding. If you must be in a shared space, wear a mask and maintain a distance of at least 6 feet from others.
- Enhance Ventilation: Improve the airflow in your home by opening windows or adjusting the air conditioning to increase outdoor air exchange.
- Practice Good Hygiene: Wash your hands frequently with soap and water for at least 20 seconds, especially after blowing your nose, coughing, or sneezing. Use hand sanitizer if soap and water are not readily available.
Symptom Management
- Fever and Pain Relief: Over-the-counter medications such as acetaminophen (Tylenol) or ibuprofen (Advil) can help reduce fever and alleviate pain. However, always follow the dosage instructions on the label or those given by your healthcare provider.
- Stay Hydrated: Drink plenty of fluids like water, herbal teas, or broth. Staying hydrated helps your body fight off the virus and recover more quickly.
- Get Adequate Rest: Your body needs energy to fight the virus. Ensure you’re getting enough sleep and resting throughout the day.
When to Seek Emergency Medical Attention
While managing COVID-19 at home, it’s crucial to monitor symptoms and recognize when they worsen, requiring medical intervention. Seek emergency medical attention if you or someone you’re caring for shows any of the following signs:
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Bluish lips or face
This is not an exhaustive list. Any severe or concerning symptoms should prompt an immediate call to your healthcare provider or emergency services.
Managing mild COVID-19 at home is primarily about taking care of yourself while protecting others. By following these guidelines, you can help mitigate the spread of the virus within your household and community, ensuring a safer environment for everyone. Remember, if your symptoms worsen or if you have concerns about your health, don’t hesitate to reach out to a healthcare professional for advice and assistance.
The Role of Vaccines in Prevention and Treatment
In the battle against the COVID-19 pandemic, vaccines have emerged as a crucial tool not only for prevention but also for managing the spread of the virus. Understanding the role of vaccines, particularly in the context of COVID-19, is essential for appreciating their impact on global health dynamics. This section delves into the overview of COVID-19 vaccines, their effectiveness, their contribution to managing the pandemic, and the critical importance of vaccination in preventing severe illness and reducing virus transmission.
Overview of COVID-19 Vaccines and Their Effectiveness
COVID-19 vaccines have been developed at an unprecedented pace, employing various technologies such as mRNA, viral vectors, and protein subunits. These vaccines work by training the immune system to recognize and fight the virus responsible for COVID-19, should the body be exposed to it. The effectiveness of these vaccines has been a subject of extensive research and real-world evidence, showing high efficacy rates in preventing COVID-19 infection, particularly severe cases that could lead to hospitalization or death.
How Vaccines Contribute to the Management of COVID-19
Vaccines contribute significantly to the management of COVID-19 by reducing the number of new infections and decreasing the likelihood of severe disease outcomes. By lowering the overall virus prevalence in the community, vaccines also reduce the burden on healthcare systems, allowing for better allocation of resources to treat other diseases and medical conditions. Furthermore, vaccination plays a pivotal role in mitigating the emergence of new variants by curtailing the virus’s ability to spread and mutate.
The Importance of Vaccination in Preventing Severe Illness and Reducing the Spread of the Virus
The importance of vaccination extends beyond individual protection. It is a key factor in achieving herd immunity, a situation where a sufficient portion of the population is immune to the virus, thereby reducing its spread. This collective immunity helps protect those who cannot be vaccinated, such as people with certain medical conditions or allergies to vaccine components. Vaccination against COVID-19 is particularly crucial for vulnerable populations, including the elderly and those with pre-existing health conditions, as it significantly decreases the risk of severe illness, hospitalizations, and death.
However, vaccines are indispensable in the fight against COVID-19, offering a beacon of hope for returning to normalcy. The widespread acceptance and administration of vaccines are pivotal in preventing severe illness, managing the pandemic, and moving towards the end of this global health crisis. As research continues and vaccine coverage expands, the role of vaccines in public health strategy will undoubtedly remain at the forefront of efforts to control and eventually eradicate COVID-19.
Navigating COVID-19 Treatment: Challenges and Considerations
The journey through the COVID-19 pandemic has been fraught with uncertainty, rapidly evolving information, and significant challenges in treatment protocols. As we continue to navigate these uncharted waters, it’s crucial to address the complexities surrounding COVID-19 treatment, including the accessibility of treatments, the impact of new variants on their efficacy, and the critical role of ongoing research and adaptation in our treatment strategies.
Access to Treatments: Global Disparities and Efforts to Improve Equity
One of the most pressing issues in the fight against COVID-19 is the stark disparity in access to treatments across different regions of the world. While wealthier nations have secured substantial quantities of antiviral drugs, vaccines, and other therapeutic options, lower-income countries have struggled to obtain these life-saving treatments. This inequality not only exacerbates the public health crisis in these regions but also poses a significant risk to global health by potentially allowing the virus to proliferate and mutate unchecked.
Efforts to improve equity in access to COVID-19 treatments have been ongoing, spearheaded by international collaborations and initiatives such as COVAX, aimed at facilitating vaccine distribution to countries in need. However, challenges persist due to logistical issues, vaccine hesitancy, and the complexities of scaling up production to meet global demand. Bridging this gap remains a paramount concern as we strive to combat the pandemic effectively.
The Impact of New COVID-19 Variants on Treatment Efficacy
The emergence of new COVID-19 variants has introduced another layer of complexity in the treatment landscape. Variants such as Delta and Omicron have shown the ability to partially evade the immunity provided by vaccines and previous infections, raising concerns about the efficacy of existing treatments. This constant evolution of the virus underscores the need for a dynamic approach to treatment, one that can quickly adapt to new challenges as they arise.
The development of variant-specific vaccines and booster shots has been a key strategy in maintaining the effectiveness of our treatment arsenal. Additionally, ongoing research into antiviral drugs that target broader aspects of the virus’s life cycle offers hope for more universally effective treatments, regardless of the variant.
The Importance of Ongoing Research and Adaptation of Treatment Strategies
The COVID-19 pandemic has highlighted the critical importance of flexibility and innovation in our approach to treatment. Ongoing research is vital to understanding the virus’s behavior, its impact on the body, and how it evolves over time. This knowledge informs the development of new treatments and the adaptation of existing ones to ensure they remain effective against the latest variants.
Collaboration across the global scientific community has accelerated the pace of discovery and implementation of COVID-19 treatments. Continuous monitoring of treatment outcomes, vaccine efficacy, and the emergence of new variants allows for rapid adjustments to treatment protocols. This adaptability will be key to staying ahead of the virus and ultimately bringing the pandemic under control.
However, navigating COVID-19 treatment requires a multifaceted approach that addresses the challenges of equitable access, the impact of emerging variants, and the need for ongoing research and adaptation. By focusing on these considerations, we can continue to make strides in our fight against the pandemic, ensuring that our treatment strategies are as effective and inclusive as possible.
FAQs: Understanding COVID-19 Diagnosis and Treatment Options
How is COVID-19 diagnosed?
COVID-19 is primarily diagnosed using RT-PCR (Reverse Transcription Polymerase Chain Reaction) tests, which detect the virus’s genetic material from a sample usually taken from a person’s nose or throat. Rapid antigen tests, which can provide results in minutes, are also used for screening purposes, though they are generally less accurate than RT-PCR tests. For a definitive diagnosis, healthcare providers may consider symptoms, exposure history, and test results.
What are the symptoms of COVID-19?
Symptoms of COVID-19 can vary widely, ranging from mild to severe illness. Common symptoms include fever, cough, shortness of breath, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting, and diarrhea. Symptoms may appear 2-14 days after exposure to the virus.
What should I do if I think I have COVID-19?
If you suspect you have COVID-19, it’s important to get tested as soon as possible. While waiting for test results, you should stay at home and isolate yourself from others, including those living in your household, to prevent the spread of the virus. If your symptoms are mild, you may be able to recover at home without medical care. However, if your symptoms worsen or if you have difficulty breathing, seek medical attention immediately.
Are there treatments available for COVID-19?
Yes, several treatments are available for COVID-19, depending on the severity of the illness. For mild cases, treatment focuses on relieving symptoms, such as fever and cough. More severe cases may require hospitalization and could include treatments like antiviral medications, steroids, and supportive care such as oxygen therapy. Vaccination is also a crucial tool in preventing COVID-19 and reducing the severity of the illness if infected.
Can COVID-19 be cured?
While there is no cure for COVID-19, most people who contract the virus recover with appropriate medical care. Recovery times can vary, with mild cases recovering in a few days to a couple of weeks, while more severe cases may require longer periods. Ongoing research is focused on developing more effective treatments and understanding the long-term impacts of the virus.
Is it safe to take over-the-counter (OTC) medication for COVID-19 symptoms?
Yes, over-the-counter medications can be used to help manage symptoms of COVID-19, such as fever, headache, and muscle pain. However, it’s important to follow the advice of a healthcare provider and the instructions on the medication’s label. Certain medications may not be suitable for everyone, especially if you have underlying health conditions or are taking other medications.
How can I prevent getting COVID-19?
The best way to prevent COVID-19 is by getting vaccinated and following public health guidelines. This includes wearing masks in crowded or indoor settings, practicing good hand hygiene, maintaining physical distance from others, and avoiding poorly ventilated spaces. Staying informed about the latest guidance from public health authorities is also crucial.
Conclusion
Looking ahead, the future of COVID-19 treatment and management appears promising. Ongoing research and development are continuously yielding new insights, leading to the refinement of therapeutic strategies and the discovery of more effective treatments. Moreover, advancements in vaccine technology and the adaptation of public health strategies to emerging variants underscore a dynamic and responsive approach to pandemic management.
As we move forward, the synergy between public compliance with health measures, the scientific community’s relentless pursuit of knowledge, and healthcare systems’ adaptability will be crucial in navigating the challenges posed by COVID-19. While uncertainties remain, the concerted efforts of the global community offer hope for a future where COVID-19 is a manageable health concern rather than a global crisis.
In conclusion, the importance of prompt diagnosis and effective treatment cannot be overstated, and the adherence to public health guidelines and vaccination remains our best defense against COVID-19. With continued vigilance, innovation, and cooperation, we can look forward to a future where we coexist with COVID-19, with minimized impact on our lives and health.