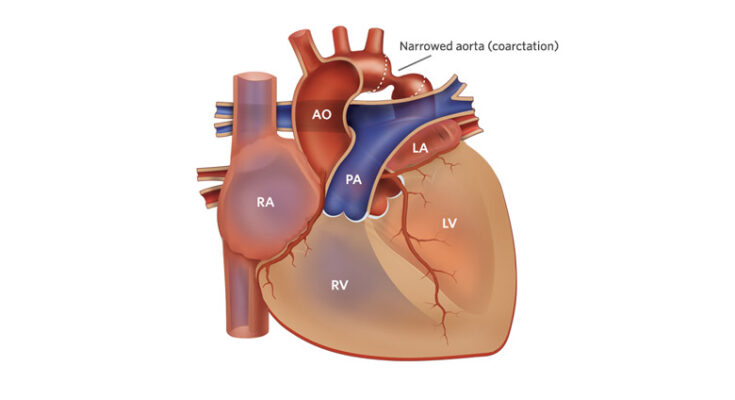
Coarctation of the Aorta Treatment: Coarctation of the aorta (CoA) is a congenital heart defect characterized by the narrowing of the aorta, the major artery that carries oxygen-rich blood from the heart to the body.
This condition can lead to significant health issues, including high blood pressure, heart failure, and damage to the heart and other organs due to restricted blood flow.
What is Coarctation of the Aorta?
Coarctation of the Aorta (CoA) is a congenital heart defect characterized by a narrowing of the aorta, the main artery that carries oxygen-rich blood from the heart to the rest of the body. This condition can lead to significant health issues, including high blood pressure, heart damage, and stroke. Understanding CoA, its prevalence, risk factors, and how it impacts heart function and blood flow is crucial for those affected and their families.
Epidemiology: Prevalence and Risk Factors
Coarctation of the Aorta is relatively rare, affecting approximately 1 in every 2,500 births. It can occur as a standalone heart defect or alongside other congenital heart anomalies. Risk factors for developing CoA include genetic conditions, such as Turner syndrome, and familial heart defects, indicating a potential genetic component to the condition. Moreover, males are slightly more likely to be affected than females.
Pathophysiology: How CoA Affects Heart Function and Blood Flow
The pathophysiology of Coarctation of the Aorta revolves around its impact on heart function and blood flow. The narrowing of the aorta increases resistance to blood flow, forcing the heart to work harder to pump blood through the body. This additional strain can lead to hypertrophy of the left ventricle, the heart’s main pumping chamber, and eventually heart failure if left untreated.
The increased pressure before the narrowing and decreased pressure beyond it can lead to a range of complications. For instance, high blood pressure in the upper body can damage the heart and kidneys, while the lower body may receive insufficient blood flow, affecting growth and development in children and causing leg pain during exercise in adults.
Early detection and treatment of Coarctation of the Aorta are vital to prevent serious complications. Treatments may include surgical repair or balloon angioplasty, depending on the severity of the narrowing and the presence of other heart defects. With appropriate management, individuals with CoA can lead healthy and active lives.
Signs and Symptoms of Coarctation of the Aorta
Recognizing these symptoms early can lead to timely diagnosis and treatment, preventing serious complications.
Early Signs in Infants and Children
In infants and young children, coarctation of the aorta may present several noticeable signs. These early indicators can include:
- Difficulty Feeding: Infants may have trouble feeding or may tire easily during feeds.
- Failure to Thrive: Affected infants might not gain weight or grow as expected.
- Breathing Problems: Shortness of breath or heavy breathing can occur due to the heart working harder to pump blood through the narrowed aorta.
- Irritability: Infants may be more irritable than usual.
- Pale Skin: The skin may appear paler than normal, indicating reduced blood flow.
- Weak Pulse or Blood Pressure Difference: A weaker pulse in the lower limbs compared to the arms, or a significant difference in blood pressure between the arms and legs, can be a hallmark sign of CoA.
Symptoms in Adolescents and Adults
In older children, adolescents, and adults, coarctation of the aorta might not be as readily apparent, with some individuals experiencing mild symptoms or none at all until later in life. When symptoms do occur, they can include:
- High Blood Pressure: Elevated blood pressure, especially if it is resistant to treatment, can be a significant indicator of CoA.
- Headaches: Persistent headaches may be a symptom.
- Leg Fatigue or Cramps: Weakness, cramps, or pain in the legs, especially during exercise, due to reduced blood flow.
- Nosebleeds: Frequent nosebleeds can be associated with high blood pressure.
- Cold Feet or Lower Legs: Reduced blood flow to the lower body can make the feet or lower legs feel cold to the touch.
- Chest Pain or Heart Murmur: In some cases, a heart murmur or chest pain might be present.
Complications if Left Untreated
Untreated coarctation of the aorta can lead to several serious complications over time. These complications underscore the importance of early diagnosis and intervention:
- Hypertension: Persistent high blood pressure can strain the heart and arteries, leading to a higher risk of heart attack and stroke.
- Aortic Rupture or Dissection: The increased pressure can cause the aorta to tear or rupture, a life-threatening emergency.
- Heart Failure: Over time, the heart may become weak from overworking, leading to heart failure.
- Stroke: High blood pressure associated with CoA increases the risk of having a stroke.
- Endocarditis: This is an infection of the inner lining of the heart chambers and heart valves, more common in people with heart defects like CoA.
If you or someone you know exhibits any of these symptoms, consulting with a healthcare provider for evaluation and possible treatment is advisable to prevent the onset of severe complications.
Diagnosis of Coarctation of the Aorta
Early diagnosis is crucial for the management and treatment of CoA. This guide outlines the steps and methodologies used in diagnosing Coarctation of the Aorta, focusing on physical examinations, imaging studies, and cardiac catheterization.
Physical Examination Findings and Initial Suspicions
The diagnosis of Coarctation of the Aorta often begins with a physical examination. Medical professionals look for specific signs that suggest a narrowing of the aorta. Key indicators include:
- High Blood Pressure: Elevated blood pressure in the arms compared to lower readings in the legs is a hallmark sign.
- Weak or Delayed Pulse: A weak or delayed pulse in the groin area, as compared to the arms, can indicate CoA.
- Heart Murmurs: An unusual heart sound, known as a murmur, might be detected when listening to the heart with a stethoscope. This murmur, caused by turbulent blood flow, can point towards CoA.
- Physical Symptoms: Symptoms such as difficulty breathing, failure to thrive in infants, or leg cramps during exercise in older children and adults may raise initial suspicions of CoA.
Imaging Studies for CoA Diagnosis
Following the initial physical examination, imaging studies are crucial for confirming the diagnosis of Coarctation of the Aorta. These studies provide detailed images of the heart and the aorta, helping to identify the location and severity of the narrowing. The most commonly used imaging techniques include:
- Echocardiography: An echocardiogram uses sound waves to create images of the heart and aorta. It’s often the first imaging test used, as it can provide detailed pictures of the heart’s structure and function.
- Magnetic Resonance Imaging (MRI): MRI is a powerful tool for visualizing the aorta and detecting CoA. It offers detailed images of the heart and blood vessels without using ionizing radiation.
- Computed Tomography (CT) Scan: A CT scan combines multiple X-ray images to create a detailed cross-sectional view of the body. With contrast material, it can clearly show the narrowing of the aorta and any associated anomalies.
Cardiac Catheterization: Purpose and Process
Cardiac catheterization is both a diagnostic and therapeutic procedure used in the management of Coarctation of the Aorta. While imaging studies can suggest the presence of CoA and provide details about its location and severity, cardiac catheterization offers definitive diagnosis and treatment options. The procedure involves:
- Insertion of a Catheter: A thin, flexible tube is inserted into a blood vessel, usually in the groin, and guided to the heart and aorta.
- Dye Injection: A special dye is injected through the catheter, making the heart and blood vessels visible on X-ray images. This highlights the narrowed section of the aorta.
- Pressure Measurement: The procedure also allows for the measurement of blood pressure on both sides of the narrowed area, providing insight into the severity of the condition.
Cardiac catheterization not only confirms the diagnosis of CoA but can also be used to treat the condition. Balloon angioplasty or stent placement can be performed during catheterization to widen the narrowed section of the aorta.
However, the diagnosis of Coarctation of the Aorta involves a comprehensive approach, starting with a detailed physical examination and followed by advanced imaging studies. When necessary, cardiac catheterization provides definitive diagnosis and treatment options, highlighting the importance of a multidisciplinary approach in managing this congenital heart defect. Early detection and accurate diagnosis are key to improving outcomes for individuals with CoA.
Treatment Options for Coarctation of the Aorta
Coarctation of the aorta, a congenital heart defect characterized by the narrowing of the aorta, requires timely and effective treatment to improve blood flow and reduce the risk of complications. This article explores the immediate management strategies for critical cases, surgical and non-surgical treatment approaches, and discusses the advantages and potential risks associated with each method.
Immediate Management Strategies for Critical Cases
In critical cases, especially in newborns and infants, immediate management of coarctation of the aorta is crucial to stabilize the patient. Initial treatment often involves medical therapy to improve heart function and increase blood flow to the body. Medications such as prostaglandin E1 can be administered to keep the ductus arteriosus open, allowing for better circulation until definitive treatment can be provided. This approach is usually a temporary solution aimed at stabilizing the condition before more permanent treatment options are pursued.
Surgical Treatment Approaches
Surgery is a common and effective treatment for coarctation of the aorta and is often recommended for infants and young children. The surgical methods include:
- Resection and End-to-End Anastomosis: This procedure involves removing the narrowed section of the aorta and reconnecting the two ends. It is the most common surgical approach and is highly effective in many patients.
- Subclavian Flap Aortoplasty: In this method, a portion of the subclavian artery is used to enlarge the narrowed area of the aorta.
- Patch Aortoplasty: This involves sewing a patch of synthetic material or part of the arterial tissue to widen the constricted area.
- Bypass Graft Repair: A graft is used to bypass the narrowed section of the aorta.
Each surgical method has its advantages, such as high success rates and the potential for a permanent solution. However, risks such as re-narrowing of the aorta, bleeding, infection, and issues related to anesthesia are also present.
Non-Surgical Interventions
For some patients, particularly adolescents and adults, non-surgical interventions like balloon angioplasty and stenting may be preferred. Balloon angioplasty involves inserting a catheter with a balloon at its tip into the narrowed area and then inflating the balloon to widen the aorta. Stenting involves placing a metal mesh tube (stent) in the narrowed area to keep it open.
These non-surgical approaches offer advantages such as shorter recovery times, less pain, and the avoidance of major surgery. However, there are potential risks, including damage to the aorta, bleeding, and the possibility of needing additional procedures in the future if the area narrows again or if the stent moves.
Advantages and Potential Risks of Each Treatment Method
Each treatment method for coarctation of the aorta offers unique advantages and comes with its own set of risks. Surgical treatments are often considered more permanent solutions with a successful track record in young patients. Non-surgical interventions, while less invasive, may require further treatment down the line and carry risks of procedural complications.
When deciding on a treatment plan, it’s essential to consider the patient’s age, the severity of the condition, and overall health. A multidisciplinary team approach, involving cardiologists, cardiac surgeons, and other specialists, is critical to tailor the treatment plan to the individual’s needs, maximizing the benefits while minimizing the risks.
Understanding the options available for treating coarctation of the aorta is the first step toward effective management. With advances in medical and surgical treatments, most individuals with this condition can look forward to a healthier future.
Post-Treatment Care and Monitoring of Coarctation of the Aorta (CoA)
After receiving treatment for Coarctation of the Aorta (CoA), a condition characterized by the narrowing of the aorta, follow-up care and monitoring are crucial for ensuring a healthy recovery and maintaining long-term wellness. This article outlines essential aspects of post-treatment care, the long-term outlook for patients, management of potential complications, and recommended lifestyle adjustments for those who have undergone CoA treatment.
Follow-Up Care Essentials
Once treatment for CoA has been completed, regular follow-up appointments are essential. These appointments allow healthcare providers to monitor the patient’s progress, ensure the aorta is functioning correctly, and detect any signs of recurrence or complications early. Follow-up care typically includes:
- Routine Imaging Tests: Echocardiograms, MRI, or CT scans may be performed regularly to evaluate the aorta’s condition and monitor for any changes.
- Blood Pressure Monitoring: Since hypertension can occur after CoA treatment, regular blood pressure checks are crucial.
- Cardiac Function Tests: Tests such as electrocardiograms (ECG) to assess the heart’s electrical activity and exercise stress tests to evaluate heart and lung function during physical activity.
Long-Term Outlook After CoA Treatment
The long-term outlook for individuals treated for CoA is generally positive, especially when the condition is corrected early in life. Many patients lead normal, active lives with few restrictions. However, regular follow-up care is vital to manage any ongoing health concerns and prevent complications.
Management of Potential Long-Term Complications
While the prognosis after CoA treatment is often favorable, some individuals may face potential long-term complications, such as:
- Re-narrowing of the Aorta (Recoarctation): A condition that may require additional interventions.
- Hypertension: Even after successful treatment, some patients may develop high blood pressure, necessitating ongoing management.
- Heart and Vascular Problems: Including increased risk of coronary artery disease, aneurysms, or stroke, underscoring the need for lifelong monitoring.
Addressing these complications early through regular check-ups and testing is critical for maintaining heart health.
Lifestyle Adjustments and Preventive Care
Adopting a heart-healthy lifestyle is an important part of post-treatment care for CoA. Patients are encouraged to:
- Maintain a Healthy Diet: Focusing on fruits, vegetables, whole grains, and lean proteins can help manage blood pressure and prevent heart disease.
- Exercise Regularly: Following a tailored exercise plan can strengthen the heart and improve overall cardiovascular health.
- Avoid Smoking and Limit Alcohol: These substances can adversely affect heart health and should be avoided or consumed in moderation.
- Regular Health Screenings: Including cholesterol levels and diabetes screenings to identify and manage risk factors for heart disease.
Post-treatment care and monitoring for Coarctation of the Aorta are critical components of a comprehensive recovery plan. By adhering to follow-up care schedules, managing potential complications, and making lifestyle adjustments, individuals who have undergone CoA treatment can enjoy a healthy, active life. Regular communication with healthcare providers is key to navigating this journey successfully, ensuring any concerns are addressed promptly for the best long-term outcomes.
Innovations in Coarctation of the Aorta Treatment
Coarctation of the aorta (CoA) is a congenital heart defect characterized by a narrowing of the aorta, the main artery carrying blood from the heart to the body. This condition can lead to hypertension, heart damage, and other serious health issues if not treated effectively. Fortunately, the field of CoA treatment has seen significant innovations in recent years, both in surgical procedures and non-surgical interventions, alongside promising research that could reshape future treatment strategies.
Recent Advances in Surgical and Non-Surgical Treatments
The landscape of CoA treatment has evolved with the introduction of advanced surgical techniques and non-surgical interventions that offer improved outcomes and reduced risks for patients.
Surgical Innovations: Traditionally, open-heart surgery was the standard approach to correct CoA, involving cutting through the chest wall to repair the narrowed artery. However, recent innovations have led to the development of less invasive surgical methods, such as end-to-end anastomosis and subclavian flap aortoplasty. These techniques require smaller incisions, leading to quicker recovery times and less postoperative pain for patients.
Non-Surgical Interventions: Catheter-based procedures have revolutionized CoA treatment, offering a minimally invasive alternative to traditional surgery. Balloon angioplasty and stenting are two prominent examples, where a catheter is inserted into a blood vessel in the groin and guided to the site of the narrowing. The balloon is then inflated to widen the artery, and a stent is often placed to keep the artery open. These procedures are particularly beneficial for patients who are not ideal candidates for surgery or those with recurrent coarctation.
Emerging Research and Its Implications for Future Treatment
The future of CoA treatment is bright, with ongoing research focusing on novel therapeutic approaches and technologies. One area of investigation is the development of bioresorbable stents, which would gradually dissolve after correcting the artery narrowing, potentially reducing the risk of long-term complications associated with metal stents.
Another promising research avenue is the application of gene therapy to treat or even prevent CoA. Scientists are exploring how genetic modifications can promote the growth of the aorta in patients with coarctation, aiming to offer a more permanent solution than current treatments.
Furthermore, advancements in imaging technologies and computational modeling are enhancing the precision of CoA diagnosis and treatment planning. These tools allow for more accurate assessments of the aorta’s structure and blood flow, enabling personalized treatment strategies that can improve outcomes for patients.
Innovations in the treatment of coarctation of the aorta have significantly improved the prognosis for individuals affected by this condition. With the advent of less invasive surgical techniques, catheter-based interventions, and ongoing research into novel therapies, the future holds promise for even more effective and personalized approaches to CoA treatment. As these innovations continue to develop, they will undoubtedly enhance the quality of life for patients with CoA and offer new hope for those facing this challenging condition.
FAQ Section: Coarctation of the Aorta
What is Coarctation of the Aorta?
Coarctation of the Aorta (CoA) is a congenital heart defect characterized by a narrowing of the aorta, the main artery carrying oxygen-rich blood from the heart to the body. This narrowing can increase blood pressure above the constriction and reduce blood flow to the lower part of the body.
What causes Coarctation of the Aorta?
The exact cause of CoA is not fully understood, but it is believed to develop during fetal growth. The condition is often associated with genetic conditions, such as Turner syndrome, and can occur with other heart defects.
How is Coarctation of the Aorta diagnosed?
CoA is typically diagnosed through a combination of physical examinations, imaging tests, and cardiac catheterization. Symptoms such as high blood pressure, weak pulses in the lower extremities, or a heart murmur may prompt further investigation. Imaging tests like echocardiograms, MRI, or CT scans provide detailed images of the heart and aorta, helping to identify the narrowing.
What are the symptoms of Coarctation of the Aorta?
Symptoms can vary depending on the severity of the condition. In infants, signs may include difficulty breathing, poor feeding, and failure to thrive. Older children and adults might experience high blood pressure, leg cramps or weakness after exercise, and cold feet or legs.
How is Coarctation of the Aorta treated?
Treatment depends on the age at diagnosis and the severity of the condition. Options include surgical repair or balloon angioplasty. Surgery involves removing the narrowed section of the aorta and reconnecting the two ends or using a patch to widen the area. Balloon angioplasty uses a catheter with a balloon to stretch open the narrowed segment.
Can Coarctation of the Aorta be cured?
While CoA can be effectively treated, patients will require lifelong follow-up care to monitor their cardiovascular health. Treatment can alleviate symptoms and improve quality of life, but ongoing monitoring is essential for detecting potential complications, such as re-narrowing of the aorta or high blood pressure.
What is the long-term outlook for someone with Coarctation of the Aorta?
With proper treatment and regular follow-up care, most individuals with CoA can lead healthy, active lives. However, the condition does require ongoing management to address any complications and to ensure the heart and aorta function optimally.
Can Coarctation of the Aorta be prevented?
Since CoA is a congenital condition, it cannot be prevented. However, early diagnosis and treatment can prevent complications and significantly improve outcomes. Pregnant women are encouraged to receive regular prenatal care, which may help in early detection of congenital heart defects.
Conclusion
Current treatments for CoA range from less invasive procedures like balloon angioplasty to surgical interventions such as end-to-end anastomosis or the placement of a stent. The choice of treatment depends on various factors, including the age of the patient, the severity of the narrowing, and the presence of other heart defects. The effectiveness of these treatments is well-documented, with many patients leading normal, active lives post-intervention.
For individuals experiencing symptoms of CoA, such as shortness of breath, chest pain, or high blood pressure, or those who have risk factors, seeking medical advice cannot be overstated. Early consultation with a healthcare provider can lead to early diagnosis, which is key to accessing effective treatments and improving outcomes.
In conclusion, understanding the importance of early detection and the effectiveness of current treatments for Coarctation of the Aorta is vital. It empowers individuals to seek medical advice promptly if they have symptoms or risk factors. Remember, early intervention can make a significant difference in the management of CoA, enabling individuals to enjoy a healthier life.