Central Sleep Apnea Treatment: Sleep is a crucial component of our daily lives, impacting our health, mood, and overall well-being. Among the disorders that disrupt sleep, Central Sleep Apnea (CSA) stands out due to its unique causes and treatment strategies.
This article aims to provide an in-depth exploration of CSA, detailing its diagnosis, implications, and the most effective treatment options available.
What is Central Sleep Apnea?
Central Sleep Apnea (CSA) is a less common form of sleep apnea, a disorder characterized by brief interruptions in breathing during sleep. Unlike Obstructive Sleep Apnea, which results from a physical blockage in the airway, CSA occurs because the brain fails to send proper signals to the muscles that control breathing. This condition leads to periodic pauses in breathing, which can significantly impact sleep quality and overall health.
Symptoms of Central Sleep Apnea
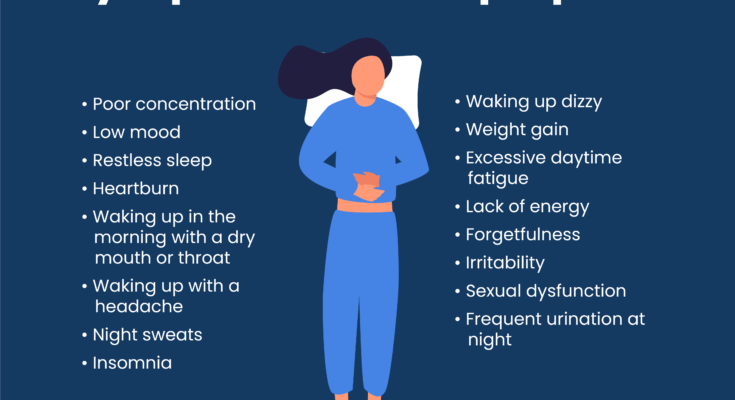
The symptoms of Central Sleep Apnea can be subtle or significant, and they often overlap with those of other sleep disorders, making diagnosis challenging. Key symptoms include:
- Interruptions in breathing during sleep, often noted by a partner
- Sudden awakenings with shortness of breath
- Insomnia or difficulty staying asleep
- Excessive daytime sleepiness
- Morning headaches
- Difficulty concentrating during the day
- Mood changes, such as depression or anxiety
Causes and Risk Factors Associated with CSA
The causes of CSA can vary, ranging from medical conditions that affect the brainstem, which controls breathing, to high altitude exposure. Key causes and risk factors include:
- Heart failure and atrial fibrillation
- Stroke or brain tumor
- Use of certain medications, including opioids
- Living or sleeping at high altitudes
- Age, with a higher prevalence in older adults
- Being male, as men are more frequently diagnosed with CSA
How CSA Affects Sleep and Overall Health
Central Sleep Apnea can significantly disrupt sleep architecture, leading to fragmented sleep and reduced time spent in restorative sleep stages. This fragmentation can result in excessive daytime sleepiness, impaired cognitive function, and an increased risk of cardiovascular issues such as hypertension, heart attack, and stroke. Moreover, the chronic sleep disruption associated with CSA can contribute to mood disorders, including depression and anxiety, further impacting overall health and quality of life.
Understanding CSA, recognizing its symptoms, and identifying its causes and risk factors are crucial steps in managing its effects on sleep and health. Early diagnosis and treatment can mitigate these impacts, improving sleep quality and overall well-being.
Diagnosis of Central Sleep Apnea (CSA)
Understanding the diagnosis process of Central Sleep Apnea (CSA) is crucial for individuals experiencing sleep disturbances. CSA is a sleep disorder where the brain temporarily stops sending signals to the muscles that control breathing, leading to interrupted sleep. Diagnosing CSA involves several steps to ensure accurate detection and effective management. Here’s a comprehensive look at the process:
Initial Consultation and Medical History Review
The journey towards diagnosing CSA starts with an initial consultation. During this session, a healthcare provider will review the patient’s medical history and symptoms. This review is vital as it helps in identifying potential risk factors or underlying conditions contributing to CSA. Patients are encouraged to discuss all symptoms, no matter how minor they may seem, including snoring, daytime fatigue, and observed breathing interruptions during sleep.
Physical Examination and Identifying Symptoms
Following the medical history review, a physical examination is conducted. The healthcare provider will check for physical signs that may indicate CSA, such as abnormalities in the throat structure, obesity, or other signs of conditions that could contribute to sleep apnea. Identifying symptoms and understanding their impact on the patient’s life are crucial steps in diagnosing CSA.
Sleep Studies (Polysomnography) and Their Role in Diagnosing CSA
A key component in diagnosing CSA is the sleep study, known as polysomnography. This test is conducted overnight in a sleep center or hospital. It monitors the patient’s brain waves, blood oxygen level, heart rate, breathing patterns, and eye and leg movements during sleep. Polysomnography provides a comprehensive overview of the patient’s sleep phases and is instrumental in confirming the presence of CSA by capturing episodes where breathing stops or becomes shallow due to lack of respiratory effort.
Challenges in Diagnosing CSA and the Importance of Specialized Sleep Centers
Diagnosing CSA can present challenges. Symptoms of CSA often overlap with those of other sleep disorders, making it difficult to pinpoint the exact cause of sleep disturbances. Furthermore, the intermittent nature of breathing interruptions can make CSA less apparent without thorough monitoring. This is why specialized sleep centers play a critical role in the diagnosis process. These centers are equipped with the necessary technology and expertise to accurately diagnose CSA, distinguishing it from other sleep disorders and ensuring patients receive the most effective treatment.
The diagnosis of Central Sleep Apnea is a meticulous process that involves a combination of patient history review, physical examination, and advanced sleep studies. Despite the challenges in diagnosing CSA, the involvement of specialized sleep centers enhances the accuracy of diagnoses, paving the way for targeted treatment strategies. Understanding the steps leading to a CSA diagnosis can empower patients and encourage them to seek the necessary medical attention for their sleep-related issues.
Treatment Options for Central Sleep Apnea (CSA)
The primary goals for treating CSA include restoring regular breathing during sleep, improving sleep quality, and alleviating symptoms. This often involves a combination of non-invasive and, in more severe cases, invasive treatment options. Creating a personalized treatment plan is crucial, taking into account the specific needs and medical history of the patient.
Non-invasive Treatment Options
- Positive Airway Pressure Devices: Devices such as Continuous Positive Airway Pressure (CPAP) and Bilevel Positive Airway Pressure (BiPAP) are cornerstone treatments for CSA. They work by delivering air pressure through a mask to keep the airways open during sleep.
- Adaptive Servo-Ventilation (ASV): ASV is an advanced form of airway pressure therapy that adjusts the pressure based on the detection of breathing abnormalities, providing a more tailored approach for individuals with CSA.
- Oxygen Supplementation: For some patients, supplemental oxygen during sleep can help improve oxygen levels in the blood, reducing the severity of breathing pauses.
- Lifestyle Changes and Managing Underlying Conditions: Addressing factors such as obesity, heart conditions, or the use of certain medications can significantly impact the severity of CSA. Lifestyle modifications, such as weight loss, reducing alcohol consumption, and optimizing the management of underlying health issues, are often recommended.
Invasive Treatment Options (If Necessary)
- Surgery: Surgery is rarely required but may be considered in cases where anatomical issues contribute to CSA, such as correcting heart or neuromuscular disorders.
- Implantable Devices: Devices like phrenic nerve stimulators, which help stimulate breathing by activating the diaphragm, may be an option for patients who do not respond to other treatments.
Importance of Personalized Treatment Plans
Every individual with CSA has a unique set of circumstances and health considerations, making personalized treatment plans essential. Working closely with a healthcare provider to monitor the effectiveness of treatment, adjusting strategies as needed, and considering both non-invasive and invasive options can lead to the best outcomes. It’s crucial for patients to have an active role in their treatment planning, ensuring that choices align with their lifestyle, preferences, and overall health goals.
However, treating Central Sleep Apnea effectively requires a comprehensive approach that includes a combination of non-invasive treatments, lifestyle adjustments, and, in some cases, invasive procedures. The key to successful management lies in a personalized treatment plan, developed and monitored by healthcare professionals, tailored to meet the specific needs of each patient.
Managing Central Sleep Apnea: Effective Strategies and Professional Guidance
Managing CSA effectively requires a comprehensive approach that includes lifestyle modifications, professional healthcare guidance, and ongoing monitoring. Here’s how you can manage CSA to improve your sleep quality and overall health.
Lifestyle Modifications and Their Impact on CSA Management
Lifestyle changes play a pivotal role in managing Central Sleep Apnea. These modifications can significantly improve your condition and enhance the effectiveness of other treatments. Here are key lifestyle changes that can positively impact CSA:
- Weight Management: Maintaining a healthy weight can reduce the severity of CSA. Excess weight, especially around the neck, can affect breathing patterns and exacerbate sleep apnea symptoms.
- Avoiding Alcohol and Sleeping Pills: Alcohol and certain medications can relax the muscles in your throat, interfering with breathing. Avoiding these substances, especially before bedtime, can help manage CSA symptoms.
- Sleep Position: For some people, sleeping on the side instead of the back can reduce episodes of sleep apnea. It’s worth experimenting with different positions to find one that reduces your symptoms.
- Heart Health: Since CSA can be associated with heart conditions, managing heart health through a balanced diet, regular exercise, and medication adherence is crucial.
The Role of Healthcare Providers in Managing CSA
The guidance of healthcare providers is indispensable in managing Central Sleep Apnea. A sleep specialist can offer insights into the most effective treatments based on your specific condition. Treatment options may include:
- Positive Airway Pressure Devices: Devices such as CPAP (Continuous Positive Airway Pressure) are commonly used to treat CSA by delivering air pressure through a mask to help keep your airway open while you sleep.
- Adaptive Servo-Ventilation (ASV): This is a newer form of air pressure therapy that adjusts the pressure based on your breathing patterns, particularly effective for certain types of CSA.
- Oxygen Supplementation: In some cases, additional oxygen during sleep can help ensure the body gets the oxygen it needs.
- Medications: Although less common, medications can sometimes be used to stimulate breathing.
Monitoring and Adjusting Treatment Over Time
Managing CSA is an ongoing process that requires regular monitoring and adjustments to treatment plans. Follow-up appointments with your healthcare provider are essential to assess the effectiveness of treatments and make necessary adjustments. Keeping a sleep diary and using home monitoring devices can also provide valuable insights into your sleep patterns and the quality of your sleep. It’s important to communicate any changes in your symptoms or concerns with your healthcare provider to ensure your treatment remains effective over time.
However, managing Central Sleep Apnea is a multifaceted approach that involves lifestyle changes, professional healthcare guidance, and ongoing monitoring. By adhering to these strategies, individuals with CSA can achieve better sleep quality and improve their overall health. Always consult with a healthcare provider for a personalized treatment plan that addresses your specific needs.
Advances in Central Sleep Apnea Treatment
Advances in technology and treatment options have paved the way for significant improvements in the management and understanding of CSA. This article explores the recent advancements in CSA treatment, highlights ongoing research, and discusses future directions that hold promise for those affected by this challenging condition.
Technological Innovations in CSA Management
The landscape of CSA treatment has been transformed by technological innovations designed to enhance patient comfort and treatment efficacy. One of the most significant advancements is the development of adaptive servo-ventilation (ASV) devices. These sophisticated machines are tailored to the individual needs of CSA patients, adjusting air pressure in real-time to match the patient’s breathing patterns. ASV devices have shown remarkable success in improving sleep quality and overall quality of life for those with CSA.
Moreover, the integration of digital health platforms into CSA management has enabled remote monitoring and personalized care like never before. Patients can now use wearable devices that track sleep patterns, oxygen levels, and heart rate, providing valuable data that can be analyzed by healthcare providers to adjust treatment plans promptly. This real-time data collection facilitates a more dynamic approach to managing CSA, allowing for treatments to be tailored more closely to the patient’s current needs.
Research and Future Directions in CSA Treatment
Research into CSA is expanding, with scientists exploring various avenues to better understand and treat this condition. One promising area of research focuses on the underlying neurological mechanisms that cause CSA. By unraveling the complex interactions between the brain and the respiratory system, researchers hope to develop new therapeutic interventions that target the root causes of CSA.
Gene therapy and pharmacological treatments are also being investigated as potential future treatments for CSA. These approaches aim to correct or mitigate the physiological and neurological abnormalities contributing to CSA, offering hope for more effective and long-lasting solutions.
In addition, clinical trials are underway to evaluate the effectiveness of novel treatment modalities, including electrical stimulation of the diaphragm and other neural pathways involved in breathing. These innovative treatments could offer alternatives for patients who do not respond well to current therapies.
Embracing a Future with Improved CSA Management
The advances in technology, combined with ongoing research, promise a future where CSA can be managed more effectively and with greater personalization. As we continue to explore new treatments and technologies, the goal remains to enhance the quality of life for individuals living with CSA, offering them not just a good night’s sleep but also improved overall health and well-being.
The journey towards better understanding and treating CSA is ongoing, and with each technological breakthrough and research milestone, we move closer to a world where this sleep disorder can be effectively managed or perhaps even cured. For those affected by CSA, these advancements represent not just hope for better sleep, but a brighter, healthier future.
Conclusion:
The importance of seeking treatment for sleep disorders cannot be overstated. Untreated sleep disorders, including CSA, can lead to a host of health issues, such as cardiovascular problems, fatigue, and decreased cognitive function, impacting daily life and overall well-being. Moreover, addressing sleep disorders can significantly improve life quality, enhancing both physical health and mental well-being.
If you’re experiencing symptoms that may indicate CSA or any other sleep disorder, it’s imperative to consult with healthcare providers. Early consultation can lead to timely diagnosis and effective treatment, paving the way for better sleep, improved health, and a more vibrant life. Healthcare professionals can offer comprehensive guidance tailored to your specific needs, ensuring you receive the most appropriate and effective care.
Remember, acknowledging the need for help and taking the first step towards seeking treatment is a sign of strength. Let’s prioritize our health and well-being by paying attention to our sleep patterns and consulting healthcare providers when concerns arise. Together, we can tackle sleep disorders like CSA, ensuring a healthier, more restful future for everyone.