Congenital Diaphragmatic Hernia Symptoms: Congenital Diaphragmatic Hernia (CDH) represents a critical condition that emerges before birth, involving an abnormal development of the diaphragm, the muscle that separates the chest cavity from the abdominal cavity.
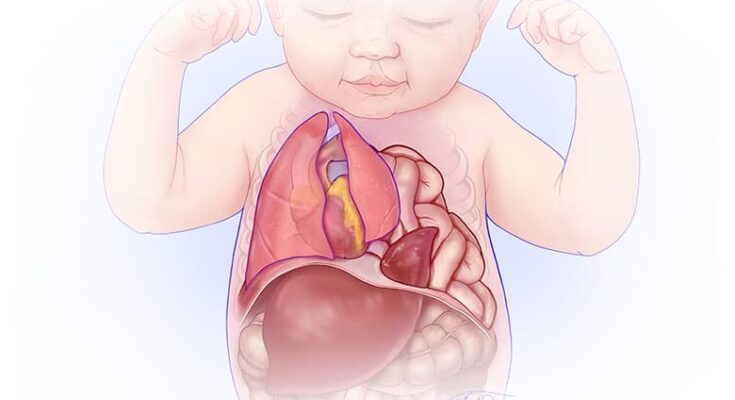
This anomaly allows abdominal organs to move into the chest, which can severely affect lung development and function.
Our in-depth exploration aims to furnish readers with comprehensive insights into the symptoms and causes of CDH, underpinned by the latest research and expert analyses.
What is Congenital Diaphragmatic Hernia (CDH)?
Congenital Diaphragmatic Hernia (CDH) is a serious condition that occurs in newborns, characterized by an abnormal development of the diaphragm, the muscle that separates the chest cavity from the abdominal cavity. This developmental anomaly results in an opening in the diaphragm, allowing abdominal organs such as the stomach, intestines, and sometimes the liver, to move into the chest cavity. This migration of organs into the chest can severely impact the development of the lungs, leading to respiratory distress and other complications after birth.
The cause of CDH is not fully understood, but it is believed to involve a combination of genetic and environmental factors. The condition is diagnosed either prenatally, through ultrasound imaging, or after birth, based on clinical signs and imaging tests. Treatment for CDH typically involves surgical repair of the diaphragmatic opening, but the timing and approach to surgery may vary based on the severity of the condition and the health of the newborn. Despite advances in medical care, CDH remains a challenging condition with significant morbidity and mortality rates.
Statistics on Prevalence and Demographics Affected
Congenital Diaphragmatic Hernia is relatively rare, affecting approximately 1 in every 2,500 to 3,000 live births worldwide. There is no clear preference for any specific demographic group based on race or ethnicity, indicating that CDH can occur across all populations. However, there is a slight male predominance, with boys being affected slightly more often than girls.
The survival rates for infants with CDH have improved significantly over the years, thanks to advancements in prenatal diagnosis, neonatal care, and surgical techniques. Currently, the overall survival rate for babies born with CDH is about 70%, but this figure can vary widely depending on several factors. These include the severity of the hernia, the presence and severity of other congenital anomalies, and the timing and effectiveness of medical and surgical interventions.
Despite the challenges posed by CDH, early and aggressive management of the condition can lead to positive outcomes for many affected infants. Continuous research and improvements in prenatal care and neonatal intensive care practices are crucial in further increasing the survival rates and improving the quality of life for children born with this condition.
Symptoms of Congenital Diaphragmatic Hernia
Recognizing the symptoms of CDH is crucial for early diagnosis and treatment. Here, we outline the key symptoms associated with CDH, how these symptoms present in newborns, and the signs that may indicate a severe case of CDH.
Key Symptoms Associated with CDH
The symptoms of Congenital Diaphragmatic Hernia can vary widely depending on the size of the hernia and the organs involved. However, some key symptoms commonly observed include:
- Difficulty Breathing: Newborns may exhibit rapid, labored, or gasping breaths.
- Blue Skin Coloration (Cyanosis): Insufficient oxygen levels can cause the skin, lips, and nail beds to have a bluish tint.
- Abnormal Chest Shape: The chest may appear concave or “sunken in” due to the displacement of abdominal organs.
- Diminished Breath Sounds: When listening with a stethoscope, there may be reduced or absent breath sounds on one side of the chest.
- A Soft Bulge in the Abdomen: The abdomen may feel soft or less full due to the displacement of organs into the chest cavity.
How Symptoms Present in Newborns
In newborns, symptoms of CDH typically become evident soon after birth and can range from mild to life-threatening. The most immediate and noticeable symptom is difficulty breathing, which is often accompanied by cyanosis, indicating a lack of oxygen. The abnormal positioning of organs may also lead to a noticeable deformity in the shape of the chest or abdomen. These symptoms are a direct result of the underdeveloped lung(s) and the pressure placed on them by the misplaced abdominal organs.
Signs That May Indicate a Severe Case of CDH
Certain signs can indicate a more severe case of Congenital Diaphragmatic Hernia, necessitating immediate medical attention:
- Persistent Cyanosis: Despite receiving oxygen therapy, the infant’s skin remains bluish, indicating severe oxygen deprivation.
- Severe Respiratory Distress: Marked by very rapid, labored breathing and the use of accessory muscles around the ribs and neck to breathe.
- Lack of Response to Initial Treatment: If symptoms do not improve with initial emergency treatment, this may indicate a more complex or severe case of CDH.
- Poor Blood Circulation: Indicated by weak pulse, cold extremities, and lethargy, suggesting compromised heart function or shock.
Early recognition of these symptoms and signs is critical for the effective management and treatment of Congenital Diaphragmatic Hernia. If CDH is suspected, prompt medical evaluation, including imaging and specialized care, is essential to address the respiratory, nutritional, and developmental needs of the affected newborn.
Causes and Risk Factors of Congenital Diaphragmatic Hernia (CDH)
The Developmental Cause of CDH During Pregnancy
Congenital Diaphragmatic Hernia (CDH) is a condition that arises during fetal development, typically characterized by an abnormal opening in the diaphragm. This opening allows organs normally situated in the abdomen, such as the stomach, intestines, and liver, to move into the chest cavity, thereby hampering proper lung formation. The exact developmental cause of CDH remains somewhat elusive, but it is understood to occur very early in pregnancy, often before many women realize they are pregnant. The diaphragm’s failure to form completely or properly is central to the development of CDH, affecting one in every 2,500 to 5,000 live births.
Genetic and Environmental Risk Factors
Research has indicated that both genetic and environmental factors play roles in the occurrence of CDH, though the specific causes can vary widely from one case to another.
Genetic Factors: There is evidence suggesting a genetic component to CDH, including associations with chromosomal abnormalities and genetic syndromes. For instance, conditions such as trisomy 18 and Fryns syndrome have been linked to a higher incidence of CDH. Families with a history of CDH may also have a slightly increased risk, though most cases appear to be sporadic, happening without a clear familial pattern.
Environmental Factors: Various environmental exposures during pregnancy have been explored as potential risk factors for CDH. These include maternal smoking, alcohol use, and certain medications or nutritional deficiencies. However, no single environmental factor has been conclusively linked to CDH, suggesting that its development is likely due to a complex interplay of multiple factors rather than a single cause.
Discussion on Research Findings Related to CDH Causes
Continuing research into CDH aims to unravel the complex interplay of factors that contribute to its development. Recent studies have focused on understanding the genetic pathways and environmental interactions that might predispose an individual to CDH. For example, advances in genetic sequencing technologies have enabled researchers to identify specific genes that may be involved in diaphragm development, offering potential insights into the biological mechanisms underlying CDH.
Moreover, research into the role of environmental factors, including exposure to certain chemicals or deficiencies in specific nutrients during pregnancy, continues to be an important area of study. Understanding these factors could lead to recommendations for preventive measures in at-risk populations.
However, while significant progress has been made in understanding the causes and risk factors of Congenital Diaphragmatic Hernia, much remains to be discovered. The condition’s multifactorial nature requires a multidisciplinary approach to research, combining genetics, environmental science, and developmental biology to uncover the mechanisms that lead to CDH and, ultimately, to improve outcomes for affected individuals.
Diagnosing Congenital Diaphragmatic Hernia (CDH)
Diagnosing Congenital Diaphragmatic Hernia (CDH) is crucial for ensuring timely treatment and improving outcomes for affected infants. CDH is a condition present at birth, characterized by an abnormal opening in the diaphragm that allows abdominal organs to move into the chest cavity, which can severely affect lung development and function. Understanding the common diagnostic methods and tests for CDH, as well as the importance of early diagnosis, is essential for parents, healthcare professionals, and caregivers.
Common Diagnostic Methods and Tests for CDH
Early and accurate diagnosis of CDH is vital for planning appropriate treatment strategies. The following are the most common diagnostic methods and tests used to identify CDH:
- Prenatal Ultrasound: This is the primary tool for diagnosing CDH before birth. High-resolution ultrasounds can detect the hernia by showing the abnormal position of abdominal organs in the fetal chest cavity. Prenatal ultrasounds not only help in diagnosing CDH but also allow for early intervention planning.
- Magnetic Resonance Imaging (MRI): Prenatal MRI can provide detailed images of the fetus and is useful in assessing the severity of CDH, particularly the lung-to-head ratio (LHR) and liver position, which are important for predicting outcomes.
- Fetal Echocardiography: This test evaluates the fetal heart to check for any associated heart defects and to assess the impact of CDH on heart function.
- Postnatal Imaging: After birth, chest X-rays, ultrasounds, and computed tomography (CT) scans are used to confirm the diagnosis and to plan surgical intervention. These imaging tests provide detailed views of the herniated organs and the condition of the diaphragm.
The Importance of Early Diagnosis
Early diagnosis of CDH is crucial for several reasons:
- Improved Planning and Outcomes: Early detection allows healthcare teams to prepare for immediate intervention after birth, which is often necessary for babies with CDH. This can include arranging for delivery in a facility equipped to handle high-risk neonates and planning for potential surgical repair.
- Better Management of Complications: Early diagnosis helps in anticipating and managing potential complications, such as respiratory distress and pulmonary hypertension, which are common in babies with CDH.
- Informed Decision Making: For expectant parents, early diagnosis provides valuable information for making informed decisions about care and treatment options, including the possibility of fetal surgery in certain cases.
- Enhanced Research Opportunities: Early identification of CDH can also facilitate enrollment in clinical trials, offering access to experimental treatments and contributing to research that can improve outcomes for future patients.
However, diagnosing Congenital Diaphragmatic Hernia as early as possible is essential for optimizing care and improving the prognosis for affected infants. Through the use of advanced diagnostic methods and tests, healthcare providers can effectively identify CDH and plan appropriate interventions, significantly enhancing the quality of life for these patients. Early diagnosis not only supports better clinical outcomes but also provides families with the knowledge and resources needed to navigate the challenges of CDH.
Treatment Options for Congenital Diaphragmatic Hernia (CDH)
Addressing CDH effectively requires a comprehensive treatment approach, combining surgical interventions, non-surgical treatments, and supportive care. Understanding these options is crucial for parents and caregivers to navigate the journey towards their child’s recovery.
Surgical Interventions and Their Timing
Surgery is the cornerstone of treating CDH, aimed at repositioning the displaced organs into the abdomen and repairing the diaphragmatic defect. The timing of surgical intervention is critical and is carefully determined by a multidisciplinary team of specialists based on the baby’s overall health, lung development, and stability.
- Immediate Postnatal Surgery: In cases where the baby is stable, surgery may be performed shortly after birth. This approach is less common and typically reserved for less severe cases.
- Delayed Surgery: More commonly, surgery is delayed to allow time for the stabilization of the baby’s condition, particularly their respiratory status. This may involve the use of mechanical ventilation, medications to improve lung function, and other supportive measures to ensure the baby is in the best possible condition for surgery.
Non-Surgical Treatments and Supportive Care Options
In addition to surgical repair, non-surgical treatments and supportive care are vital in managing CDH and its complications, especially before and after surgery.
- Respiratory Support: Many babies with CDH require assistance with breathing. This can include mechanical ventilation, oxygen therapy, and nitric oxide therapy to help improve oxygenation.
- Nutritional Support: Nutritional support is essential for growth and recovery. In some cases, this may involve tube feeding or total parenteral nutrition (TPN) if the baby is unable to feed by mouth or absorb nutrients efficiently.
- Medications: Medications may be used to treat pulmonary hypertension (high blood pressure in the lungs), a common complication of CDH, and to support overall heart and lung function.
Outcomes and Prognosis After Treatment
The prognosis for babies with CDH has improved significantly over the years, thanks to advances in surgical techniques, neonatal care, and supportive therapies. However, outcomes can vary widely based on the severity of the hernia, the presence of other anomalies, and the baby’s condition at birth.
- Survival Rates: With modern treatment strategies, the survival rate for babies with CDH is approximately 70-90%, although this can vary based on individual factors.
- Long-Term Health: Children who survive CDH may face long-term health issues, including respiratory problems, gastrointestinal difficulties, and developmental delays. Ongoing follow-up with a multidisciplinary team is essential to address these challenges and support the child’s development.
However, the treatment of Congenital Diaphragmatic Hernia is multi-faceted, involving timely surgical intervention, comprehensive non-surgical treatments, and extensive supportive care. Each child’s treatment plan is customized to their specific needs, with the goal of not only survival but also optimizing quality of life. Advances in medical science continue to improve outcomes for CDH patients, offering hope to affected families.
Living with Congenital Diaphragmatic Hernia
Living with Congenital Diaphragmatic Hernia (CDH) presents unique challenges for individuals and their families. This condition, where a hole in the diaphragm allows abdominal organs to move into the chest, can have significant long-term effects on health and development. Understanding the importance of long-term care and the resources available for support is crucial for managing CDH effectively.
Long-term Care and Monitoring for Individuals with CDH
Long-term care for individuals with CDH involves a multidisciplinary approach to address the various health challenges that may arise. Regular follow-ups with a healthcare team are essential to monitor growth, respiratory function, and overall development. This team may include pediatric surgeons, pulmonologists, gastroenterologists, and other specialists depending on the individual’s needs.
Key Aspects of Long-term Care Include:
- Regular Health Check-ups: Routine visits to healthcare providers are crucial for early detection and management of potential complications, such as respiratory infections or nutritional deficiencies.
- Respiratory Support: Some individuals may require ongoing respiratory support, including oxygen therapy or ventilatory assistance, to manage chronic lung disease associated with CDH.
- Nutritional Management: Nutritional support and dietary planning can help address growth and developmental concerns, ensuring individuals receive the necessary nutrients for optimal health.
- Developmental Assessments: Regular assessments with a developmental pediatrician can help identify and address any delays or challenges in physical, emotional, or cognitive development.
Support Resources for Families and Caregivers
The journey with CDH is not just a medical challenge but also an emotional and practical one for families and caregivers. Accessing support resources can provide much-needed assistance and relief.
Valuable Resources Include:
- Support Groups: Joining a support group, whether online or in-person, can connect families with others who understand the unique challenges of living with CDH. These communities offer emotional support, practical advice, and a sense of belonging.
- Educational Material: Many organizations and healthcare providers offer educational resources that help families understand CDH, its treatments, and how to care for someone with this condition.
- Financial Assistance Programs: The cost of long-term medical care can be overwhelming. Various foundations and charities offer financial assistance programs to help cover medical expenses, travel for treatment, and other costs associated with care.
- Mental Health Services: Access to mental health professionals, such as counselors or psychologists, can support families and caregivers in managing stress, anxiety, and the emotional toll of CDH.
By understanding the needs of individuals with CDH and utilizing available resources, families and caregivers can navigate the challenges of this condition more effectively. Embracing a proactive approach to care and support can lead to improved outcomes and a better quality of life for those affected by CDH.
Prevention and Research Advances in Congenital Diaphragmatic Hernia (CDH)
Preventing Congenital Diaphragmatic Hernia (CDH)
While the exact cause of Congenital Diaphragmatic Hernia (CDH) remains largely unknown, current research focuses on identifying potential risk factors and preventive measures to reduce the incidence of CDH. Studies are exploring the genetic, environmental, and maternal health factors that could contribute to the development of CDH in fetuses. Efforts include analyzing family health histories to identify any genetic predispositions and examining the impact of maternal lifestyle, diet, and exposure to certain medications or environmental toxins during pregnancy.
Advancements in prenatal screening and diagnostics are also playing a crucial role in early detection. Innovative ultrasound techniques and genetic testing can now identify CDH earlier in pregnancy, allowing for better preparation and immediate intervention after birth if necessary. While prevention may not always be possible, understanding and minimizing risk factors is a key area of focus for researchers aiming to decrease the prevalence of CDH.
Advances in Treatment and Management
The treatment and management of Congenital Diaphragmatic Hernia have seen significant advancements, improving the survival rate and quality of life for affected infants. One of the most notable advances is the development of fetal surgical procedures. These involve repairing the diaphragmatic hernia before birth, offering a better outcome for the baby by reducing the risk of lung damage and other complications associated with CDH.
Postnatal care has also evolved, with a focus on minimizing invasive procedures and supporting the infant’s ability to breathe independently. This includes the use of gentle ventilation techniques, oxygen therapy, and, in some cases, extracorporeal membrane oxygenation (ECMO) to support the heart and lungs. Research into the optimal timing and method of surgical repair post-birth is ongoing, with the goal of improving long-term respiratory and developmental outcomes.
Moreover, the management of CDH now often involves a multidisciplinary team approach, including pediatric surgeons, neonatologists, respiratory therapists, nutritionists, and physical therapists. This comprehensive care model ensures that all aspects of the infant’s health are addressed, from immediate postnatal care to long-term developmental support.
However, while CDH remains a challenging condition, ongoing research into prevention and the continuous advancement in treatment and management techniques are offering new hope to affected families. These developments not only aim to improve survival rates but also focus on enhancing the quality of life for infants with CDH, paving the way for a future where the impact of this condition is significantly mitigated.
FAQs on Congenital Diaphragmatic Hernia (CDH)
What is Congenital Diaphragmatic Hernia (CDH)?
Congenital Diaphragmatic Hernia (CDH) is a birth defect characterized by the abnormal development of the diaphragm, the muscle that helps in breathing. This condition allows abdominal organs to move into the chest, which can lead to severe complications in lung development and function.
What causes CDH?
The exact cause of CDH is not known. It is believed to result from a combination of genetic and environmental factors during fetal development. No specific action or condition during pregnancy has been definitively linked to causing CDH.
How common is CDH?
CDH occurs in approximately 1 in every 2,500 to 5,000 live births. It is considered a rare condition but has significant impacts on affected infants and their families.
What are the symptoms of CDH?
Symptoms of CDH can vary but typically include difficulty breathing, rapid breathing (tachypnea), a bluish tint to the skin (cyanosis), and underdevelopment of the lung (pulmonary hypoplasia) on the affected side. The severity of symptoms depends on the size of the hernia and the extent of lung underdevelopment.
How is CDH diagnosed?
CDH is often diagnosed before birth through prenatal ultrasound, which can show the herniation of abdominal organs into the chest cavity. After birth, additional imaging tests, such as an MRI or CT scan, can help determine the extent of the condition.
What treatment options are available for CDH?
Treatment for CDH typically involves surgical repair of the diaphragm, which is often performed after the baby is stabilized and the lungs are sufficiently developed. In severe cases, treatments like extracorporeal membrane oxygenation (ECMO) may be used to support the baby’s breathing until surgery is possible.
Can CDH be cured?
With early diagnosis and appropriate treatment, many children with CDH can lead healthy lives. However, they may require long-term medical follow-up to manage complications or health issues related to their condition, such as respiratory problems or developmental delays.
How can I support a child with CDH?
Supporting a child with CDH involves providing emotional and physical care, ensuring they receive necessary medical treatment, and possibly working with a team of specialists, including pediatric surgeons, pulmonologists, and physical therapists. Joining a support group for families affected by CDH can also provide valuable information and emotional support.
Conclusion
In summary, understanding the symptoms and recognizing the underlying causes of Congenital Diaphragmatic Hernia (CDH) is crucial for timely diagnosis and effective treatment. CDH is a condition that requires immediate attention due to its potential complications and impact on a newborn’s health. By being aware of the signs such as difficulty breathing, a blue appearance of the skin, and abnormal chest development, parents and caregivers can act swiftly in seeking medical advice.
We cannot overemphasize the importance of consulting healthcare professionals if there are any concerns regarding CDH. Early intervention by specialists can significantly improve the outcome for affected infants, providing them with the best possible chance at a healthy life. Remember, healthcare providers are there to support and guide you through understanding the condition, evaluating the risks, and making informed decisions about the necessary treatments.
In closing, while the diagnosis of CDH can be daunting for any family, advancements in medical science have greatly improved the prognosis for many children. Encouragement, support, and open communication with your healthcare team are key elements in navigating the journey ahead. Your proactive approach in recognizing potential symptoms and seeking expert advice can make a profound difference in the health and well-being of your child.