Chagas Disease Treatment: Chagas Disease, also known as American trypanosomiasis, is a tropical parasitic disease caused by the Trypanosoma cruzi parasite.
This condition primarily affects populations in Latin America but has spread to other parts of the world due to globalization and migration.
Understanding its diagnosis and treatment is crucial for managing and controlling the spread of this disease.
What is Chagas Disease
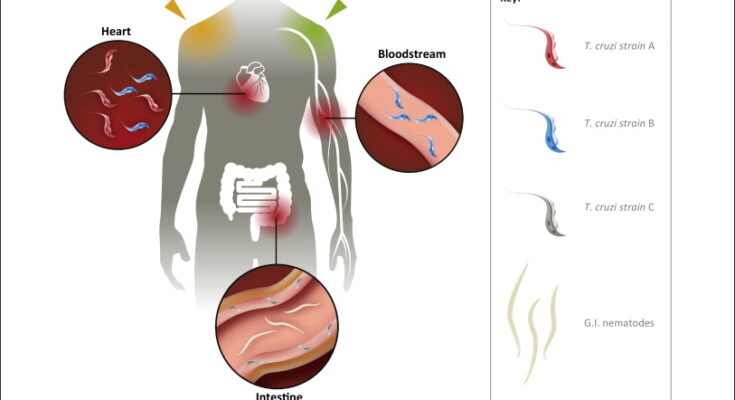
Chagas disease, also known as American trypanosomiasis, is a tropical parasitic infection caused by the protozoan parasite Trypanosoma cruzi. It is a significant public health concern in Latin America, where it is primarily transmitted through the feces of infected triatomine bugs, commonly referred to as “kissing bugs.” These insects feed on human blood and release the parasite into the bite wound or mucous membranes, leading to infection.
Transmission Pathways
Chagas disease can be transmitted through several pathways, each posing unique challenges in preventing and controlling the spread of the disease. These pathways include:
- Vector-borne Transmission: The most common route of transmission is through the bite of infected triatomine bugs. When these bugs feed on human blood, they excrete feces containing T. cruzi parasites, which can then enter the body through the bite wound or mucous membranes.
- Congenital Transmission: Pregnant women infected with T. cruzi can pass the parasite to their unborn children, leading to congenital Chagas disease. This mode of transmission underscores the importance of screening and treatment for pregnant women in endemic areas.
- Blood Transfusion and Organ Transplantation: Before the implementation of screening protocols, Chagas disease could be transmitted through transfusions of infected blood or the transplantation of infected organs. Nowadays, rigorous screening processes have significantly reduced these risks in many countries.
- Oral Transmission: Although less common, Chagas disease can also be transmitted orally through the consumption of food or beverages contaminated with T. cruzi parasites. Outbreaks of oral transmission have been reported, emphasizing the need for proper food handling and hygiene practices.
Stages of Chagas Disease and Their Symptoms
Chagas disease progresses through two main stages, each with distinct symptoms and health implications:
- Acute Stage: The initial phase of the infection can last for several weeks to months. During this time, symptoms may be mild or even absent. When symptoms do occur, they can include fever, fatigue, body aches, headache, rash, loss of appetite, diarrhea, and vomiting. Swelling at the infection site (where the parasite entered the body) or swelling of the eyelids (Romana’s sign) may also be observed.
- Chronic Stage: After the acute phase, the disease can enter a chronic stage, which can last for years or even decades without any symptoms. However, approximately 30% of infected individuals will develop serious cardiac, digestive, or neurological complications. Symptoms of chronic Chagas disease may include irregular heartbeats, heart failure, enlarged esophagus or colon, leading to difficulties in eating or passing stool.
However, Chagas disease remains a significant health challenge, particularly in Latin America but also in other regions due to global migration. Understanding its transmission pathways and recognizing the symptoms of its acute and chronic stages are crucial for early detection, effective treatment, and ultimately, reducing its spread and impact on affected populations. Public health efforts focus on vector control, screening blood and organ donations, and improving diagnosis and access to care for those at risk of or living with Chagas disease.
Diagnosis of Chagas Disease
Importance of Early and Accurate Diagnosis
The early and accurate diagnosis of Chagas disease is paramount for effective management and treatment of this potentially life-threatening condition. Chagas disease, caused by the Trypanosoma cruzi parasite, can lead to serious cardiac and digestive system complications if not treated promptly. Early detection allows for the initiation of antiparasitic treatments that can significantly reduce the risk of chronic complications and improve the quality of life for patients. Furthermore, accurate diagnosis helps in preventing the transmission of the disease, as individuals diagnosed in the acute phase can take steps to avoid donating blood or organs, which are potential modes of transmission.
List of Diagnostic Methods
Several diagnostic methods are employed to detect Chagas disease, each with its own specific use case:
- Serological Tests: These are the most commonly used methods for diagnosing chronic Chagas disease. They detect antibodies against T. cruzi in the blood. Examples include ELISA, indirect immunofluorescence, and Western blot assays.
- Parasitological Tests: Direct visualization of the parasite in blood samples is possible in the acute phase of the disease. Techniques such as microscopic examination of fresh blood or its derivatives (e.g., buffy coat) are used.
- Molecular Tests: Polymerase Chain Reaction (PCR) is used to detect T. cruzi DNA in blood samples. This method is particularly useful in the acute phase and for congenital transmissions.
- Xenodiagnosis and Hemoculture: These methods involve culturing the parasite or using a clean, laboratory-bred triatomine bug to feed on the patient’s blood, then checking the bug for infection. They are more often used in research settings.
Challenges in Diagnosing Chagas Disease
Diagnosing Chagas disease poses several challenges:
- Symptom Overlap: The initial symptoms are nonspecific and can overlap with other diseases, making early diagnosis difficult.
- Sensitivity and Specificity: Some diagnostic tests may not be sensitive or specific enough, leading to false negatives or positives.
- Access to Testing: In endemic regions, access to diagnostic facilities and advanced testing methods can be limited.
- Chronic Phase Detection: In the chronic phase, the low parasitemia levels make direct detection of the parasite challenging.
Recent Advancements in Diagnostic Technologies
Recent advancements in the diagnostic technologies for Chagas disease are aimed at overcoming these challenges:
- Improved Serological Tests: Newer serological assays with higher sensitivity and specificity are being developed, facilitating more accurate diagnosis.
- Point-of-Care (POC) Tests: Portable, rapid diagnostic tests that can be used in field settings are becoming available, improving access to diagnosis in remote areas.
- Molecular Techniques: Enhancements in PCR and the development of novel molecular markers have increased the sensitivity of detecting T. cruzi DNA, even at low parasitemia levels.
- Biomarker Discovery: Research into identifying specific biomarkers of infection and disease progression is ongoing, which could lead to more precise diagnostic tools.
The continuous improvement and adaptation of diagnostic methods are crucial in the fight against Chagas disease. Early and accurate diagnosis remains a cornerstone of effective disease management, reducing the burden of Chagas disease and preventing its spread.
Treatment Options for Chagas Disease
Effective management of this disease requires a comprehensive understanding of the available treatment options. This section aims to elucidate the goals, strategies, and specifics of treatments for Chagas disease, enhancing its manageability and outcomes for affected individuals.
Overview of Treatment Goals and Strategies
The primary goal of treating Chagas disease is to eliminate the Trypanosoma cruzi parasite from the infected individual’s body, thereby preventing the progression of the disease and reducing the risk of chronic complications. Treatment strategies vary depending on the stage of the disease (acute or chronic) and the presence of any complications. Early diagnosis and prompt treatment are crucial for improving the prognosis.
Antiparasitic Treatments: Nifurtimox and Benznidazole
Two main antiparasitic medications, Nifurtimox and Benznidazole, are the cornerstone treatments for Chagas disease. Both drugs are effective in killing the parasite, especially during the acute phase of the infection.
- Indications for Use: Nifurtimox and Benznidazole are recommended for patients diagnosed with acute Chagas disease, reactivated infections (due to immunosuppression), and in some cases, during the early chronic phase. Their use in children and adolescents tends to be more effective, with better outcomes reported.
- Dosage and Duration: The dosage and duration of treatment with Nifurtimox and Benznidazole depend on the patient’s age, weight, and the severity of the disease. Typically, treatment lasts around 60 to 90 days. It is essential for healthcare providers to adjust dosages appropriately to maximize efficacy while minimizing potential side effects.
- Side Effects and Management: While effective, these medications can cause side effects, including skin rashes, digestive disturbances, and neuropathy. Regular monitoring and supportive care can help manage these side effects. In some cases, dosage adjustments or discontinuation may be necessary.
Symptomatic Treatments and Management of Chronic Complications
In addition to antiparasitic therapy, symptomatic treatment is vital for managing the signs and symptoms of Chagas disease, especially in its chronic stages. This includes managing cardiac and gastrointestinal complications through medications, lifestyle modifications, and, in some cases, surgical interventions.
Importance of Treatment During Different Stages of the Disease
The stage of Chagas disease significantly influences treatment decisions. During the acute phase, antiparasitic treatment is most effective and can lead to a cure. In the chronic phase, the focus shifts towards managing symptoms and preventing further complications. Early intervention and tailored treatment approaches are essential for improving quality of life and reducing mortality rates associated with Chagas disease.
However, managing Chagas disease requires a multi-faceted approach that includes antiparasitic treatments, symptom management, and addressing chronic complications. Understanding the treatment options available and their appropriate application is crucial for healthcare providers and patients alike in combating this challenging disease.
Prevention and Control Measures for Vector-Borne Diseases
Effective prevention and control measures are critical to mitigate the impact of these diseases. This section outlines key strategies to control vectors and prevent the transmission of vector-borne diseases, including screening blood donations and organ donors, alongside awareness and education campaigns.
Strategies for Vector Control and Prevention of Transmission
Vector control is the cornerstone of preventing and managing vector-borne diseases. Here are some effective strategies:
- Environmental Management: Modify or manage the environment to prevent the breeding of vectors. This includes removing stagnant water where mosquitoes breed, proper waste management, and improving sanitation.
- Chemical Control: Use of insecticides and larvicides to control vector populations. However, it’s crucial to use these chemicals judiciously to avoid resistance and adverse environmental impacts.
- Biological Control: Introduction of natural predators of vectors, such as certain fish species that eat mosquito larvae, can be an effective and environmentally friendly option.
- Personal Protective Measures: Encouraging the use of protective clothing, bed nets (preferably insecticide-treated nets), and repellents can significantly reduce the risk of vector bites.
Screening Blood Donations and Organ Donors
Screening blood donations and organ donors for vector-borne diseases is crucial in preventing the transmission of these diseases through medical procedures. Implementing stringent screening processes ensures that infectious agents are not transmitted to recipients, safeguarding public health. This measure is particularly important for diseases like Zika virus, West Nile virus, and malaria, which can be transmitted through blood transfusion and organ transplantation.
Awareness and Education Campaigns
Raising awareness and educating the public about vector-borne diseases and their prevention is vital. Awareness campaigns should focus on:
- Disease Knowledge: Informing the community about the symptoms, transmission, and treatment of vector-borne diseases.
- Preventive Practices: Educating on the importance of environmental management, personal protection, and the need for community participation in vector control activities.
- Community Engagement: Encouraging community involvement in vector control and environmental cleanup efforts to reduce vector breeding sites.
However, the prevention and control of vector-borne diseases require a multi-faceted approach that includes effective vector control strategies, stringent screening of blood and organ donations, and comprehensive awareness and education campaigns. By implementing these measures, communities can significantly reduce the incidence of these diseases and protect public health.
Challenges in Chagas Disease Treatment
Chagas disease, caused by the Trypanosoma cruzi parasite, is a significant public health concern, particularly in Latin America. While efforts to control and treat the disease have advanced, several challenges hinder the progress in combating Chagas disease effectively. This article explores the main obstacles in the treatment of Chagas disease, including issues related to access to diagnosis and treatment, drug resistance, and the impact of public health policies.
Access to Diagnosis and Treatment in Endemic and Non-Endemic Regions
One of the primary hurdles in managing Chagas disease is the difficulty of accessing diagnosis and treatment, especially in rural and impoverished areas where the disease is most prevalent. In endemic regions, limited healthcare infrastructure, shortage of trained healthcare professionals, and lack of awareness among the population about the disease contribute to underdiagnosis and undertreatment. Moreover, the asymptomatic nature of the early stage of the disease makes it challenging to identify and treat early cases without systematic screening programs.
In non-endemic regions, such as North America and Europe, where cases are increasingly found due to migration, there’s a lack of awareness and knowledge about Chagas disease among healthcare providers. This situation leads to misdiagnosis or delayed diagnosis, preventing timely treatment and increasing the risk of chronic complications.
Drug Resistance and the Need for New Treatments
The treatment of Chagas disease relies on two drugs, benznidazole and nifurtimox, which have been in use for over 50 years. These medications are effective primarily in the acute phase of the infection but have limited efficacy in the chronic phase and can cause significant side effects. Additionally, there is an emerging concern about the potential development of drug resistance due to the long-term use of these drugs. The limited efficacy and the side effects of the current treatments underscore the urgent need for new therapeutic options that are safer and more effective across all stages of the disease.
The Role of Public Health Policies
Public health policies play a crucial role in addressing the challenges of Chagas disease treatment. Effective policies are needed to improve access to healthcare services and to promote the integration of Chagas disease screening and treatment into primary healthcare systems, especially in endemic areas. Additionally, public health initiatives should focus on educating healthcare providers and communities about the disease to enhance early diagnosis and treatment.
Investment in research and development of new diagnostic tools and treatments is also critical. Public health policies that support collaboration between governments, non-profit organizations, and the pharmaceutical industry can facilitate the development and distribution of innovative solutions to combat Chagas disease.
Furthermore, policies aimed at vector control and housing improvements are essential in preventing the transmission of Trypanosoma cruzi and reducing the incidence of new cases. International cooperation and funding are vital to support these initiatives, particularly in resource-limited settings.
The challenges in Chagas disease treatment are multifaceted, involving complex issues related to healthcare access, drug resistance, and public health policy. Addressing these challenges requires a coordinated approach that combines improvements in healthcare infrastructure, advances in medical research, and comprehensive public health strategies. Through concerted efforts, it is possible to overcome these obstacles and move closer to effectively controlling and ultimately eliminating Chagas disease as a public health threat.
Future Directions in Chagas Disease Treatment
The battle against Chagas disease, a neglected tropical disease caused by the parasite Trypanosoma cruzi, has seen significant strides in diagnosis and treatment. However, the disease continues to affect millions worldwide, particularly in Latin America, where it is endemic. As researchers and healthcare professionals seek more effective ways to combat this disease, several key areas have emerged as critical future directions for Chagas disease treatment: research on new therapeutic agents, vaccine development, and international collaboration for disease control and elimination.
Research on New Therapeutic Agents
The development of new therapeutic agents represents a cornerstone in the future fight against Chagas disease. Current treatments, such as benznidazole and nifurtimox, offer effective solutions but come with limitations, including lengthy treatment courses and side effects that can impact patient adherence. Moreover, these treatments are less effective in the chronic stage of the disease. Hence, there is a pressing need for research into novel therapeutic agents that are more efficacious, have fewer side effects, and can be used across all stages of Chagas disease.
Innovations in drug discovery and the application of cutting-edge technology, such as CRISPR gene editing and nanotechnology, offer promising avenues for identifying and developing new drugs. These technologies can help in understanding the biology of the Trypanosoma cruzi parasite and its interaction with human hosts, paving the way for targeted treatments that could improve patient outcomes.
Vaccine Development
Although no vaccine for Chagas disease is currently available, vaccine development is an area of intense research and holds promise for a long-term solution to prevent infection. A vaccine would not only offer a proactive approach to disease management but also significantly reduce transmission rates, particularly in endemic regions.
Research efforts are focused on identifying antigens that can elicit a strong and durable immune response against the parasite. Advances in immunology and molecular biology are instrumental in these efforts, enabling scientists to design and test vaccine candidates that could eventually lead to a safe and effective vaccine for human use.
International Collaboration for Disease Control and Elimination
Chagas disease is a global health issue that requires a coordinated international response. International collaboration is essential for pooling resources, sharing research findings, and implementing cross-border initiatives to control and eventually eliminate the disease. Partnerships between endemic and non-endemic countries, along with the involvement of international health organizations, can facilitate the exchange of knowledge, improve surveillance and diagnosis, and enhance access to treatment.
Efforts such as the World Health Organization’s Global Plan to Combat Neglected Tropical Diseases and the Pan American Health Organization’s Initiative for the Elimination of Communicable Diseases are examples of how international collaboration can lead to significant progress in disease control and elimination strategies.
Conclusion
We call upon stakeholders at all levels—governments, health organizations, researchers, and the public—to intensify efforts toward increasing awareness of Chagas Disease. There’s a critical need for enhanced research initiatives to develop more effective diagnostic tools and treatments. Equally important is the need for increased funding to support these initiatives and to ensure that advancements in Chagas Disease management are accessible to all, especially those in underprivileged communities most affected by this disease.
In conclusion, tackling Chagas Disease requires a concerted, global effort to shift the tide against this life-threatening condition. By fostering greater understanding, investing in research, and securing the necessary funds, we can make significant strides in combating this disease. Let us all commit to this cause, for the sake of those suffering and at risk of Chagas Disease, to improve health outcomes and ultimately save lives.