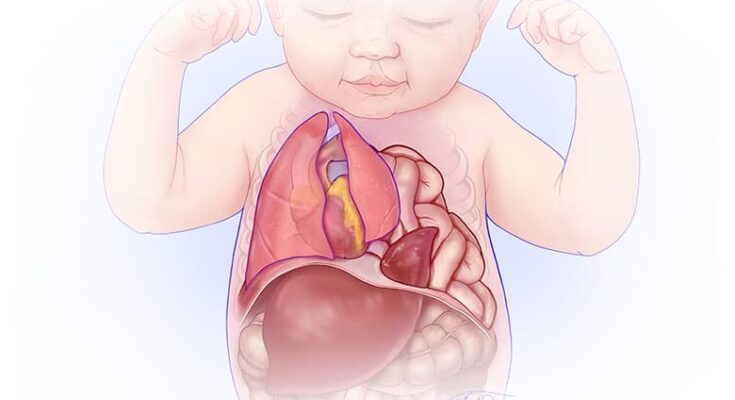
Congenital Diaphragmatic Hernia Treatment: Congenital Diaphragmatic Hernia (CDH) is a significant medical condition that affects infants, characterized by an abnormal development of the diaphragm, the muscle that separates the chest cavity from the abdominal cavity.
This condition allows the abdominal organs to move into the chest, which can cause severe complications in breathing and overall health.
Understanding the diagnosis and treatment options for CDH is crucial for parents, caregivers, and medical professionals to manage this condition effectively.
What is Congenital Diaphragmatic Hernia (CDH)
Congenital Diaphragmatic Hernia (CDH) is a serious condition present at birth that affects the diaphragm, the muscle that helps in breathing by moving up and down. This condition allows abdominal organs to move into the chest, which can lead to severe breathing difficulties and other complications. Understanding CDH, its prevalence, impact, causes, risk factors, and types is essential for early diagnosis and treatment.
Statistics on Prevalence and Impact
CDH affects approximately 1 in every 2,500 to 3,000 live births. The impact of CDH can vary significantly, ranging from mild to life-threatening conditions. The survival rate for babies born with CDH has improved over the years, thanks to advancements in medical technology and treatment methods. However, it still poses significant challenges, with survival rates hovering around 70% to 80% in developed countries. The condition not only affects the physical health of the newborn but also has a profound emotional and financial impact on the families involved.
Causes and Risk Factors
The exact cause of CDH is not known, but it is believed to result from a combination of genetic and environmental factors. Some of the risk factors associated with CDH include a family history of the condition, maternal smoking during pregnancy, and certain genetic conditions. Researchers are continuously studying the role of genes and the environment to better understand the causes of CDH and identify potential preventive measures.
Types of CDH
CDH can be categorized into two main types based on the location of the hernia:
- Bochdalek Hernia: This is the most common type of CDH, occurring in approximately 85% to 90% of cases. It typically appears on the left side of the diaphragm, allowing abdominal organs like the stomach, intestines, and sometimes the liver, to move into the chest cavity.
- Morgagni Hernia: Less common than the Bochdalek hernia, Morgagni hernias occur near the center of the diaphragm, closer to the front of the body. These hernias are generally smaller and may present fewer symptoms but can still significantly impact the affected infant’s health.
However, Congenital Diaphragmatic Hernia is a complex condition that requires prompt and effective medical intervention. Understanding the prevalence, impact, causes, risk factors, and types of CDH is crucial for early diagnosis, treatment planning, and improving the overall outcomes for affected infants. With ongoing research and advancements in medical care, there is hope for better management and survival rates for babies born with CDH.
Symptoms and Early Signs of Congenital Diaphragmatic Hernia (CDH)
Recognizing the symptoms and early signs of CDH is crucial for prompt treatment, which can significantly improve outcomes for affected infants. This guide will outline common symptoms in newborns, how to recognize warning signs, and the importance of early detection.
Common Symptoms in Newborns
CDH can present a range of symptoms in newborns, which may vary in severity depending on the size of the hernia and the organs involved. Common symptoms include:
- Difficulty Breathing: Newborns with CDH may experience rapid, labored, or shallow breathing due to the displacement of the lungs by abdominal organs.
- Blue Skin Coloration (Cyanosis): Insufficient oxygenation can cause a bluish tint to the skin, lips, and fingernails.
- Abnormal Chest Shape: The chest may appear concave or asymmetrical due to the position of the displaced organs.
- Diminished Breath Sounds: A stethoscope may reveal reduced or absent breath sounds on the affected side of the chest.
- A Soft Belly: The abdomen may feel less full or softer than normal because the organs are in the chest cavity, not the abdominal cavity.
How to Recognize Warning Signs
Early detection of CDH is critical. Parents, caregivers, and healthcare providers should be vigilant for the above symptoms, especially if they present shortly after birth. Any signs of distress, difficulty breathing, or unusual chest or abdominal appearances should prompt immediate medical evaluation. Advances in prenatal imaging now often allow for the diagnosis of CDH before birth, giving families and medical teams time to plan for specialized care the newborn may require.
The Importance of Paying Attention to Early Symptoms for Prompt Treatment
Prompt recognition and treatment of CDH are vital. Early intervention can help manage respiratory distress and prepare for surgical repair of the diaphragm. The prognosis for infants with CDH significantly improves with immediate and appropriate medical attention. Treatment typically involves stabilizing the infant, followed by surgery to reposition any displaced organs and repair the diaphragm.
Surgery alone, however, is not the sole aspect of treatment; comprehensive care including respiratory support, nutritional support, and sometimes long-term follow-up for associated conditions is essential for the best outcomes. Early diagnosis, either prenatally or immediately after birth, followed by prompt treatment, can greatly enhance the quality of life for infants with CDH and reduce the risk of complications.
However, understanding and recognizing the symptoms and early signs of Congenital Diaphragmatic Hernia in newborns is crucial. Early detection and treatment pave the way for improved survival rates and health outcomes, highlighting the importance of vigilant observation and prompt medical intervention for newborns showing any signs of CDH.
Diagnosis of Congenital Diaphragmatic Hernia
Early and accurate diagnosis is crucial for managing CDH effectively. This article outlines the diagnostic procedures for CDH, explores the role of genetic testing, and discusses how diagnoses influence treatment plans.
List of Diagnostic Procedures
The diagnosis of Congenital Diaphragmatic Hernia typically involves several procedures aimed at assessing the condition’s severity and planning appropriate treatment strategies. These procedures include:
- Prenatal Ultrasound: This is the most common method for diagnosing CDH before birth. It helps in identifying the herniation of abdominal organs into the chest cavity.
- Fetal MRI: Magnetic Resonance Imaging (MRI) provides detailed images of the fetus and can be used to assess the severity of the hernia and its impact on lung development.
- Echocardiogram: This test assesses the heart’s function and structure, which can be affected by the shifted organs in cases of CDH.
- Chest X-ray: After birth, a chest X-ray can confirm the diagnosis by showing the position of abdominal organs within the chest cavity.
- Blood Tests: These can be conducted to check for other conditions that might be associated with CDH or to assess the baby’s overall health.
The Role of Genetic Testing
While the exact cause of CDH is not always clear, genetic factors can play a significant role. Genetic testing has emerged as a pivotal tool in the diagnostic process, offering insights into potential genetic abnormalities associated with CDH. It can help in identifying underlying genetic conditions, guiding treatment decisions, and providing information for genetic counseling. Genetic testing might involve examining the baby’s DNA, usually through a blood sample, to look for chromosomal abnormalities that could be linked to CDH.
How Diagnoses Influence Treatment Plans
The diagnosis of CDH, particularly the details uncovered through the diagnostic procedures and genetic testing, significantly influences the treatment plan. The severity of the hernia, the presence of other congenital abnormalities, and the baby’s overall health condition play critical roles in determining the course of treatment. Typically, treatment plans may include:
- Surgical Repair: The primary treatment for CDH is surgery to reposition the herniated organs into the abdomen and repair the diaphragm. The timing and approach to surgery depend on the baby’s health and lung development.
- Supportive Care: This includes measures to support breathing, such as mechanical ventilation, and nutrition until surgery is feasible.
- Long-term Management: Depending on the presence of other conditions or complications, long-term care may involve additional surgeries, respiratory support, and regular monitoring.
As research continues to evolve, the integration of advanced diagnostic methods is likely to further improve the management strategies for CDH, enhancing the quality of life for affected individuals.
Treatment Options for Congenital Diaphragmatic Hernia (CDH)
The successful management of CDH involves immediate care and stabilization of the newborn, surgical interventions, and supportive non-surgical treatments. The choice of treatment is highly personalized, depending on the severity of the hernia and the overall health of the infant.
Immediate Care and Stabilization of the Newborn
The initial step in treating CDH involves the stabilization of the newborn to ensure they are breathing properly and their vital signs are stable. This may include providing oxygen, using a ventilator if necessary, and ensuring that the baby is warm and stable. This critical phase allows healthcare providers to assess the baby’s condition thoroughly and plan the next steps of treatment.
Surgical Treatments: Overview and Types
Surgical repair is often essential in treating CDH. The timing of surgery depends on the newborn’s stability and overall health. There are several surgical approaches:
- Repair of the Diaphragm: The most common surgical treatment involves repairing the diaphragm’s hole. The surgeon stitches the muscle back together. If the hole is large or the diaphragm muscle is underdeveloped, additional measures may be required.
- Use of a Patch: In cases where the diaphragm cannot be stitched together due to the size of the hernia, a surgical patch may be used to cover the opening. This patch acts as part of the diaphragm, allowing the lungs to expand and function more normally.
- Minimally Invasive Techniques: For some infants, minimally invasive surgery (such as laparoscopy or thoracoscopy) may be an option. These techniques involve smaller incisions, which can lead to quicker recovery times and less post-operative pain.
Non-surgical Treatments
In addition to surgical options, non-surgical treatments play a crucial role in the care of infants with CDH:
- Respiratory Support: Many babies with CDH require assistance with breathing. This can range from supplemental oxygen to more advanced support like mechanical ventilation or extracorporeal membrane oxygenation (ECMO) if the baby has severe pulmonary hypertension.
- Nutritional Support: Ensuring the baby receives adequate nutrition is vital for recovery and growth. This may involve feeding through a tube initially, especially if the baby has difficulty sucking or swallowing.
Importance of Personalized Treatment Plans
Each case of CDH is unique, and treatment plans must be tailored to the individual needs of the newborn. A multidisciplinary team of specialists, including neonatologists, pediatric surgeons, respiratory therapists, and nutritionists, work together to create a comprehensive care plan. This personalized approach ensures that each aspect of the baby’s health is addressed, optimizing the chances for a successful recovery.
However, the treatment of Congenital Diaphragmatic Hernia requires a coordinated, multidisciplinary approach, prioritizing immediate stabilization, appropriate surgical intervention, and supportive care. Personalized treatment plans are essential for addressing the unique challenges of each case, aiming for the best possible outcomes for these vulnerable patients.
Innovations in Congenital Diaphragmatic Hernia Treatment
Recent advancements in the field have paved the way for innovative approaches, enhancing the survival rates and outcomes for affected newborns. This section delves into the latest research and developments, highlights advances in surgical techniques, and explores emerging therapies, shedding light on their potential to revolutionize CDH treatment.
Latest Research and Developments
The landscape of CDH treatment is continually evolving, thanks to ongoing research efforts. Recent studies focus on understanding the genetic and molecular underpinnings of CDH, aiming to identify predictive markers for disease severity and potential therapeutic targets. This research is crucial for developing personalized treatment plans and improving prognostic models. Additionally, advancements in prenatal imaging techniques have significantly improved the early detection of CDH, allowing for better preparation and timely interventions.
Advances in Surgical Techniques
Surgical intervention remains a cornerstone in the management of CDH. Over the years, there have been significant improvements in surgical techniques, enhancing the safety and efficacy of the procedures. Minimally invasive techniques, such as thoracoscopic and laparoscopic repairs, have become more prevalent, offering the benefits of smaller incisions, reduced pain, and quicker recovery times. Furthermore, the introduction of fetoscopic endoluminal tracheal occlusion (FETO) represents a promising prenatal surgical approach. FETO involves the temporary blockage of the fetal trachea, promoting lung growth in utero and improving postnatal outcomes.
Emerging Therapies and Their Potential
Beyond surgical innovations, emerging therapies offer new hope for CDH treatment. One such area of exploration is the use of stem cell therapy and tissue engineering to repair or regenerate the diaphragm and affected lung tissue. Early-stage research suggests that these approaches could potentially reduce the need for invasive surgeries and improve long-term lung function. Additionally, pharmacological interventions aimed at enhancing pulmonary development and reducing pulmonary hypertension—a common complication of CDH—are under investigation. These emerging therapies, while still in the experimental phase, hold the promise of transforming the treatment landscape for CDH, potentially improving survival rates and quality of life for affected individuals.
However, the field of congenital diaphragmatic hernia treatment is witnessing remarkable innovations, from advanced surgical techniques to cutting-edge research into genetic therapies and stem cell treatments. These developments not only aim to improve immediate outcomes but also seek to enhance the long-term health and well-being of those affected by CDH. As research continues to advance, there is renewed hope for more effective and less invasive treatment options, signaling a brighter future for patients and their families.
The Role of Multidisciplinary Care in Congenital Diaphragmatic Hernia (CDH) Treatment
This condition can lead to significant respiratory distress and other complications shortly after birth. Given the complexity of CDH, a multidisciplinary approach to treatment is not just beneficial; it’s essential. This article delves into the importance of a team approach, the specialists involved in care, and the coordination of care for the best outcomes in CDH treatment.
Importance of a Team Approach
A team approach is crucial in the treatment of CDH due to the condition’s multifaceted nature. Babies with CDH often require immediate and highly specialized care to manage not just the diaphragmatic hernia but also associated complications such as pulmonary hypoplasia (underdeveloped lungs) and pulmonary hypertension (high blood pressure in the lungs’ arteries). A multidisciplinary team brings together healthcare professionals from various specialties to address the wide range of needs these patients have, ensuring a comprehensive and cohesive treatment plan.
Specialists Involved in Care
The multidisciplinary care team for CDH typically includes:
- Neonatologists: Doctors specializing in the care of newborns who lead the treatment plan and coordinate care among different specialists.
- Pediatric Surgeons: Surgeons with expertise in treating conditions in infants, including performing the surgery to repair the diaphragmatic hernia.
- Respiratory Therapists: Professionals who assist with the management of the baby’s breathing challenges.
- Nutritionists: Experts who ensure the baby receives the right nutrients to grow and recover.
- Physical Therapists: Specialists who help in the development of motor skills and address any musculoskeletal issues.
- Pediatric Cardiologists: Doctors who monitor and manage heart-related issues, such as pulmonary hypertension, that can accompany CDH.
- Social Workers and Support Staff: Professionals who provide emotional support and practical assistance to the families, helping them navigate the complexities of care.
Coordinating Care for the Best Outcomes
Coordinating care among the various specialists involved is key to achieving the best outcomes for babies with CDH. This coordination ensures that all aspects of the child’s health are addressed in a synchronized manner, from surgical repair of the hernia and management of respiratory function to nutritional support and physical development. Regular team meetings and communication between specialists are vital components of this process, allowing for the continuous evaluation of the patient’s progress and the adjustment of treatment plans as needed.
By adopting a multidisciplinary approach to CDH treatment, healthcare providers can offer personalized, high-quality care that addresses the full spectrum of needs for these vulnerable patients. This comprehensive strategy not only improves survival rates but also enhances the quality of life for children with CDH and their families, underscoring the vital role of teamwork in managing complex health challenges.
However, the multidisciplinary care model in the treatment of Congenital Diaphragmatic Hernia represents best practice in pediatric healthcare. It emphasizes the importance of specialized, coordinated care and the positive impact it has on patient outcomes, showcasing how collaboration among healthcare professionals can lead to the successful management of even the most challenging conditions.
Recovery and Long-term Care of Congenital Diaphragmatic Hernia (CDH)
Recovering from Congenital Diaphragmatic Hernia (CDH) is a gradual process that extends beyond the initial treatment phase, necessitating ongoing care and monitoring to ensure the best possible outcomes for the child. This comprehensive guide outlines what families and caregivers can expect during the recovery phase, how to monitor for potential complications, the long-term outlook for children with CDH, and the support available for families and caregivers.
What to Expect After Treatment
Following the surgical repair of a CDH, babies often remain in the hospital’s neonatal intensive care unit (NICU) for several weeks. The length of stay can vary depending on the severity of the hernia, the presence of other health conditions, and how well the baby responds to treatment. During this time, babies receive support to breathe, feed, and grow. Parents and caregivers are encouraged to be involved in their baby’s care as much as possible, learning from the healthcare team how to care for their child’s unique needs once home.
Monitoring for Complications
After discharge, regular follow-ups with pediatric specialists are essential to monitor the child’s development, lung function, and to address any complications that may arise. Complications can include respiratory problems, growth and feeding issues, and gastroesophageal reflux disease (GERD). Early identification and management of these complications can prevent more serious problems and improve the child’s quality of life.
Long-term Outlook and Quality of Life
The long-term outlook for children with CDH has improved significantly with advances in medical care. Many children go on to lead healthy, active lives. However, some may experience ongoing health issues related to their condition, such as chronic lung disease or developmental delays. Regular check-ups with healthcare providers can help manage these issues effectively. Participation in therapies, such as respiratory therapy or physical therapy, can also be beneficial.
Support for Families and Caregivers
Caring for a child with CDH can be challenging, but support is available. Hospitals and healthcare teams can provide resources and referrals to support groups, counseling, and other services to help families navigate the complexities of CDH care. Connecting with other families who have gone through similar experiences can be incredibly supportive. Online forums and local support groups offer spaces to share experiences, advice, and encouragement.
However, the recovery and long-term care of children with Congenital Diaphragmatic Hernia require a multidisciplinary approach that includes medical treatment, regular monitoring, and support for both the child and their family. With the right care and support, children with CDH can achieve a good quality of life, overcoming the challenges posed by their condition. Families and caregivers play a crucial role in their care and have access to various resources to aid them on this journey.
FAQs (Frequently Asked Questions) about Congenital Diaphragmatic Hernia (CDH)
What is Congenital Diaphragmatic Hernia (CDH)?
Congenital Diaphragmatic Hernia (CDH) is a birth defect that occurs when the diaphragm, the muscle that separates the chest from the abdomen, fails to develop properly. This allows abdominal organs, such as the stomach, intestines, and liver, to move into the chest, which can impair lung development and function.
How common is CDH?
CDH affects approximately 1 in every 2,500 to 5,000 live births. It can occur in any pregnancy and is seen equally in males and females.
What causes CDH?
The exact cause of CDH is not known. It is believed to result from a combination of genetic and environmental factors. In some cases, CDH is associated with other genetic conditions or syndromes.
What are the symptoms of CDH?
Symptoms of CDH may vary depending on the severity of the condition. Common symptoms include difficulty breathing, a rapid heartbeat, a bluish color to the skin due to lack of oxygen (cyanosis), and a concave abdomen due to the displacement of abdominal organs.
How is CDH diagnosed?
CDH is often diagnosed before birth through prenatal ultrasound. This imaging test can reveal the herniation of abdominal organs into the chest. After birth, diagnosis may be confirmed through physical examination, chest X-rays, and other imaging studies.
What treatment options are available for CDH?
The primary treatment for CDH is surgery to repair the diaphragm and return the abdominal organs to their proper place. This surgery is typically performed after the baby is stabilized, often within the first few days to weeks of life. In severe cases, additional treatments, such as ECMO (Extracorporeal Membrane Oxygenation), may be necessary to support the baby’s breathing.
What is the prognosis for babies with CDH?
The prognosis for babies with CDH varies depending on the severity of the condition, the presence of other anomalies, and the timing of the diagnosis and treatment. Advances in medical care have significantly improved the survival rate, which is now over 70% in many specialized centers.
Can CDH be prevented?
Since the exact cause of CDH is not fully understood, there are no specific measures to prevent it. However, maintaining a healthy pregnancy through proper nutrition, avoiding harmful substances, and regular prenatal care can help reduce the risk of birth defects.
Is there any research being done on CDH?
Yes, ongoing research is focused on understanding the causes of CDH, improving diagnostic methods, and developing advanced treatments to enhance outcomes for affected infants. Researchers are also exploring genetic factors that may contribute to the condition.
Conclusion:
For parents and caregivers, the journey with CDH can be daunting. However, it’s essential to remember that you’re not alone. There are specialized care centers with teams of experts dedicated to the treatment of CDH. These professionals are equipped with the knowledge, skills, and resources to provide the best possible care for your child. Seeking out these specialized services can make a significant difference in the management of the condition and the overall wellbeing of your child and family.
Encouragement for those navigating this challenging path is crucial. While the road may seem long and filled with uncertainty, there is hope. With early diagnosis, advanced treatment options, and the support of specialized care teams, many children with CDH go on to lead healthy, fulfilling lives. It’s important for parents and caregivers to reach out for support, stay informed about the latest in CDH care, and advocate for the best possible outcomes for their child.
In closing, Congenital Diaphragmatic Hernia presents significant challenges, but with the right approach, these can be navigated successfully. Early diagnosis, cutting-edge treatment, and specialized care are the cornerstones of managing CDH, offering hope and a brighter future for affected children and their families.