Coronary Artery Disease Treatment: Coronary Artery Disease (CAD), also known as ischemic heart disease, is a significant medical condition that affects millions globally.
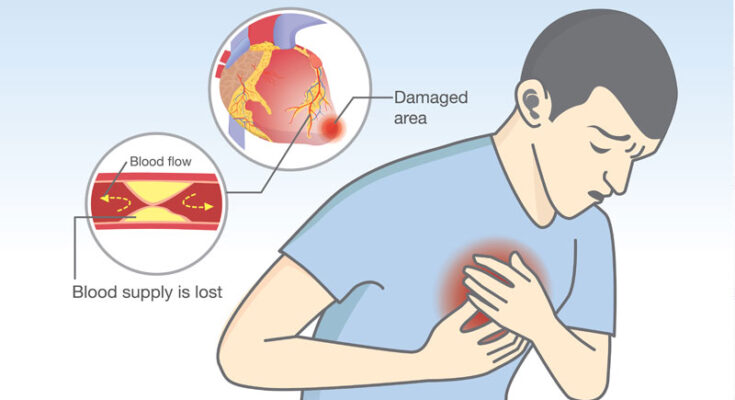
It occurs when the coronary arteries, responsible for supplying oxygen-rich blood to the heart muscle, become narrowed or blocked due to plaque buildup.
This article delves into the nuances of diagnosing and treating CAD, offering valuable insights for individuals seeking to understand this condition better.
What is Coronary Artery Disease?
Coronary Artery Disease (CAD), also known as ischemic heart disease, is a condition characterized by the impairment of blood flow to the heart muscle. This happens due to the narrowing or blockage of the coronary arteries – the blood vessels that supply blood to the heart itself. The primary cause of this narrowing is the buildup of fatty deposits, or plaques, on the artery walls, a process known as atherosclerosis. CAD can lead to serious health issues, including heart attacks, angina (chest pain), heart failure, and irregular heartbeats.
Causes of Coronary Artery Disease
The development of CAD is primarily attributed to atherosclerosis. The causes include:
- High levels of cholesterol and triglycerides in the blood, contributing to plaque buildup.
- High blood pressure, which can damage artery walls and speed up atherosclerosis.
- Smoking, which directly damages the interior walls of arteries, making them more susceptible to atherosclerosis.
- Insulin resistance or diabetes, which exacerbates the formation of plaques in the arteries.
Risk Factors Contributing to CAD
Several risk factors can increase the likelihood of developing CAD, including:
- Age: The risk increases with age, particularly after 65.
- Family history of heart disease, especially if it occurred at an early age.
- Sedentary lifestyle: Lack of exercise is linked with CAD and its risk factors.
- Obesity: Excess weight typically worsens other risk factors.
- Poor diet: Diets high in saturated fats, trans fats, sodium, and sugar can raise the risk.
- Excessive alcohol consumption: This can lead to elevated blood pressure and other heart disease risk factors.
The Impact of CAD on Heart Function
CAD can significantly impair heart function by reducing the heart’s ability to receive oxygen-rich blood. This can result in:
- Angina: Chest pain caused by reduced blood flow to the heart muscle.
- Heart attacks: Occur when a coronary artery is completely blocked.
- Heart failure: The heart’s inability to pump blood effectively can be a consequence of prolonged damage from CAD.
- Arrhythmias: Irregular heartbeats can result from damage to the heart tissue from CAD.
Statistics on Prevalence and Morbidity
CAD is one of the leading causes of death globally. According to the World Health Organization (WHO), it is responsible for an estimated 9 million deaths annually, making it a major public health concern. In the United States, the Centers for Disease Control and Prevention (CDC) reports that CAD is the most common type of heart disease, affecting about 18.2 million adults aged 20 and older. It’s also noted that about 2 in 10 deaths from CAD occur in adults less than 65 years old, highlighting its significant impact on morbidity and mortality rates across different age groups.
By understanding the causes, risk factors, and impact of CAD, individuals can take proactive steps towards heart health, potentially reducing the prevalence and severity of this condition through lifestyle changes and medical interventions.
Symptoms and Early Signs of Coronary Artery Disease
Understanding the symptoms and early signs of CAD is crucial for timely diagnosis and treatment, improving overall outcomes and quality of life. This article explores the common and atypical symptoms associated with CAD, emphasizing the importance of recognizing these early signs for prompt and effective management.
Common Symptoms Associated with CAD
The hallmark symptom of CAD is angina, a type of chest pain or discomfort that occurs when the heart muscle doesn’t receive enough oxygen-rich blood. Angina can feel like pressure, squeezing, fullness, or pain in the center of your chest. It may also radiate to your shoulders, arms, neck, jaw, or back. Other common symptoms of CAD include:
- Shortness of breath: This may occur when CAD has progressed enough to affect heart function, leading to difficulty breathing during routine activities.
- Fatigue: Feeling unusually tired, especially after physical activity, can be a subtle sign of CAD.
- Palpitations: Irregular heartbeats or a feeling of skipped beats can sometimes be associated with CAD.
- Nausea or indigestion: These symptoms are more common in women and may be mistaken for other conditions.
Understanding Atypical Symptoms and Their Significance
Not everyone with CAD experiences classic symptoms. Atypical symptoms are especially common in women, older adults, and people with diabetes, and they may include:
- Stomach pain or severe indigestion
- Unexplained weakness or dizziness
- Sweating without apparent reason
Recognizing these atypical symptoms is critical, as they often go unnoticed or are mistaken for less serious conditions, delaying diagnosis and treatment of CAD.
The Importance of Recognizing Early Signs for Timely Treatment
Early detection of CAD can significantly alter the course of the disease. By recognizing the early signs and symptoms, individuals can seek medical advice promptly, allowing for the initiation of treatment strategies that can slow disease progression, manage symptoms, and reduce the risk of heart attacks or strokes. Lifestyle modifications, medications, and in some cases, surgical interventions can be effectively employed to manage CAD when caught early.
Timely treatment not only improves survival rates but also enhances the quality of life by reducing symptoms and preventing complications. Awareness and education about the signs and symptoms of CAD play a vital role in early diagnosis and successful management of this common but potentially life-threatening condition.
However, understanding both common and atypical symptoms of Coronary Artery Disease is essential for early detection and timely treatment. Awareness campaigns and education on CAD symptoms are crucial for encouraging individuals to seek medical evaluation for any concerning signs, leading to earlier intervention and better health outcomes.
Diagnostic Approaches for Coronary Artery Disease (CAD)
Early and accurate diagnosis is crucial for effective management and treatment. Here, we explore the primary diagnostic approaches for CAD, emphasizing their roles and importance in assessing the condition.
Physical Examination and Patient History
The first step in diagnosing CAD involves a thorough physical examination and a detailed review of the patient’s medical history. During the examination, healthcare providers look for signs of heart disease, such as abnormal heart sounds, fluid retention, and changes in blood pressure. The patient’s history of symptoms, lifestyle factors (such as smoking and diet), family history of heart disease, and other health conditions provide essential clues for assessing the risk of CAD. This foundational step helps to guide further diagnostic testing.
Blood Tests and Biomarkers
Blood tests play a critical role in diagnosing CAD by measuring levels of certain biomarkers that indicate heart stress or damage. Key biomarkers include cholesterol levels, triglycerides, high-density lipoprotein (HDL), and low-density lipoprotein (LDL). Elevated levels of certain enzymes, such as troponin, can also signal a recent heart attack. These tests provide valuable information about the risk factors and presence of heart disease, guiding the need for more specialized tests.
Non-Invasive Imaging Techniques
Non-invasive imaging techniques are essential tools for visualizing the heart’s structure and function, helping to detect and evaluate CAD without the need for surgical procedures.
- Echocardiogram: This ultrasound test provides images of the heart’s chambers, valves, and surrounding structures, assessing the heart’s pumping action.
- Magnetic Resonance Imaging (MRI): MRI uses a magnetic field and radio waves to create detailed images of the heart and blood vessels, useful for identifying areas of muscle damage and blockages.
- Computed Tomography (CT) Scans: CT scans offer detailed cross-sectional images of the heart, allowing for the detection of calcified plaque in the coronary arteries.
These techniques are pivotal in assessing the severity and extent of CAD, aiding in the decision-making process for treatment.
Invasive Procedures
In certain cases, more invasive procedures are warranted to diagnose CAD accurately.
- Coronary Angiography: This procedure involves the injection of a contrast dye into the coronary arteries through a catheter, followed by X-ray imaging. It provides a clear view of blockages or narrowing in the arteries, offering critical information for planning interventions, such as angioplasty or coronary artery bypass grafting (CABG).
The Role of Each Diagnostic Method in Assessing CAD
Each diagnostic method contributes uniquely to the comprehensive assessment of CAD. Physical examinations and patient history lay the groundwork by identifying potential risk factors and symptoms. Blood tests and biomarkers further refine risk assessment and detect early signs of heart stress or damage. Non-invasive imaging techniques offer a detailed view of the heart’s structure and function, identifying areas affected by CAD. Invasive procedures like coronary angiography provide definitive information on the location and severity of arterial blockages, guiding therapeutic decisions.
Together, these diagnostic approaches enable healthcare providers to accurately diagnose CAD, assess the disease’s severity, and tailor treatment plans to individual patients, improving outcomes and quality of life.
Treatment Options for Coronary Artery Disease
Effective management and treatment of CAD are crucial to improve quality of life and reduce the risk of heart attack or stroke. Treatment options for CAD are multifaceted, ranging from lifestyle modifications to advanced surgical interventions. Tailoring these treatments to individual patient needs is essential for optimal outcomes. Below, we explore the various treatment avenues for CAD, emphasizing their importance and how they contribute to comprehensive care.
Lifestyle Modifications and Risk Factor Management
The foundation of managing and treating Coronary Artery Disease involves lifestyle changes and risk factor management. Adopting a heart-healthy lifestyle can significantly lower the progression of CAD. Key recommendations include:
- Healthy Eating: Adopting a diet low in saturated fats, cholesterol, and sodium while rich in fruits, vegetables, whole grains, and lean protein.
- Regular Physical Activity: Engaging in at least 150 minutes of moderate aerobic exercise or 75 minutes of vigorous exercise per week.
- Weight Management: Achieving and maintaining a healthy weight to reduce heart strain and improve overall health.
- Smoking Cessation: Avoiding tobacco in all forms, as smoking significantly increases the risk of CAD.
- Moderating Alcohol Consumption: Limiting alcohol intake to moderate levels.
Pharmacological Treatments
Medications play a critical role in managing CAD by controlling symptoms and reducing the risk of heart attacks. The main classes of drugs used include:
- Antiplatelet Agents: Drugs like aspirin reduce the risk of blood clots, a common cause of heart attacks and strokes.
- Cholesterol-lowering Medications: Statins are the most common drugs used to lower LDL (bad) cholesterol levels, thereby reducing the risk of plaque buildup in the arteries.
- Beta-blockers and Other Blood Pressure Medications: These drugs help lower blood pressure, reducing the heart’s workload and minimizing the risk of further heart damage.
- Angiotensin-converting Enzyme (ACE) Inhibitors: ACE inhibitors can help improve heart function and lower blood pressure, crucial for people with CAD.
Non-pharmacological Interventions
In cases where medication and lifestyle adjustments are insufficient to control CAD, non-pharmacological interventions may be necessary, such as:
- Coronary Angioplasty and Stent Placement: This procedure involves the insertion of a small balloon to open up the clogged artery, often followed by the placement of a stent to keep the artery open.
- Coronary Artery Bypass Grafting (CABG): In this surgical procedure, arteries or veins from other parts of the body are used to bypass the blocked coronary arteries, improving blood flow to the heart.
Emerging Treatments and Therapies
Research into CAD is ongoing, with new treatments and therapies under development. These include gene therapy, novel drug therapies, and advanced stenting techniques. Staying informed about these emerging options can provide additional avenues for treatment in the future.
The Importance of Individualized Treatment Plans
Every patient’s journey with CAD is unique, necessitating personalized treatment plans. Factors such as the severity of the disease, underlying health conditions, and personal preferences play a significant role in determining the most effective treatment approach. Regular consultations with healthcare providers, including cardiologists, dietitians, and physical therapists, are essential to tailor treatments to individual needs, ensuring the best possible outcomes.
However, the treatment of Coronary Artery Disease involves a comprehensive approach that includes lifestyle modifications, pharmacological treatments, non-pharmacological interventions, and staying abreast of emerging therapies. An individualized treatment plan, developed in close collaboration with healthcare professionals, is paramount to managing CAD effectively, enhancing quality of life, and reducing the risk of serious complications.
Living with Coronary Artery Disease (CAD)
Living with Coronary Artery Disease (CAD) requires a comprehensive approach to manage and mitigate its effects on your health. CAD, a condition characterized by the narrowing of the coronary arteries due to plaque buildup, can lead to serious heart issues if not properly managed. However, with the right lifestyle changes, regular monitoring, and support for emotional and mental health, individuals with CAD can lead fulfilling lives. Below, we discuss strategies for managing CAD effectively.
Lifestyle Changes for Managing CAD
- Adopt a Heart-Healthy Diet: Emphasize a diet rich in fruits, vegetables, whole grains, and lean proteins. Limit intake of saturated fats, cholesterol, sodium, and added sugars. Consider incorporating foods high in omega-3 fatty acids, like salmon and walnuts, which can help reduce artery inflammation.
- Maintain Regular Physical Activity: Aim for at least 150 minutes of moderate aerobic exercise or 75 minutes of vigorous exercise each week. Exercise helps improve heart muscle function and promotes weight management. Always consult with your healthcare provider before starting a new exercise regimen.
- Quit Smoking and Limit Alcohol: Smoking cessation is crucial as it directly contributes to coronary artery damage and exacerbates CAD. Limiting alcohol consumption can also reduce your risk factors.
- Manage Stress: Chronic stress can negatively impact your heart health. Techniques such as mindfulness, meditation, and deep breathing exercises can help manage stress levels.
- Monitor Weight and Maintain a Healthy Body Mass Index (BMI): Overweight and obesity are risk factors for CAD. Achieving and maintaining a healthy weight through diet and exercise is key.
Regular Monitoring and Follow-Up Care
- Routine Check-Ups: Regular visits to your healthcare provider are essential for monitoring the progression of CAD and adjusting treatment plans as necessary.
- Medication Adherence: If prescribed, it’s important to take medications as directed to manage symptoms and prevent complications. This may include statins, blood pressure medications, or aspirin.
- Monitoring Blood Pressure and Cholesterol Levels: Keeping these numbers in check is crucial for preventing further artery damage.
- Cardiac Rehabilitation: Participation in a cardiac rehabilitation program may be recommended to improve cardiovascular health through supervised exercise and education on heart-healthy living.
Coping with Emotional and Mental Health Impacts
- Seek Support: Living with CAD can be challenging, not just physically but also emotionally. It’s important to seek support from friends, family, or support groups where experiences and coping strategies can be shared.
- Professional Help: Consulting a mental health professional can be beneficial in dealing with feelings of anxiety, depression, or stress that often accompany chronic conditions like CAD.
- Stay Informed: Understanding your condition and being an active participant in your treatment can help alleviate fears and uncertainties.
- Find Enjoyable Activities: Engaging in hobbies and activities that bring joy can improve quality of life and reduce stress.
Living with Coronary Artery Disease requires a multifaceted approach, focusing on lifestyle changes, regular medical care, and emotional support. By adopting these strategies, individuals with CAD can manage their condition effectively and enjoy a healthier, more active life.
Prevention and Risk Reduction Strategies for Coronary Artery Disease
By adopting a few key lifestyle changes and engaging in regular medical check-ups, individuals can significantly reduce their risk of developing CAD. In this article, we’ll explore effective prevention and risk reduction strategies, focusing on the role of diet, exercise, smoking cessation, and the importance of regular medical check-ups for at-risk individuals.
Embracing a Heart-Healthy Diet
A heart-healthy diet is crucial in the prevention of coronary artery disease. This diet focuses on the intake of whole foods, rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Foods high in omega-3 fatty acids, like salmon and flaxseeds, are especially beneficial for heart health. Conversely, it’s important to limit the intake of processed foods, sugars, and saturated fats. Adopting a Mediterranean or DASH (Dietary Approaches to Stop Hypertension) diet can also contribute to heart health by lowering blood pressure and cholesterol levels, key risk factors for CAD.
Prioritizing Regular Exercise
Regular physical activity is another pillar of CAD prevention. The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week for adults. Exercise helps maintain a healthy weight, reduces blood pressure and cholesterol levels, and strengthens the heart muscle. Even simple activities like walking, cycling, or swimming can have profound benefits for heart health.
The Critical Role of Smoking Cessation
Smoking is a major risk factor for coronary artery disease. It damages the lining of the arteries, leading to the build-up of plaque, which can eventually block these arteries. Quitting smoking can dramatically reduce the risk of CAD. Within just one year of quitting, the risk of heart disease drops to about half that of a smoker. It’s never too late to quit, and there are numerous resources available to help individuals stop smoking, including nicotine replacement therapy, counseling, and support groups.
Importance of Regular Medical Check-Ups
For individuals at risk of CAD, regular medical check-ups are essential. These check-ups can help detect risk factors such as high blood pressure, high cholesterol, and diabetes early on. Early detection allows for timely intervention, such as lifestyle changes or medication, to manage these conditions effectively before they can lead to coronary artery disease. At-risk individuals should work closely with their healthcare provider to monitor their heart health and adjust their prevention strategies as needed.
Preventing coronary artery disease involves a holistic approach that includes a heart-healthy diet, regular exercise, smoking cessation, and regular medical check-ups. By taking proactive steps towards a healthier lifestyle, individuals can significantly reduce their risk of CAD and enjoy a longer, healthier life. Remember, prevention is always better than cure, and it’s never too early or too late to start taking care of your heart.
Conclusion
Understanding the significance of diagnosing and treating Coronary Artery Disease (CAD) effectively is paramount to improving overall heart health and preventing potentially life-threatening complications. CAD, a leading cause of heart attacks, requires prompt and accurate diagnosis to tailor the most effective treatment plan for each individual. Advancements in medical science have brought forth innovative diagnostic tools and treatments, yet early detection remains a critical factor in achieving the best outcomes.
If you suspect that you might be at risk for CAD, or if you experience symptoms such as chest pain, shortness of breath, or extreme fatigue, it is crucial to seek medical advice immediately. Consulting with a healthcare professional can provide you with the necessary evaluation and guidance to manage your condition effectively. Remember, early intervention can significantly reduce the risk of severe heart events and improve your quality of life.
Looking towards the future, the outlook on advancements in coronary artery disease treatment is promising. With ongoing research and technological innovations, we anticipate the development of even more precise diagnostic tools and minimally invasive treatment options. These advancements aim to enhance patient outcomes, reduce recovery times, and offer more personalized approaches to managing CAD.
In conclusion, the journey towards combating Coronary Artery Disease is an ongoing one, with each step forward in diagnosis and treatment bringing us closer to better heart health. Encouragement for individuals to proactively seek medical advice and stay informed about the latest in heart care is crucial. As we look ahead, the future of CAD treatment holds great potential for further improving the lives of those affected by this condition.