Cervical Cancer Symptoms: Cervical cancer, a type of cancer that occurs in the cells of the cervix — the lower part of the uterus that connects to the vagina, presents a significant health challenge across the globe.
Understanding its symptoms and causes is crucial for early detection and treatment, which can significantly improve outcomes for those affected.
What is Cervical Cancer?
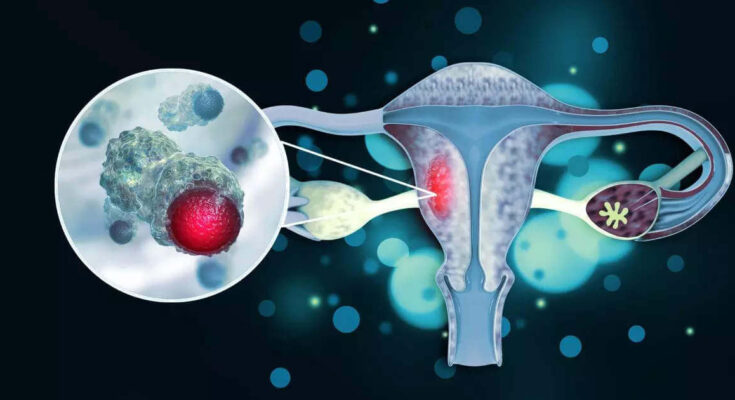
Cervical cancer is a type of cancer that occurs in the cells of the cervix — the lower part of the uterus that connects to the vagina. This disease can affect the deeper tissues of the cervix and may spread to other parts of the body (metastasize), often impacting the lungs, liver, bladder, vagina, and rectum. Despite being a serious medical condition, early detection and effective treatment can significantly improve the prognosis for women with cervical cancer.
Brief Statistics on Cervical Cancer Incidence and Mortality Rates
Cervical cancer was once one of the most common causes of cancer death for American women. However, the incidence and mortality rates of cervical cancer have decreased significantly over the past few decades, thanks to the widespread use of the Pap test (Pap smear) which can detect precancerous conditions of the cervix. According to the World Health Organization (WHO), cervical cancer is the fourth most frequent cancer in women worldwide but varies significantly by region due to differences in access to screening and treatment services. Each year, hundreds of thousands of women globally are diagnosed with cervical cancer, and a significant proportion of these women succumb to the disease, highlighting the importance of preventive measures and early detection.
The Role of Human Papillomavirus (HPV) in Cervical Cancer Development
Human papillomavirus (HPV) plays a pivotal role in the development of almost all cases of cervical cancer. HPV is a common virus that is transmitted through sexual contact. There are many types of HPV, but only a few cause most cases of cervical cancer. Types 16 and 18, in particular, are responsible for approximately 70% of all cases. The body’s immune system typically prevents the virus from doing harm; however, in a small percentage of people, the virus survives for years, contributing to the process that causes some cervical cells to become cancer cells.
Vaccination against HPV has emerged as a powerful tool in the fight against cervical cancer, offering protection against the most dangerous strains of the virus. Alongside regular screening with Pap smears and HPV tests, vaccination significantly reduces the risk of developing cervical cancer.
Understanding cervical cancer, its causes, and preventive measures is crucial for reducing its incidence and mortality rates. Awareness and education about HPV and the importance of regular cervical screenings can save lives through early detection and timely treatment.
Symptoms of Cervical Cancer: Recognizing the Signs for Early Detection
Here, we will explore the symptoms associated with early-stage and advanced cervical cancer, delve into the reasons these symptoms occur, and emphasize the importance of monitoring your body and seeking medical advice.
Early-Stage Cervical Cancer Symptoms (or Lack Thereof)
In its initial stages, cervical cancer may not present any symptoms, making it difficult to detect without regular screening tests, such as Pap smears or HPV tests. This silent progression underscores the importance of routine gynecological exams for all women, especially those over the age of 21 or those who have been sexually active for several years. On occasion, some women may experience subtle signs that could indicate early cervical cancer, including:
- Irregular bleeding: This includes bleeding between regular menstrual periods, after sexual intercourse, or after menopause.
- Unusual vaginal discharge: An increase in quantity, a change in consistency or color, or a presence of a foul odor in vaginal discharge can be an early warning sign.
It’s important to note that these symptoms can also be indicative of conditions other than cervical cancer, making professional medical evaluation essential for a correct diagnosis.
Common Symptoms of Advanced Cervical Cancer
As cervical cancer progresses to more advanced stages, the symptoms become more pronounced and may include:
- Persistent pelvic pain: Unlike the occasional discomfort many women experience during their menstrual cycle, this pain is constant and may intensify over time.
- Pain during intercourse: This symptom, known as dyspareunia, can be a sign of advanced cervical or other types of gynecological cancers.
- Significant changes in urinary and bowel habits: This includes pain during urination, blood in the urine, or alterations in the frequency and consistency of bowel movements.
- Leg pain or swelling: In advanced stages, cancer may spread and cause swelling in the legs due to lymph node blockage.
Explanation of Why These Symptoms Occur
The symptoms of cervical cancer occur as the cancerous cells grow and invade nearby tissues and organs. For example, irregular bleeding and unusual vaginal discharge can result from the growth of cancerous cells on the surface of the cervix, which can lead to irritation or infection. Pain during intercourse, pelvic pain, and changes in urinary and bowel habits can occur as the cancer spreads to surrounding tissues and nerves. Leg pain or swelling happens when cancer spreads to the lymph nodes and disrupts normal fluid drainage, leading to accumulation and swelling.
Importance of Paying Attention to Your Body and Seeking Medical Advice
Being attuned to your body’s signals and seeking medical advice if you notice any changes or symptoms is vital for early detection and treatment of cervical cancer. Early-stage cervical cancer can often be treated successfully with less invasive procedures, and the prognosis is generally favorable when caught early. Regular screening tests, such as Pap smears and HPV tests, are crucial for detecting precancerous conditions or early-stage cervical cancer before symptoms appear.
If you experience any of the symptoms mentioned above, or if something just doesn’t feel right, schedule an appointment with your healthcare provider. It’s essential to have an open and honest conversation about your symptoms and concerns. Remember, early detection saves lives, and paying attention to your body is the first step in taking control of your health.
However, while early-stage cervical cancer may not always present noticeable symptoms, recognizing the signs of advanced cervical cancer and understanding why they occur can empower women to seek timely medical advice. Regular screenings and being proactive about gynecological health are key strategies in the fight against cervical cancer.
Causes and Risk Factors of Cervical Cancer
Understanding the causes and risk factors of cervical cancer is crucial for its prevention and early detection. Cervical cancer begins in the cells lining the cervix—the lower part of the uterus that connects to the vagina. Various factors can contribute to the development of this disease, with the primary cause being infection with certain types of the Human Papillomavirus (HPV).
The Primary Cause: Human Papillomavirus (HPV) Infection
HPV is a group of more than 100 related viruses, some of which are transmitted through sexual contact. High-risk HPV types are responsible for the majority of cervical cancer cases. HPV infection is common, and in most cases, the body’s immune system clears the infection on its own. However, in some individuals, the infection persists and leads to the transformation of normal cervical cells into precancerous lesions, which can eventually develop into cancer.
Other Risk Factors Contributing to Cervical Cancer
In addition to HPV infection, several other factors can increase the risk of developing cervical cancer. These include:
- Smoking: Women who smoke are about twice as likely as non-smokers to get cervical cancer. Smoking can weaken the immune system, making it harder for the body to fight off HPV infections.
- Having a Weakened Immune System: Individuals with weakened immune systems, such as those with HIV/AIDS or those taking immunosuppressant drugs, are at a higher risk of developing cervical cancer because their bodies are less able to fight off HPV.
- Long-term Use of Birth Control Pills: Research suggests that the risk of cervical cancer increases the longer a woman takes birth control pills, but the risk decreases after stopping them.
- Having Multiple Sexual Partners: Having multiple sexual partners or having sex with someone who has had multiple partners increases the risk of HPV infection.
- Early Sexual Activity: Engaging in sexual activity at a young age increases the risk of HPV infection because younger individuals may have a less developed cervical lining.
- Genetic Factors and Family History: Women with a family history of cervical cancer or certain genetic conditions may have a higher risk of developing the disease.
Understanding these risk factors is essential for prevention and early detection of cervical cancer. Regular screening tests, such as the Pap smear and HPV test, can help detect precancerous conditions of the cervix so they can be treated before cancer develops. Vaccination against HPV is also an effective way to reduce the risk of cervical cancer.
Preventing Cervical Cancer: Strategies and Recommendations
Cervical cancer prevention is crucial for women’s health worldwide. With advancements in medical research, there are now effective strategies to significantly reduce the risk of developing cervical cancer. These include HPV vaccination, regular cervical screening tests, and adopting healthy lifestyle modifications. Understanding the efficacy and recommendations for these preventive measures can empower women to take control of their health.
HPV Vaccination: Efficacy and Recommendations
The Human Papillomavirus (HPV) vaccine is a groundbreaking tool in the fight against cervical cancer. HPV is the most common viral infection of the reproductive tract and the main cause of cervical cancer. The vaccine offers strong protection against the types of HPV that most commonly cause cervical cancer.
Efficacy: Clinical trials and real-world studies have shown that the HPV vaccine is highly effective in preventing infections with HPV types that cause the majority of cervical cancers. The vaccine is most effective when administered before individuals become sexually active, as it prevents HPV infection but does not treat existing infections.
Recommendations: It is recommended that both girls and boys receive the HPV vaccine at ages 11 or 12, although vaccination can start as early as age 9. Catch-up vaccines are also recommended for males and females through age 26 if they did not get vaccinated when they were younger. Adults aged 27 through 45 years should consult with their healthcare provider about the potential benefits of receiving the vaccine.
Regular Cervical Screening Tests: Purpose and Frequency
Cervical screening tests, including the Pap test (or Pap smear) and the HPV DNA test, play a vital role in preventing cervical cancer. These tests help identify precancerous changes in the cervix that, if left untreated, could develop into cancer.
Purpose: The Pap test screens for precancerous or cancerous cells on the cervix. The HPV DNA test detects the presence of high-risk HPV types in cervical cells. Together, these tests are instrumental in early detection, which is key to preventing the progression to cervical cancer.
Frequency: The American Cancer Society recommends that women begin cervical cancer screening at age 25 and continue through age 65. Women aged 25 to 65 should have a primary HPV test every five years. If primary HPV testing is not available, a co-test (an HPV test with a Pap test) every five years or a Pap test alone every three years are acceptable alternatives.
Lifestyle Modifications to Reduce Risk
Adopting healthy lifestyle choices can also help reduce the risk of developing cervical cancer. Key modifications include:
- Smoking Cessation: Smoking is associated with an increased risk of cervical cancer. Quitting smoking can help lower this risk.
- Safe Sex Practices: Using condoms and limiting the number of sexual partners can reduce the risk of HPV infection, which is a major risk factor for cervical cancer.
- Diet and Exercise: Maintaining a healthy diet and regular exercise regimen can support overall health and potentially reduce cancer risk.
Preventing cervical cancer involves a multifaceted approach that includes getting vaccinated against HPV, undergoing regular screening tests, and adopting healthy lifestyle habits. By following these recommendations, women can significantly reduce their risk of developing cervical cancer and ensure early detection for the best possible outcome. Engaging in open conversations with healthcare providers about cervical cancer prevention is an important step in taking charge of one’s health.
Diagnosing Cervical Cancer: A Step-by-Step Guide
Cervical cancer, when detected early, can be treated effectively, highlighting the importance of regular screenings and awareness of the diagnostic process. This article outlines the crucial steps involved in diagnosing cervical cancer, emphasizing the significance of early detection in enhancing treatment outcomes.
1. Pap Smear
The Pap smear, also known as a Pap test, is a primary and critical step in the early detection of cervical cancer. During this procedure, cells from the cervix are gently collected and then examined under a microscope to identify any precancerous or cancerous changes. Women are recommended to start undergoing Pap smears at the age of 21 and continue at regular intervals. This test plays a pivotal role in detecting cervical cancer at an early stage, even before symptoms appear, making it an essential tool in cervical cancer prevention.
2. HPV DNA Test
The Human Papillomavirus (HPV) DNA test is another vital diagnostic tool. It involves testing cells collected from the cervix for the presence of any of the types of HPV most likely to lead to cervical cancer. This test can be done in conjunction with the Pap smear or when Pap test results are unclear. It’s particularly recommended for women over the age of 30 as part of their routine screening. Identifying high-risk HPV types early can guide follow-up and treatment, if necessary.
3. Colposcopy
If the results of a Pap smear or HPV DNA test indicate abnormal changes, a colposcopy may be recommended. This procedure allows the doctor to closely examine the cervix, vagina, and vulva for signs of disease. Using a special instrument called a colposcope, which magnifies the cells of the cervix, the doctor can spot abnormal areas and take samples for further testing if necessary. It’s a critical step for confirming the presence of precancerous or cancerous cells.
4. Biopsy
A biopsy is often performed during a colposcopy to confirm a diagnosis of cervical cancer. In this procedure, a small sample of tissue is taken from the cervix and examined for cancer cells. There are different types of biopsies, such as a punch biopsy, endocervical curettage, or cone biopsy, each designed to remove tissue for analysis in a way that best suits the location and suspected type of the abnormal cells.
The Importance of Early Diagnosis
Early diagnosis of cervical cancer plays a fundamental role in improving treatment outcomes. When detected at an early stage, cervical cancer is one of the most successfully treatable forms of cancer. Early detection means that treatment can be started sooner, which can significantly increase the chances of a successful outcome and reduce the likelihood of the cancer spreading to other parts of the body.
Regular screenings through Pap smears and HPV DNA tests, followed by timely colposcopy and biopsy if needed, are key to catching cervical cancer early. This highlights the importance of adhering to recommended screening schedules and paying attention to any follow-up procedures advised by healthcare providers.
By understanding and participating in the diagnostic process, women can take an active role in their health care and significantly improve their chances of preventing or successfully treating cervical cancer. Regular communication with healthcare providers, staying informed about when to undergo screenings, and understanding the steps involved in diagnosing cervical cancer are crucial components of women’s health and well-being.
Treatment Options for Cervical Cancer
Cervical cancer, a type of cancer that occurs in the cells of the cervix — the lower part of the uterus that connects to the vagina, presents a spectrum of treatment options tailored to the cancer’s stage, overall health, and personal preferences of the individual. Advances in medical science have broadened the treatment modalities, incorporating traditional methods alongside innovative therapies such as targeted therapy and immunotherapy, especially in advanced cases. This article explores the array of treatment options available for cervical cancer, emphasizing the role of targeted therapy and immunotherapy.
Treatment Modalities Based on Stages
The treatment for cervical cancer is stage-dependent, with each stage offering different modalities aimed at the best possible outcome. Here’s a breakdown:
Early Stages (0, I, and II)
- Surgery is often the first line of treatment, ranging from simple procedures like LEEP (Loop Electrosurgical Excision Procedure) or cone biopsy to more extensive ones such as a hysterectomy, where part or all of the uterus is removed.
- Radiation Therapy may be used alone or in combination with chemotherapy, especially if surgical options are not viable or if there is a higher risk of cancer spreading.
- Chemotherapy is typically used in conjunction with radiation therapy to enhance its effectiveness in these stages.
Advanced Stages (III and IV)
- Chemoradiation, a combination of chemotherapy and radiation therapy, is a standard approach, aiming to control the spread of the disease and alleviate symptoms.
- Palliative Care focuses on relieving symptoms and improving quality of life for those with more advanced cancer.
The Role of Targeted Therapy and Immunotherapy in Advanced Cases
In recent years, targeted therapy and immunotherapy have emerged as significant players in the treatment of advanced cervical cancer. These treatments represent a shift towards more personalized medicine, targeting specific cancer characteristics and the body’s immune response.
- Targeted Therapy works by targeting specific genes, proteins, or the tissue environment that contributes to cancer growth and survival. For example, Bevacizumab (Avastin) is a targeted therapy approved for cervical cancer that blocks the growth of new blood vessels to the tumor, effectively starving the cancer cells.
- Immunotherapy harnesses the power of the body’s immune system to fight cancer. Drugs like Pembrolizumab (Keytruda) have been approved for advanced cervical cancer, especially for cases that are not responsive to other treatments. These drugs work by helping the immune system recognize and attack cancer cells more effectively.
Both targeted therapy and immunotherapy offer hope for patients with advanced cervical cancer, often with fewer side effects compared to traditional treatments. They have been instrumental in treating cases where cancer has recurred or spread too far to be managed by conventional methods alone.
However, the treatment landscape for cervical cancer is dynamic, with options ranging from surgery and chemoradiation to cutting-edge therapies like targeted therapy and immunotherapy. The choice of treatment is highly individualized, based on the cancer’s stage, specific characteristics, and the patient’s overall health and treatment preferences. Advances in medical research continue to provide new hope for more effective and less invasive cervical cancer treatments, improving outcomes and quality of life for patients.
Living with Cervical Cancer
Living with cervical cancer presents numerous challenges, not only in battling the disease itself but also in coping with the symptoms and side effects of its treatment. This journey, however, can be navigated more smoothly with the right support systems in place, including counseling and cancer support groups. The following section delves into these aspects, providing valuable insights for those affected by cervical cancer.
Managing Symptoms and Side Effects of Treatment
Treatment for cervical cancer, such as chemotherapy, radiation therapy, and surgery, can lead to a range of side effects. These may include fatigue, nausea, pain, and changes in sexual health, among others. Managing these symptoms effectively is crucial to improving quality of life during treatment. Here are some strategies:
- Medical Interventions: Always discuss your symptoms with your healthcare provider. They can offer medications or other treatments to alleviate side effects like nausea or pain.
- Lifestyle Adjustments: Simple changes in diet and exercise can make a significant difference. For instance, small, frequent meals might help with nausea, and gentle exercise can boost energy levels.
- Holistic Therapies: Complementary therapies such as yoga, meditation, and acupuncture have been found to help some patients manage symptoms and reduce stress.
Support Systems: Counseling and Cancer Support Groups
Navigating the emotional and psychological toll of cervical cancer is as important as managing physical symptoms. Counseling and support groups offer invaluable resources:
- Counseling: Professional counselors or therapists who specialize in cancer care can provide individualized support, helping you process your emotions and develop strategies for coping with the disease. This can be through one-on-one sessions, family therapy, or couples counseling, depending on your needs.
- Cancer Support Groups: These groups offer a sense of community and understanding that is hard to find elsewhere. Sharing experiences with others who are in a similar situation can provide comfort, reduce feelings of isolation, and offer practical advice on dealing with treatment and its side effects.
Living with cervical cancer is a profoundly challenging experience, but with the right management strategies and support systems, it can be faced with strength and resilience. It’s essential to reach out for help and to utilize the resources available, from medical interventions and lifestyle adjustments to counseling and support groups. Remember, you are not alone on this journey, and there is support available every step of the way.
Incorporating these strategies into your care plan can help mitigate the impacts of cervical cancer and its treatment, allowing for a focus on healing and recovery. Always communicate openly with your healthcare team about your symptoms and the emotional challenges you’re facing—they’re there to support you in every aspect of your treatment and recovery.
Conclusion
In summarizing the critical insights into cervical cancer, it’s paramount to underscore the significance of recognizing its symptoms and understanding the underlying causes. Awareness is the first step towards prevention, and knowledge of these aspects can dramatically alter the course of one’s health trajectory. Regular screenings, such as Pap smears and HPV tests, are instrumental in catching precancerous conditions and cervical cancer in its early stages, when it is most treatable. Vaccination against the human papillomavirus (HPV), a leading cause of cervical cancer, offers another powerful tool in our arsenal against this disease, providing a layer of protection that cannot be overlooked.
Advancements in the treatment of cervical cancer continue to offer hope, showcasing the remarkable progress science has made in battling this condition. From innovative surgical techniques to targeted therapy and immunotherapy, the options for treatment are expanding, improving the outlook for those diagnosed. Yet, the cornerstone of combating cervical cancer remains early detection. It cannot be overstressed how crucial early diagnosis is; it significantly improves treatment success rates and increases the chances of a full recovery.
As we move forward, let us embrace the advancements in medical science with optimism while also committing to the proactive measures within our grasp—regular screenings and vaccinations. By doing so, we not only protect ourselves but also contribute to the broader effort of reducing the incidence of cervical cancer globally. Let this be a call to action for all individuals to prioritize their health, for early detection and prevention are key to turning the tide against cervical cancer.