Coronary Artery Disease Symptoms: Coronary Artery Disease (CAD) stands as the foremost cause of death globally, affecting millions each year.
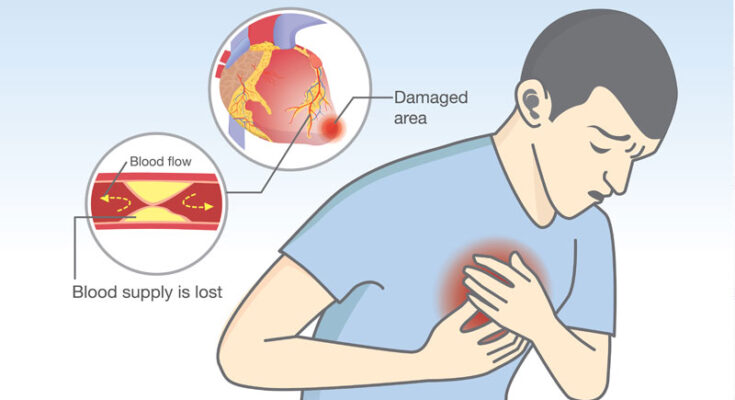
This condition, characterized by the narrowing or blockage of the coronary arteries, leads to a significant reduction in blood flow to the heart muscle, ultimately increasing the risk of heart attack and other heart-related complications.
Understanding its symptoms and causes is paramount for early detection and effective management.
What is Coronary Artery Disease (CAD)
Coronary Artery Disease (CAD), also known as coronary heart disease, is a significant medical condition that directly impacts heart function and overall cardiovascular health. This article aims to provide a comprehensive understanding of CAD, focusing on how it affects heart function, the role of atherosclerosis in its development, and an overview of its prevalence and impact.
How CAD Affects Heart Function
Coronary Artery Disease primarily affects the heart’s function by reducing the flow of oxygen-rich blood to the heart muscle itself. This reduction is often the result of a buildup of plaque—a combination of fat, cholesterol, calcium, and other substances found in the blood—within the coronary arteries. These arteries are crucial as they supply the heart muscle (myocardium) with the blood it needs to function effectively. When these arteries are narrowed or blocked due to plaque accumulation, the heart cannot receive the adequate blood supply it requires, leading to symptoms such as chest pain (angina), shortness of breath, or, in more severe cases, a heart attack.
The Role of Atherosclerosis in CAD Development
Atherosclerosis plays a central role in the development of Coronary Artery Disease. It begins with damage to the inner layer of a coronary artery, which can be caused by various factors, including high blood pressure, smoking, diabetes, or high levels of cholesterol in the blood. Once the artery wall is damaged, plaques begin to form at the site of injury in a process that can be slow and progressive. Over time, these plaques can harden or rupture. When a plaque ruptures, a blood clot can form on its surface, potentially blocking the flow of blood through the coronary artery and leading to a heart attack.
Statistics on CAD Prevalence and Impact
Coronary Artery Disease is one of the leading causes of death worldwide, affecting millions of individuals annually. According to the World Health Organization (WHO), CAD is responsible for an estimated 9 million deaths each year, making it a major public health concern. In the United States alone, the Centers for Disease Control and Prevention (CDC) reports that CAD is the most common type of heart disease, with approximately 18.2 million adults aged 20 and older diagnosed with the condition. This staggering prevalence underscores the significant impact of CAD on public health, highlighting the importance of prevention, early detection, and management strategies to combat this disease.
Symptoms of Coronary Artery Disease (CAD)
Recognizing the symptoms of CAD is crucial for early detection and management. Below is a detailed list of common symptoms associated with CAD, an explanation of how symptoms may vary between individuals, including differences by gender, and warning signs that require immediate medical attention.
Common Symptoms of CAD
- Chest Pain or Discomfort (Angina): Often described as a feeling of pressure, tightness, or squeezing in the center of the chest. It may also be felt in the neck, jaw, shoulder, arms, or back.
- Shortness of Breath: Difficulty breathing, especially during physical activity or when lying down, can be a sign of CAD as the heart struggles to pump blood efficiently.
- Fatigue: Unexplained tiredness or exhaustion, particularly during activities that used to be manageable, can indicate reduced blood flow to the heart.
- Palpitations: Irregular heartbeats or a feeling of the heart racing or fluttering can occur when the heart is deprived of oxygen-rich blood.
- Nausea or Indigestion: These symptoms can be more common in women and may sometimes be mistaken for non-cardiac conditions.
- Dizziness or Lightheadedness: Feeling dizzy or lightheaded can happen if the brain isn’t receiving enough blood, possibly due to narrowing of the coronary arteries.
Variation in Symptoms Between Individuals
The manifestation of CAD symptoms can significantly vary between individuals, influenced by factors such as age, gender, and overall health. Importantly, gender differences are notable:
- Men are more likely to experience classic symptoms like chest pain and pressure.
- Women may have subtler symptoms, such as fatigue, nausea, and shortness of breath, which are often overlooked or misattributed to non-cardiac causes.
Understanding these differences is vital for early recognition and intervention, as symptoms in women are sometimes less recognized as signs of heart disease.
Warning Signs Requiring Immediate Medical Attention
Some symptoms of CAD are critical and warrant immediate medical attention. These include:
- Severe Chest Pain: Especially if it lasts more than a few minutes or is accompanied by other symptoms like shortness of breath, sweating, or nausea.
- Sudden Onset of Symptoms: Such as severe shortness of breath, fainting, or dizziness.
- Heart Attack Symptoms: These can encompass chest discomfort with or without arm or jaw pain, unusual fatigue, and a cold sweat.
If you or someone you know experiences these warning signs, seek emergency medical care immediately. Early intervention can be lifesaving.
Causes and Risk Factors for Coronary Artery Disease
Understanding the causes and risk factors associated with CAD is essential for prevention and management. This article delves into the various factors leading to the development of CAD, emphasizing the importance of awareness and lifestyle adjustments.
High Cholesterol Levels
Elevated cholesterol levels in the blood are a primary cause of CAD. Cholesterol can accumulate on the artery walls, forming plaques that narrow and harden the arteries, impeding blood flow to the heart. Managing cholesterol levels through diet, exercise, and medication is crucial for heart health.
High Blood Pressure
High blood pressure, or hypertension, exerts extra force against the artery walls, accelerating the hardening and narrowing process (atherosclerosis) associated with CAD. Regular monitoring and controlling blood pressure levels can significantly reduce the risk of developing CAD.
Smoking
Smoking is a major risk factor for CAD. It damages the lining of the arteries, leading to the accumulation of fatty substances and plaque formation. Quitting smoking can dramatically lower the risk of CAD and improve overall heart health.
Diabetes
Individuals with diabetes, particularly type 2 diabetes, are at a higher risk of developing CAD. High blood sugar levels can damage arteries over time, contributing to the plaque buildup. Managing diabetes through lifestyle changes and medication can help mitigate this risk.
Sedentary Lifestyle
A sedentary lifestyle, characterized by minimal physical activity, contributes to the development of CAD. Regular exercise helps improve heart health by controlling weight, reducing blood pressure, and improving cholesterol levels.
Genetic Predisposition
Genetics play a significant role in the risk of developing CAD. Individuals with a family history of heart disease are more likely to develop CAD. While genetic predisposition cannot be changed, understanding one’s risk can encourage proactive measures for heart health.
Environmental and Lifestyle Factors
Beyond genetics, environmental and lifestyle factors significantly impact the risk of CAD. Unhealthy diets, excessive alcohol consumption, stress, and pollution can all contribute to the development of heart disease. Adopting a heart-healthy lifestyle, including a balanced diet, regular exercise, and stress management, is key to reducing the risk of CAD.
However, coronary artery disease is influenced by a combination of genetic, environmental, and lifestyle factors. While some risk factors, such as genetics, cannot be altered, many can be managed through lifestyle changes and medical interventions. Awareness and proactive management of these risk factors are essential steps in preventing the onset and progression of CAD. By adopting healthier habits and seeking regular medical advice, individuals can significantly reduce their risk of developing coronary artery disease, leading to a healthier, more vibrant life.
Diagnosing Coronary Artery Disease
Recognizing and diagnosing CAD promptly can lead to more effective management and treatment options, ultimately improving patient outcomes. This section explores the various diagnostic tests and procedures used to identify CAD and highlights the importance of early detection.
Diagnostic Tests and Procedures for CAD
Healthcare providers use several diagnostic tests and procedures to detect and evaluate the extent of coronary artery disease. These tests help in assessing the presence of blockages or narrowing in the coronary arteries that could lead to heart attacks or other cardiovascular complications. Here’s a comprehensive list:
- Electrocardiogram (ECG or EKG): An ECG records the electrical activity of the heart. It can identify irregular heart rhythms, areas of damage, and other heart conditions that may suggest CAD.
- Echocardiogram: This ultrasound test provides images of the heart’s chambers and valves, showing how well the heart pumps blood and identifying areas of poor blood flow.
- Stress Test: Also known as an exercise test or treadmill test, it measures how well the heart functions under physical stress. It can reveal problems with blood flow within the heart.
- Coronary Angiography and Cardiac Catheterization: This invasive procedure involves threading a thin tube through a blood vessel to the heart. A special dye injected into the arteries makes them visible on X-rays, identifying blockages.
- Computed Tomography Angiography (CTA): A non-invasive test that uses CT imaging to visualize the coronary arteries. It can detect plaque buildup and blockages.
- Magnetic Resonance Angiography (MRA): This test uses magnetic resonance imaging (MRI) to provide detailed images of the heart and blood vessels, assessing their health and functionality.
- Blood Tests: Certain blood tests can measure levels of cholesterol, triglycerides, and other substances in the blood, which may indicate an increased risk of CAD.
Importance of Early Detection
Early detection of CAD is crucial for several reasons:
- Prevention of Heart Attacks: Identifying CAD early can help prevent heart attacks by allowing for timely intervention and management of risk factors.
- Improved Management: Early detection enables healthcare providers to implement lifestyle changes and medications that can slow the progression of the disease.
- Better Prognosis: Patients diagnosed early with CAD generally have a better prognosis, as treatments can be more effective before the disease advances.
- Reduced Healthcare Costs: Early intervention can reduce the need for more expensive and invasive treatments later on, such as coronary artery bypass surgery or stent placement.
However, diagnosing Coronary Artery Disease involves a combination of clinical evaluation, diagnostic tests, and procedures that together provide a comprehensive view of a patient’s heart health. The importance of early detection cannot be overstated, as it plays a pivotal role in managing the disease effectively, preventing complications, and ensuring a better quality of life for patients. By understanding the available diagnostic options and the significance of early intervention, individuals can take proactive steps towards maintaining heart health and mitigating the risks associated with CAD.
Preventing Coronary Artery Disease (CAD)
With the right strategies and lifestyle changes, the risk of developing CAD can be significantly reduced. In this comprehensive guide, we will delve into effective measures, including diet and nutrition tips, exercise recommendations, smoking cessation, managing chronic conditions, and the critical role of regular check-ups and screenings, especially for those at higher risk.
Diet and Nutrition Tips
A heart-healthy diet plays a pivotal role in preventing CAD. Incorporating a variety of nutritious foods into your daily meals can help manage your weight, reduce cholesterol levels, and lower blood pressure. Key dietary recommendations include:
- Fruits and Vegetables: Aim for a colorful variety of fruits and vegetables. They are rich in vitamins, minerals, fiber, and antioxidants, which help protect your heart.
- Whole Grains: Choose whole-grain bread, pasta, and cereals over refined products. Whole grains provide essential fiber, helping to regulate blood pressure and heart health.
- Lean Proteins: Opt for lean protein sources like poultry, fish, beans, and nuts. Fish such as salmon and mackerel are high in omega-3 fatty acids, which have been shown to lower the risk of heart disease.
- Limit Unhealthy Fats: Reduce intake of saturated and trans fats found in red meat and processed foods. Instead, focus on healthy fats from avocados, olive oil, and nuts.
Exercise Recommendations
Regular physical activity is crucial for maintaining a healthy heart. Exercise helps improve cardiovascular fitness, reduce high blood pressure, and maintain a healthy weight. Aim for at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous aerobic activity per week, along with muscle-strengthening exercises on two or more days per week. Activities can include walking, jogging, cycling, swimming, or any other form of exercise that increases your heart rate.
Smoking Cessation
Smoking is a major risk factor for developing CAD. Quitting smoking can drastically reduce the risk of heart disease, as well as improve overall health. Seek support through cessation programs, counseling, or medication approved for smoking cessation. It’s never too late to quit, and the benefits begin the moment you stop.
Managing Chronic Conditions
Chronic conditions such as diabetes, high blood pressure, and high cholesterol can increase the risk of CAD. Managing these conditions through medication, lifestyle changes, and regular monitoring can significantly lower your risk. Work closely with your healthcare provider to develop a management plan that’s right for you.
Importance of Regular Check-ups and Screenings
Regular check-ups and screenings are essential for identifying risk factors and early signs of CAD, especially for individuals at higher risk. These may include people with a family history of heart disease, smokers, individuals with high blood pressure, cholesterol, or diabetes, and those leading a sedentary lifestyle. Regular monitoring allows for timely interventions to prevent the progression of the disease.
By adopting these strategies and making conscious lifestyle changes, individuals can significantly reduce their risk of developing Coronary Artery Disease. Remember, prevention is always better than cure. Start taking steps today towards a healthier heart and a longer, more vibrant life.
Treatment Options for Coronary Artery Disease
These treatments range from medications and surgical interventions to lifestyle modifications and cardiac rehabilitation. Understanding these options can empower individuals to work with their healthcare providers to develop a comprehensive treatment plan tailored to their needs.
Medications
Medications play a pivotal role in managing Coronary Artery Disease. They aim to alleviate symptoms, improve heart function, and prevent future heart events. Commonly prescribed medications include:
- Statins: Lower cholesterol levels in the blood, reducing plaque buildup in the arteries.
- Beta-blockers: Decrease heart rate and blood pressure, reducing the heart’s workload.
- Angiotensin-converting enzyme (ACE) inhibitors: Help relax blood vessels, improving blood flow and decreasing blood pressure.
- Antiplatelet drugs: Prevent blood clots from forming, reducing the risk of heart attacks.
Each medication targets specific aspects of the disease, and a combination of these drugs may be used to achieve the best outcomes.
Surgical Interventions
For cases where medications and lifestyle changes are not sufficient, surgical interventions may be necessary. These procedures aim to restore blood flow to the heart muscle. The most common surgeries include:
- Angioplasty with Stent Placement: A minimally invasive procedure where a small balloon is inflated inside the narrowed artery to widen it, often followed by placing a stent to keep the artery open.
- Coronary Artery Bypass Grafting (CABG): A more invasive surgery where blood vessels from other parts of the body are used to bypass blocked arteries, improving blood flow to the heart muscle.
These surgical options can significantly reduce symptoms, such as chest pain, and improve the overall quality of life.
Lifestyle Modifications
Lifestyle modifications serve as the cornerstone of treatment for Coronary Artery Disease. These changes aim to tackle the root causes of the disease and include:
- Healthy Eating: Adopting a diet low in saturated fats, cholesterol, and sodium while rich in fruits, vegetables, and whole grains.
- Regular Exercise: Engaging in moderate-intensity aerobic activity for at least 150 minutes per week.
- Quitting Smoking: Smoking cessation is crucial as it significantly reduces the risk of further heart damage.
- Maintaining a Healthy Weight: Losing weight and keeping it off can significantly reduce the burden on the heart.
These modifications not only help manage CAD but also improve overall health and well-being.
Cardiac Rehabilitation
Cardiac rehabilitation is a personalized program that includes exercise training, education on heart-healthy living, and counseling to reduce stress and improve mental health. It plays a vital role in the recovery and long-term maintenance of heart health for individuals who have undergone surgery or experienced a heart attack. The goal of cardiac rehabilitation is to help patients regain strength, prevent their condition from worsening, and reduce the risk of future heart events.
However, the treatment of Coronary Artery Disease involves a multifaceted approach that includes medications, surgical interventions, lifestyle changes, and cardiac rehabilitation. Each treatment option has its objectives, focusing on relieving symptoms, preventing complications, and improving the quality of life. By working closely with their healthcare team, individuals can develop a treatment plan that best suits their condition and lifestyle, leading to better heart health and a reduced risk of future heart-related issues.
Conclusion
In this article, we’ve explored the essential aspects of Coronary Artery Disease (CAD), focusing on its symptoms and causes. We’ve learned that CAD is a significant health condition characterized by the narrowing of coronary arteries, which can lead to chest pain, shortness of breath, and even heart attacks. Factors contributing to CAD include high cholesterol, high blood pressure, smoking, diabetes, obesity, and a sedentary lifestyle.
Understanding these symptoms and causes is the first step towards proactive heart health management. It’s crucial to recognize the importance of maintaining a healthy lifestyle, which includes regular exercise, a balanced diet, and avoiding tobacco use. Additionally, managing underlying conditions such as hypertension and diabetes is essential in preventing the development or progression of CAD.
We encourage our readers not to overlook the signs and symptoms associated with Coronary Artery Disease. Early detection and intervention can significantly impact your health outcome. Therefore, if you have any concerns about your heart health or if you’re experiencing symptoms that could be related to CAD, it’s imperative to seek professional medical advice immediately. A healthcare provider can offer personalized recommendations and treatment plans to manage your condition effectively.
Remember, taking proactive steps towards managing your heart health is not just about preventing disease; it’s about ensuring a quality of life that allows you to enjoy the moments that matter most. Stay informed, stay healthy, and never hesitate to reach out for help when you need it.