Congenital Heart Defects in Children Treatment: Congenital heart defects (CHDs) are the most common type of birth defect, affecting millions of infants worldwide. These conditions are present at birth and can affect the structure of a child’s heart and the way it works.
From mild defects that require no treatment to complex abnormalities that necessitate sophisticated medical interventions, CHDs encompass a wide spectrum of disorders.
Understanding the diagnosis and treatment options for congenital heart defects is crucial for parents, caregivers, and healthcare providers to ensure affected children can lead healthy, fulfilling lives.
What are Congenital Heart Defects?
Congenital heart defects (CHDs) are the most common type of birth defect, affecting the structure of a baby’s heart and the way it works. These defects are present at birth and can affect the walls of the heart, the valves of the heart, and the arteries and veins near the heart. They can disrupt the normal flow of blood through the heart, leading to a variety of health issues. CHDs can range from simple conditions that cause no symptoms to complex issues that cause severe, life-threatening symptoms.
Types of Congenital Heart Defects
There are many different types of congenital heart defects, ranging from mild to severe. Some of the most common include:
- Atrial Septal Defect (ASD): A hole in the wall between the two upper chambers of the heart (atria).
- Ventricular Septal Defect (VSD): A hole in the wall between the two lower chambers of the heart (ventricles).
- Tetralogy of Fallot: A complex heart defect that involves four heart defects present at birth.
- Pulmonary Valve Stenosis: A condition where the flow of blood from the heart to the lungs is obstructed at the pulmonary valve.
- Coarctation of the Aorta: A narrowing of the major artery (the aorta) that carries blood to the body.
- Transposition of the Great Arteries: A condition where the two main arteries going out of the heart are switched in position.
Causes and Risk Factors
The exact cause of congenital heart defects is often unknown. However, several factors may increase the risk of a baby being born with a CHD, including:
- Genetic Factors: CHDs can run in families, suggesting a genetic component.
- Environmental Factors: Certain environmental factors, such as the mother’s use of certain medications, alcohol or drug abuse, or exposure to certain chemicals during pregnancy, can increase the risk.
- Maternal Health Conditions: Conditions such as diabetes or obesity in the mother can increase the risk of CHDs in the baby.
- Infections during Pregnancy: Certain infections during pregnancy can increase the risk of CHDs.
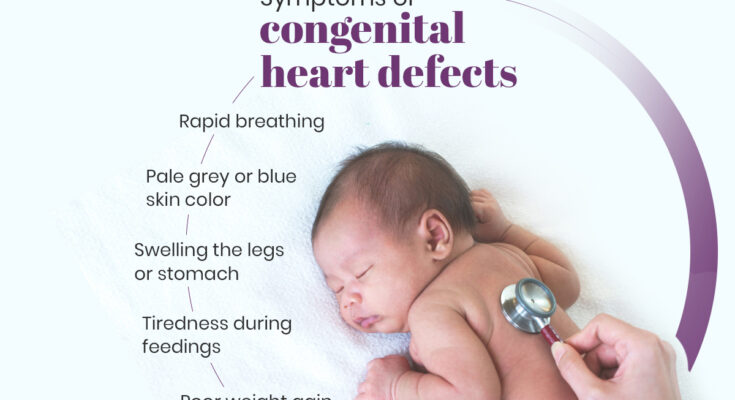
Symptoms and Signs to Watch For
Symptoms of congenital heart defects can vary widely depending on the type and severity of the defect. Some children with mild defects may have no symptoms, while those with more severe forms may exhibit signs early in life. Common symptoms and signs to watch for include:
- Rapid breathing or shortness of breath
- Fatigue and weakness, especially during physical activity
- A bluish tint to the skin, lips, and fingernails (cyanosis)
- Poor weight gain in infants
- Swelling in the legs, abdomen, or areas around the eyes
- Fainting, dizziness, or lightheadedness
- Heart murmurs or irregular heart rhythms
Early detection and treatment of congenital heart defects can significantly improve the outlook for children with these conditions. Advances in medical treatments and interventions have greatly improved the life expectancy and quality of life for many individuals with CHDs. If you suspect your child has a congenital heart defect, it is crucial to consult a healthcare provider for an accurate diagnosis and appropriate treatment.
Diagnosis of Congenital Heart Defects
The early diagnosis of congenital heart defects (CHDs) plays a pivotal role in managing and treating heart anomalies present from birth. Understanding the screening and diagnostic processes, the indispensable role of pediatric cardiologists, and the importance of early detection is essential for parents and caregivers. This guide provides an insightful overview of navigating through the complexities of CHDs, emphasizing the significance of specialized care and timely intervention.
Screening and Diagnostic Tests
The journey towards diagnosing congenital heart defects begins with comprehensive screening and diagnostic tests. These tests are designed to detect any abnormalities in the heart’s structure and function. The screening process often starts prenatally with fetal ultrasounds, which can reveal signs of heart defects before a child is born. After birth, newborns undergo a routine pulse oximetry screening, a non-invasive test that measures oxygen levels in the blood and can indicate potential heart problems.
For further examination, pediatric cardiologists may recommend advanced diagnostic tests such as echocardiograms, cardiac MRIs, or CT scans. An echocardiogram, often referred to as a cardiac echo, uses sound waves to create detailed images of the heart, allowing doctors to evaluate the heart’s structure and blood flow. Cardiac MRI and CT scans offer complementary detailed views, aiding in the comprehensive assessment of complex heart defects.
The Role of Pediatric Cardiologists in Diagnosis
Pediatric cardiologists are the cornerstone of diagnosing and managing congenital heart defects. These specialists possess the expertise to interpret screening results accurately and conduct further diagnostics to confirm the presence of CHDs. Their in-depth understanding of the unique needs of infants, children, and adolescents with heart conditions ensures that each patient receives a personalized care plan tailored to their specific heart defect.
Pediatric cardiologists also play a crucial role in guiding families through the diagnosis process, providing support, and outlining the most effective treatment options available. Their dedication to their young patients goes beyond medical treatment, encompassing emotional and psychological support to help families navigate the challenges of living with a congenital heart defect.
Importance of Early Detection
Early detection of congenital heart defects is paramount in mitigating potential complications and improving the quality of life for affected children. Identifying heart defects at the earliest possible stage allows for timely interventions, which can range from medication management to surgical procedures, depending on the severity of the condition. Early diagnosis also enables healthcare providers to monitor the child’s heart health closely, adapt treatments as they grow, and prevent serious complications.
Moreover, early detection and treatment planning contribute significantly to reducing the emotional and financial stress on families. It opens doors to specialized care and support services, offering hope and a pathway to a healthier future for children with congenital heart defects.
The diagnosis of congenital heart defects involves a collaborative approach centered around advanced screening techniques, the expertise of pediatric cardiologists, and the critical importance of early detection. Embracing this journey with knowledge and understanding equips parents and caregivers with the tools to seek the best possible care for their children, ensuring they lead fulfilling lives despite the challenges of CHDs. Early intervention and specialized care are the keys to unlocking a brighter, healthier future for children born with heart defects.
Treatment Options for Congenital Heart Defects in Children
Treatment options range from non-surgical interventions to cutting-edge surgical procedures, and ongoing research continues to unveil new methods and technologies. Here’s an overview of the treatment landscape for congenital heart defects in children.
Non-Surgical Treatments
Non-surgical treatments are often the first line of management for mild congenital heart defects and can include:
- Medications: Drugs can help manage symptoms and improve heart function. Common medications include diuretics to reduce fluid accumulation, ACE inhibitors to lower blood pressure, and beta-blockers to regulate heart rhythms.
- Oxygen Therapy: For children with CHDs that affect oxygen levels in the blood, supplemental oxygen can help ensure that their bodies receive enough oxygen.
- Cardiac Catheterization: This minimally invasive procedure involves inserting a thin tube into a vein or artery and guiding it to the heart to correct certain defects without open-heart surgery.
Surgical Treatments
For more severe congenital heart defects, surgical intervention may be necessary:
- Open-Heart Surgery: Used to repair structural heart defects, such as holes in the heart, valve problems, or abnormal blood vessels.
- Heart Transplant: In rare cases where a heart defect cannot be repaired, a heart transplant may be the only option.
Emerging Treatment Options and Technological Advancements
The field of pediatric cardiology is rapidly evolving, with new treatments and technologies on the horizon:
- Stem Cell Therapy: Research is ongoing into how stem cells can be used to regenerate damaged heart tissue.
- 3D Printing: Customized 3D-printed heart models are being used for surgical planning and to create implants tailored to the unique anatomy of each child’s heart.
- Robot-Assisted Surgery: Offers the potential for more precise and less invasive procedures, reducing recovery times and improving outcomes.
The Multidisciplinary Approach to Treatment
A holistic and multidisciplinary approach is crucial for managing congenital heart defects. This involves a team of specialists, including:
- Pediatric Cardiologists: Doctors who specialize in diagnosing and treating heart problems in children.
- Cardiothoracic Surgeons: Surgeons who perform heart surgery.
- Nurses and Nurse Practitioners: Provide care and support throughout the treatment process.
- Social Workers and Psychologists: Help families cope with the emotional and psychological aspects of a CHD diagnosis and treatment.
This comprehensive team works together to create a tailored treatment plan that addresses the medical, psychological, and social needs of the child and their family.
However, the treatment of congenital heart defects in children has made significant strides, and ongoing research continues to push the boundaries of what is possible. With a combination of non-surgical treatments, surgical interventions, and the promise of new technologies, the future for children with CHDs is brighter than ever.
Advancements in the Treatment of Congenital Heart Defects
The treatment of congenital heart defects (CHDs) has witnessed significant advancements over the past few decades. These improvements span across surgical techniques, genetic therapy, stem cell research, and postoperative care, offering hope and improved outcomes for patients. This article delves into the innovations in surgical procedures, explores the promising future of gene therapy and stem cell research, and highlights the enhancements in postoperative care and monitoring.
Innovations in Surgical Techniques
The evolution of surgical techniques has been a cornerstone in treating congenital heart defects. Minimally invasive surgery, for instance, has become more prevalent, reducing recovery times and improving the precision of complex procedures. Techniques such as the use of real-time 3D imaging and robotic-assisted surgery offer surgeons unprecedented views and control, leading to higher success rates and lower risks of complications. These technological advancements have not only made surgeries safer but also accessible to a broader range of patients, including newborns and infants with complex heart defects.
The Future of Gene Therapy and Stem Cell Research
Gene therapy and stem cell research represent the frontier of congenital heart defect treatments. These approaches target the underlying causes of heart defects, offering the potential for not just treatment but cure. Gene therapy aims to correct or replace faulty genes responsible for heart defects, a strategy that could prevent the development of CHDs before birth. Meanwhile, stem cell research focuses on regenerating damaged heart tissue, offering the promise of repairing heart defects after they have occurred. While still in the experimental stages, early successes in these areas provide a glimpse into a future where congenital heart defects may be corrected at the genetic or cellular level, reducing the need for invasive surgeries.
Improvements in Postoperative Care and Monitoring
Postoperative care and monitoring have also seen remarkable improvements, significantly impacting patient outcomes. Enhanced monitoring technologies and practices now allow for real-time tracking of a patient’s recovery, enabling immediate response to any signs of distress or complication. Innovations in pain management and physical therapy have improved patient comfort and recovery speed. Moreover, the integration of telehealth services has revolutionized follow-up care, making it easier for patients to stay connected with their healthcare providers, ensuring continued care and monitoring without the frequent need for in-person visits.
Living with Congenital Heart Defects
Living with Congenital Heart Defects (CHDs) presents unique challenges and requires ongoing attention to ensure the well-being of the affected child and their family. Understanding the journey of living with CHDs, from long-term care and monitoring to the impact on daily life, and the support systems available, can empower families to navigate these challenges more effectively.
Long-Term Care and Monitoring
Children with Congenital Heart Defects require continuous medical oversight throughout their lives. This long-term care often involves regular check-ups with pediatric cardiologists, medication management, and possibly additional surgeries or interventions as the child grows. Advances in medical technology and treatment strategies have significantly improved the outcomes for children with CHDs, making it possible for many to lead full, active lives. However, the necessity for ongoing monitoring underscores the importance of establishing a strong relationship with healthcare providers who specialize in congenital heart conditions.
Impact on the Child’s Life and Family
The impact of CHDs extends beyond the physical challenges faced by the child. It can affect every aspect of family life, including emotional well-being, financial stability, and social interactions. Families often navigate feelings of anxiety and uncertainty, especially around the time of diagnosis and surgical interventions. The child’s condition may also impose limitations on physical activities, affecting their ability to participate in certain sports or play with peers, which can influence their social development and self-esteem.
Support Systems and Resources for Families
Fortunately, there are numerous support systems and resources designed to assist families dealing with CHDs. These include:
- Support Groups: Connecting with other families who are going through similar experiences can provide emotional support, practical advice, and a sense of community. Many hospitals and organizations offer support groups for parents and siblings of children with CHDs.
- Financial Assistance Programs: The cost of ongoing medical care for CHDs can be substantial. Various organizations and charities offer financial assistance programs to help families cover medical expenses and travel costs related to treatment.
- Educational Resources: Understanding CHDs is crucial for families. Hospitals, clinics, and heart health organizations provide educational materials that explain different types of heart defects, treatment options, and how to care for a child with a heart condition.
- Advocacy and Awareness Organizations: Groups such as the American Heart Association and The Children’s Heart Foundation work to raise awareness about CHDs and advocate for research and policies that benefit children with heart conditions and their families.
It’s essential for families to seek out and utilize the support systems available to them, fostering a community of care that surrounds the child with love, understanding, and the best possible opportunities for health and happiness.
FAQs on Congenital Heart Defects in Children Treatment
What are congenital heart defects in children?
Congenital heart defects (CHDs) refer to problems with the heart’s structure that are present from birth. These defects can affect the walls of the heart, the valves of the heart, and the arteries and veins near the heart. They can disrupt the normal flow of blood through the heart, which can affect breathing, circulation, and overall health.
How are congenital heart defects diagnosed?
CHDs are often detected during pregnancy through routine ultrasounds or soon after birth if symptoms are evident. Diagnostic tests may include echocardiograms, electrocardiograms (EKG), chest X-rays, pulse oximetry, and cardiac MRI. These tests help doctors understand the nature of the defect and plan appropriate treatment.
What treatment options are available for children with congenital heart defects?
Treatment options vary depending on the type and severity of the heart defect. They can range from medications that help manage symptoms to more invasive procedures like catheter-based interventions and heart surgery. In some cases, a combination of treatments may be necessary to address the defect effectively.
Is surgery always required for treating congenital heart defects?
Not all congenital heart defects require surgery. Some mild defects may only need monitoring and medications to manage symptoms. However, moderate to severe defects often require surgical intervention to repair the heart and improve its function. The necessity of surgery is determined based on the specific defect and the child’s overall health.
How can I prepare my child for heart surgery?
Preparing your child for heart surgery involves both emotional and physical preparation. Discuss the procedure in a way that is appropriate for your child’s age and understanding. Ensure they know what to expect before, during, and after surgery. Physically, follow the medical team’s instructions regarding eating, drinking, and medication adjustments. Support from family, friends, and possibly a child psychologist can also be beneficial.
What is the recovery process like after surgery for congenital heart defects?
Recovery varies by individual and the complexity of the surgery. Initially, children will spend time in the intensive care unit (ICU) for close monitoring. The total hospital stay can range from a few days to a few weeks. Once home, recovery includes rest, gradual increase in activities, and follow-up appointments. Parents and caregivers play a crucial role in monitoring the child’s health and ensuring compliance with post-operative care instructions.
Can children with treated congenital heart defects lead normal lives?
Many children with treated congenital heart defects can lead active, healthy lives. Advances in medical and surgical treatments have significantly improved outcomes. However, ongoing medical care and monitoring are important to manage any long-term effects and ensure the best quality of life.
Where can I find support and resources for managing my child’s congenital heart defect?
Support and resources are available through hospitals, heart health organizations, and online communities. These can provide valuable information, emotional support, and connections to other families navigating similar experiences. Your healthcare provider can also recommend resources tailored to your child’s needs.
Conclusion
For parents and guardians navigating the complexities of CHDs with their children, your role is incredibly significant. Your dedication, love, and support provide the essential foundation for your child’s resilience and well-being. It’s important to stay informed, advocate for your child’s health needs, and connect with supportive communities that understand your journey. Remember, your strength and advocacy are powerful forces that can drive positive changes in both your child’s life and the broader landscape of congenital heart defect care.
Looking towards the future, the outlook for children with CHDs is more hopeful than ever. With ongoing research, enhanced funding, and the collective efforts of healthcare providers, families, and policymakers, we are moving closer to a world where every child with a CHD can lead a fuller, healthier life. The challenges are significant, but so are the opportunities for breakthroughs and progress. By working together, we can continue to improve the lives of children with CHDs, offering them the bright and promising future they deserve.
In summary, the journey with congenital heart defects is a testament to the power of resilience, the importance of continuous advancement, and the impact of community support. As we look forward, let’s carry with us the hope that research, funding, and shared efforts will lead to even greater outcomes for children affected by CHDs. Together, we can make a difference in the lives of these brave young hearts.